RANGE OF MOTION OF ALL JOINTS
Table of Contents
What is a Range of Motion(ROM)?
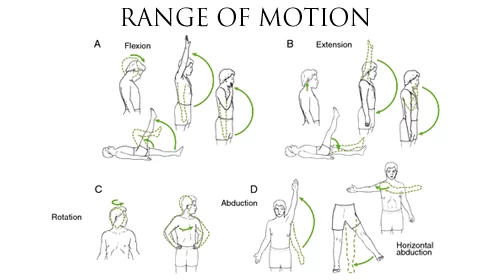
Range of motion (ROM) is a measurement of the distance and direction a joint can move to its full potential. A joint is a location in the body where bones connect. Most of them are constructed to allow movement in predetermined directions. The amount of movement through a normal range of motion is commonly measured in degrees using an instrument called a Goniometer.
Each joint has different ranges of motion for each type of movement it can perform. There are a few joints that do not support movement, such as in the skull.

Common joint movements include flexion, extension, abduction, and adduction. Extension is a physical position that decreases the angle between the bones of the limb at a joint. It occurs when muscles contract and bones move the joint into a bent position. The opposite movement, flexion, bends the joint so that the joint angle shortens.
ALL JOINTS OF NORMAL RANGE MOTION :
Although there is variability among various individuals, the following are generally accepted values for a normal ROM in each individual joint as measured in degrees. Physical therapists and exercise physiologists measure an individual’s range of motion and compare it to these normal values.
- Hip :
Flexion: 0 to 125 degrees
Extension: 115 to 0 degrees
Hyperextension (straightening beyond normal range) :- 0 to 15 degrees
Abduction (moving away from the central axis of the body) :- 0 to 45 degrees
Adduction (moving towards the central axis of the body) :- 45 to 0 degrees
Lateral rotation (rotation away from the center of the body) :- 0 to 45 degrees
Medial rotation (rotation towards the center of the body) :- 0 to 45 degrees
- Knee :

Flexion: 0 to 135-145 degrees
Extension: 135-145 to 0 degrees
- Ankle :
Plantar flexion (movement downward): 0 to 50 degrees
Dorsi-flexion (movement upward): 0 to 20 degrees
- Foot :
Inversion (turned inward): 0 to 35 degrees
Eversion (turned outward): 0 to 25 degrees
- Metatarsophalangeal Joint of the Foot:
Flexion: 0 to 30 degrees
Extension: 0 to 80 degrees
- Interphalangeal Joint of the Toe:
Flexion: 0 to 50 degrees
Extension: 50 to 0 degrees
- Shoulder :
Flexion: 0 to 180 degrees
Extension: 0 to 50 degrees
Abduction: 0 to 90 degrees
Adduction: 90 to 0 degrees
Lateral rotation: 0 to 90 degrees
Medial rotation: 0 to 90 degrees
- Elbow :
Flexion: 0 to 160 degrees
Extension: 145 to 0 degrees
Pronation (rotation inward): 0 to 90 degrees
Supination (rotation outward): 0 to 90 degrees
- Wrist :
Flexion: 0 to 90 degrees
Extension: 0 to 70 degrees
Abduction: 0 to 25 degrees
Adduction: 0 to 65 degrees
- Metacarpophalangeal (MCP) :
Abduction: 0 to 25 degrees
Adduction: 20 to 0 degrees
Flexion: 0 to 90 degrees
Extension: 0 to 30 degrees
- Interphalangeal Proximal (PIP) Joint of the Finger :

