Odontoid Fracture
Table of Contents
Definition
An odontoid fracture, also known as a dens fracture or a type II odontoid fracture, is a specific type of fracture that occurs at the base of the skull in the upper cervical spine. The odontoid process, or dens, is a bony projection from the second cervical vertebra (C2), which allows for rotational movement of the head.
A protuberance of the axis is the odontoid process, sometimes referred to as the dens. Due to this anatomical structure’s closeness to the spinal cord and brainstem, pressures operating on it may induce life-threatening fractures.
A bone fragment that extends superiorly from the second cervical vertebra (C2, or the axis), is known as the odontoid process or dens. The largest single component of the cervical spine’s lateral rotation is provided by the first cervical vertebra (atlas), which rotates around the odontoid process. 1. Type I: consists of the tops of the dens and is mostly stable. Dynamic radiographic imaging is advised if instability caused by the avulsion of the alar ligament is suspected. The fracture of the odontoid process is classified into one of three types: type I, type II, or type III fractures, depending on the size and morphology of the fracture.
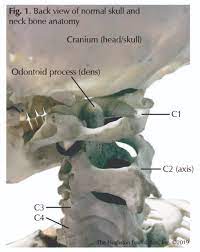
Clinically Relevant Anatomy
The C2 vertebra, also called the axis, is one of three atypical vertebrae. The axis denotes an odontoid process that extends superiorly from the body and resembles a peg. The odontoid approach lies anterior to the spinal cord and is utilized as the pivot for the rotation of the head. The C1 vertebra, which maintains the cranium, rotates on this.
The craniovertebral joint between the atlas and the axis is known as, the atlanto-axial joint. Because they lack intervertebral discs, the craniovertebral joints set themselves apart from other vertebral joints by having a wider range of motion than as compared to the vertebral column. The odontoid process and anterior arch of the atlas are maintained together by the transverse ligament of the atlas. This ligament avoids the volar displacement of C1 and the dorsal displacement of C2. If any displacement of this form occurs, the spinal cord can be compromised due to the narrowing of the vertebral foramen. The cervical nerves that flow above and below the axis are important for both the head and the respiratory system (diaphragm), thus they must not be overlooked as structures.
Odontoid fractures happen as a consequence of trauma to the cervical spine. In more youthful patients, they are generally the result of high-impact trauma, which happens as a consequence of a motor cycler or diving accident. In the geriatric population, trauma can happen after lower energy consequences for example falls from a standing position. The most typical cause of injury is a hyperextension of the cervical spine, moving the head and C1 vertebrae backward. If the energy cause and leading force are high adequately (or the patient’s bone density is compromised secondary to osteopenia or osteoporosis), the odontoid will fracture with variable displacement and degrees of comminution.
An odontoid fracture can also happen with hyperflexion of the cervical spine. The transverse ligament runs dorsal to (back) the odontoid process and attaches to the lateral mass of C1 on either side. If the cervical spine is excessively flexed, then the transverse ligament can transmit the extreme anterior forces to the odontoid process and generate an odontoid fracture.
Symptoms of Odontoid Fracture
Patients with odontoid fractures can show a variety of symptoms. Frequently, patients complain of neck pain and stiffness that is aggravated during neck movement. Difficulty swallowing, also understood as dysphasia, is another standard finding and can be correlated with bleeding from the fracture site resulting in a hematoma (blood collection). In uncommon instances, patients will have myelopathy (spinal cord injury) symptoms which may include abnormal reflexes, imbalance, and dexterity difficulties. Patients with neurological symptoms may complain of weakness in the hand and upper limbs and impaired sensation.
Epidemiology
Odontoid fractures account for twenty percent of cervical spine fractures in the older population and are the most familiar fracture subtype in older individuals equal to or older than 65 years. The axis (2nd cervical vertebra) is the most frequent vertebra to be involved in cervical spine damage, and odontoid fractures account for forty percent of all C2 fractures. This shows a bimodal division with peaks among initial adults and the aged population.