Flexion: 0 to 120 degrees
Extension: 120 to 0 degrees
Interphalangeal Distal (DIP) Joint of the Finger :
Flexion: 0 to 80 degrees
Extension: 80 to 0 degrees
- Metacarpophalangeal Joint of the Thumb :
Abduction: 0 to 50 degrees
Adduction: 40 to 0 degrees
Flexion: 0 to 70 degrees
Extension: 60 to 0 degrees
- Interphalangeal Joint of the Thumb :
Flexion: 0 to 90 degrees
Extension: 90 to 0 degrees
HOW RANGE OF MOTION IS MEASURED?
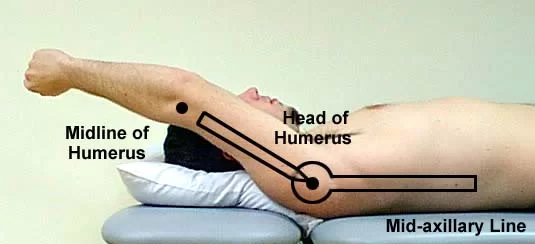
The range of motion is measured by your physical therapist using a device called a goniometer. A goniometer is a metal or plastic handheld device with two arms. Numbers representing angular distance are on the device, much like a protractor. Your physical therapist lines up the arms along your body, and then he or she can move your body in specific directions and measure the amount of motion that occurs.
Measuring ROM is usually a painless procedure. There are some instances after surgery or injury where measuring the ROM may be painful, but the pain is usually short-lived and only occurs during the measurement.
In general, there are three types of ROM that are measured. They are passive (PROM), active-assistive (AAROM), and active (AROM).
- Passive Range of Motion :
Passive ROM occurs around a joint if you are not using your muscles to move. Someone else, like your physical therapist, manually moves your body while you relax. A machine may also be used to provide passive ROM. For example, after knee replacement surgery, you may not be able to use your muscles to move the knee. Your physical therapist may bend and straighten your knee for you, passively moving your leg. Occasionally, a device called continuous passive motion (CPM) is used to provide passive ROM.
Passive ROM is usually used during the initial healing phase after surgery or injury. If paralysis prevents your body from moving normally, passive ROM may also be used to prevent contractures or skin pressure ulcers.
- Active-Assistive Range of Motion :
Active-assistive ROM occurs when you are able to move your injured body part, but you may require some help to move to ensure further injury or damage does not occur. The assistance that helps move your body can come from you or from another person. It may also come from a mechanical device or machine.
An example of AAROM is after shoulder rotator cuff surgery. You may be allowed to move your arm, but another person may assist your arm during a motion to help limit the amount of stress that may occur. Active-assistive ROM is typically used after injury or surgery when some healing has occurred and your muscle can contract, but protection is still required to prevent damage to your healing body part.
- Active Range of Motion :
Active ROM occurs when you use your muscles to help move your body part. This requires no other person or device to help you move. Active ROM is used when you are able to start moving independently after injury or surgery, and little or no protection from further injury is needed. Strengthening exercises are a form of active ROM.
Be sure to speak with your physical therapist or doctor to understand what type of ROM is necessary if you are injured or have had surgery.
Understanding what range of motion is and how it is used in physical therapy can help you become better informed about your course of physical therapy and have a positive physical therapy experience. Working towards normal ROM can help ensure a safe and rapid return to optimum functional mobility.
FACTORS THAT AFFECT RANGE OF MOTION :
There are numerous influences—inherent and situational—that can affect your ROM. Some of the things that you can’t control and that you are born with include:
- The type of joint, as some joints aren’t meant to move a lot
- The internal resistance within a joint
- Bony structures which limit movement
- The elasticity of muscle tissue, for instance, the muscle tissue that is scarred due to a previous injury is not very elastic
- The muscle’s ability to relax and contract to achieve the greatest range of movement
- Another factor that you can’t control is how old you are. One study examined the effects of age and sex on joint ranges of motion and found that older participants showed smaller ROMs than their younger counterparts. In one case, the difference in ROM was 44.9 percent for the eversion and inversion of the foot. What’s more, older subjects needed more time to reach a full range of motion.
As for gender, it was found to have a significant effect on ROM. Men had smaller ROMs than women in some areas, with the greatest difference, 29.7 percent, occurring in the hand.
These differences in age and sex were found to affect specific joints and motions, which could be explained by the differences in anatomy and the frequency that the joints are used in activities between the groups.
CAUSES & TREATMENT FOR LIMITED RANGE OF MOTION :
Limited range of motion is a term used when a joint has a reduction in its ability to move. This can be due to injuries to the soft tissues surrounding a joint. It may also be caused by diseases such as osteoarthritis, rheumatoid arthritis, or other types of arthritis.
Regaining the range of motion in a joint is one of the first phases of injury rehabilitation. Physiotherapists often prescribe specific ROM exercises for each joint.
Each joint has a normal ROM, while each person has a different amount of ability to achieve it. Joints maintain a balanced range of motion by regular use and stretching of the surrounding soft tissues (muscles, tendons, and ligaments). Just 10 minutes of stretching three times a week can help improve the range of motion.