Odontoid fractures are caused by the combination of bone density and weight. This results from high-energy forces in young cohorts but trivial injuries in older ones. Hyperextension injuries cause the skull and C1 arch to cause traction at the odontoid process, while hyperflexion injuries cause the transverse ligament to limit the dorsal movement of the dens. Type II is the most ordinary of the kinds of odontoid fractures and accounts for more than fifty percent of all odontoid fractures. Type III odontoid fractures make up most of the left-behind odontoid fractures. Type I odontoid fractures are not very common. Road traffic accidents are answerable for the prevalence of circumstances. In a study consisting of more than 30,000 individuals, the average age of the cohorts was 77, and 44 percent were women.
Fractures of the dens account for around fifteen percent of almost all cervical spine typical axial fractures. The demographic groups differ as these fractures happen in both young patients because of a high-energy trauma (a motorcycle accident) and in old patients because of a low-energy trauma (for example, a fall). The fundamental cause of trauma is hyperextension of the neck. Other potential mechanisms involve blunt trauma or hyperflexion trauma.
There are three different kinds of odontoid process fractures, characterized by the anatomic site of the fracture line. This is known as the Anderson and D’Alonzo type. Type I fractures happen very uncommonly and type II is the very common
- Type I: avulsion fracture of the apex. Stable trauma.
- Type II: fracture through the base of the dens, at the connection of the odontoid base and the body of the 2nd cervical vertebrae. Frequentkly mot stanle trauma.
- Type III: fracture widens into the body of the axis. generally stable trauma.
Pathophysiology
Advanced age and big occiput-C2 angles are predictive of the odontoid fracture angle.
The atlantoaxial joint and fractured fragment all move in unison, resulting intolerable pain during movements of the neck. The nonunion rate next to conservative treatment may be as greater than ninety percent owing to thin bony trabeculae and watershed zone at the base of dens.
Non-operative treatment of odontoid fractures can consequence are given below:
- Solid fusion
- Non stable ununion, or
- Fibrous nonunion.
The fusion is governed by the subsequent:
- Type of trauma
- Fracture subtype
- The slope of the fracture line
- Angulation (greater or lower than 11 degrees
- Displacement (greater or lower than 5 mm)
- Blood circulation
- Bone quality, and
- Age of the patient and the fracture.
Risk Factors
When the cervical vertebral column is in hyperflexion (flexes excessively forward) or hyperextension (flexes excessively backward), type II odontoid fractures happen. Hyperflexion and hyperextension may be caused by trauma, for example, a fall or whiplash from a motorcycle accident.
Age plays a significant role in the incidence of odontoid fractures, which are the most common type of cervical spine fracture in patients older than 70. This is probably due to the increased risk of falls in the elderly, as well as the higher incidence of osteoporosis (a pathology of weak and brittle bones).
Even younger individuals are susceptible to type II odontoid fractures, which most frequently result from injuries mostly in motorbike accidents.
Differential Diagnosis
Several individuals may be incorrectly diagnosed with an odontoid fracture. It is important to be familiar with these to avoid pointless intervention.
OsOdontoideum
Osodontoideum is a documented anatomical variation of the normal C2 odontoid process. During development, there are multiple ossification centers in the spine, with one starting in the odontoid process, one in the odontoid tip, and one in the vertebral body. If the ossification centers in the odontoid process and the vertebral body fail to combine, then the odontoid process (dens) can be seen to be disconnected from the vertebral body and copy a type II odontoid fracture. In younger children, complete ossification of the spine has not yet taken place, and the regular growth pattern and ossification can also mimic a type II odontoid fracture.
Persistent Ossiculum Terminale
The rostral tip of the odontoid process has a take-apart ossification center during development from the residual odontoid process. When the two ossification centers fail to combine, there can be a constant gap between the odontoid process and the tip of the odontoid process, which may mimic a type I odontoid fracture.
Complications
Mortality at the moment of trauma is observed in 25 to 40 percent of patients.