Continuous Passive Movement Machine (CPM) is also used to Maintain and improve the Range of Motion, Mostly physiotherapists use this machine post-operative. All joint CPM machines and knee joint stiffness CPM machines are highly used.
A study found that small gains in ROM might be made by applying heat while stretching. In healthy individuals, those who were complaining of tight muscles saw a slight improvement in range of motion with heat and stretching compared to those who only stretched.
TYPES OF EXERCISE OF ROM :
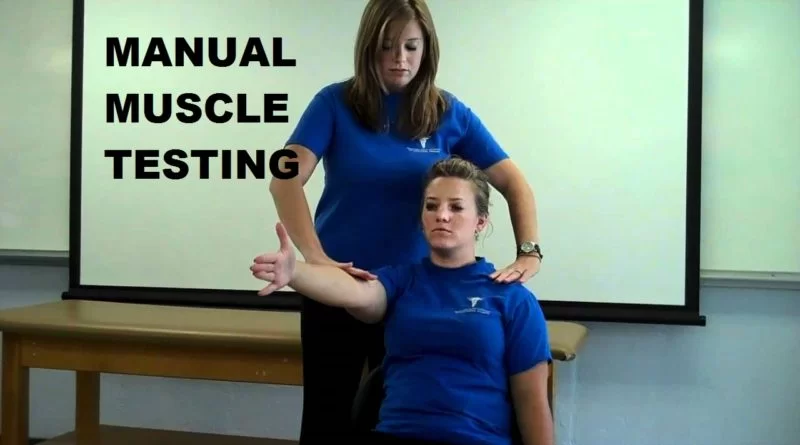
Physiotherapists often prescribe specific ROM exercises for each joint. These exercises aim to gently increase the range of motion with attention to the pain, stiffness, and swelling that may be present. There are three types of range-of-motion exercises:
Active range-of-motion: You perform these exercises without assistance.
Active assistive range-of-motion: The therapist helps the patient do these exercises. This may be done if the muscles are weak or when the movement causes discomfort.
Passive range-of-motion: The therapist or equipment moves the joint through the range of motion without any effort from the patient.
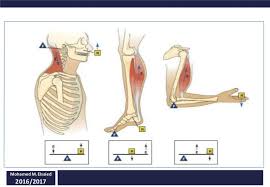
- Strength and conditioning: Many exercises aim to improve muscle strength may be increased with progressive resistive exercise. When a muscle is very weak, gravity alone is sufficient resistance. When muscle strength becomes fair, additional manual or mechanical resistance (eg, weights, spring tension) is added.
General conditioning exercises combine various exercises to treat the effects of debilitation, prolonged bed rest, or immobilization. The goals are to reestablish hemodynamic balance, increase cardio-respiratory capacity and endurance, and maintain range of motion and muscle strength.
For the elderly, the purpose of these exercises is both to strengthen muscles enough to function normally and possibly to regain normal strength for age.
- Proprioceptive neuromuscular facilitation :
This technique helps promote neuromuscular activity in patients who have upper motor neuron damage with spasticity; it enables them to feel muscle contraction and helps maintain the affected joint’s range of motion. For example, applying strong resistance to the left elbow flexor (biceps) of patients with right hemiplegia causes the hemiplegic biceps to contract, flexing the right elbow.
- Co-ordination exercises :
These task-oriented exercises improve motor skills by repeating a movement that works more than one joint and muscle simultaneously (eg, picking up an object, or touching a body part).
- Ambulation exercises :
Before proceeding to ambulation exercises, patients must be able to balance in a standing position. Balancing exercise is usually done using parallel bars with a therapist standing in front of or directly behind a patient. While holding the bars, patients shift weight from side to side and from forward to backward. Once patients can balance safely, they can proceed to ambulation exercises.
As soon as patients can walk safely on level surfaces, they can start training to climb stairs or to step over curbs if either skill is needed. Patients who use walkers must learn special techniques for climbing stairs and stepping over curbs. When climbing stairs, ascent starts with the better leg, and descent starts with the affected leg (ie, good leads up; bad leads down). Before patients are discharged, the social worker or physical therapist should arrange to have secure handrails installed along all stairs in the patients’ homes.
- Transfer training :
Patients who cannot transfer independently from bed to chair, chair to commode, or chair to a standing position usually require attendants 24 h/day. Adjusting the heights of commodes and chairs may help. Sometimes assistive devices are useful; eg, people who have difficulty standing from a seated position may benefit from a chair with a raised seat or a self-lifting chair.





142 Comments