Most of the survivors are usually neurologically intact. However, this can harbinger the threat of instability at the atlantoaxial area and spinal cord damage, resulting in Brown-Sequard syndrome, spinal cord injury, cruciate paralysis, myelopathy, and constant disabling neck pain in approximately 25 percent of patients.
There can be simultaneous damage correlated with and complicating the odontoid fractures, which contain:
- Anterior cervical wedge fracture
- Atlanto occipital dissociation
- Cervical burst fracture
- Cervical facet dislocation
- Cervical spinous process fracture
- Extension cervical teardrop fracture
- Flexion cervical teardrop fracture
- Hangman’s fracture
- Isolated transverse process fractures, and
- Jefferson fracture
Examination
Type 2 fractures are divided into many categories. Treatment for a type 2A fracture involves external immobilization and minimum displacement. Anterior screw fixation is typically used to treat misplaced type 2Bs. Treatment for a type 2C fracture, which runs from the anteroinferior to the posterosuperior, involves C1-C2 instrumental fusion. Co-morbidities must be evaluated throughout the diagnosis procedure since they may have an impact on the course of treatment. Besides the assessment of the co-morbidities, it is very important to subject the patient to a full neurological examination.
Evaluation
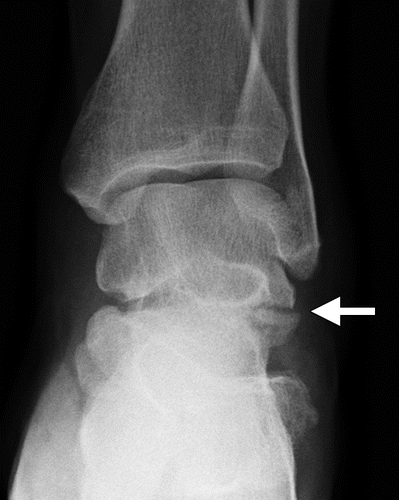
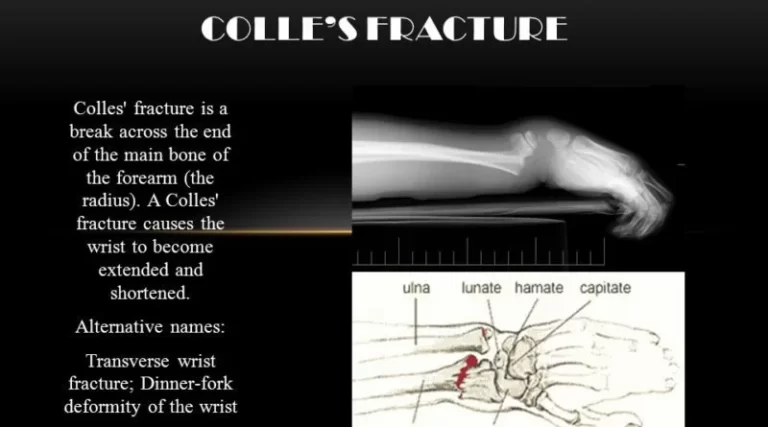
X-rays of the cervical spine comprise lateral, anterior-posterior (AP), and open-mouth views. Even though radiographs yield lower sensitivity and specificity rates when compared to computed tomogram (CT) scans, knowledgeable clinicians and practitioners can still be grateful for the assumed injury in the absence of CT utilization. In addition, flexion-extension radiographs must be obtained in the setting of supposed occipitocervical instability (helpful in type I odontoid fractures or the setting of osodontoideum). Early stability on upright radiographs is related to stability on follow-up.
Computerized tomography (CT) of the spine provides the most excellent resolution of the bony elements and permits the identification and description of an odontoid fracture. This also permits the recognition of anatomic anomalies, for example, the fault of the posterior arch of C1, that can help plan the management strategy.CT angiography is necessary in conditions with fracture extension within the surrounding area of the vascular zone and to examine the path of the vertebral artery during dorsal fixation.
Magnetic resonance imaging is used to examine the integrity of the transverse ligament as well as the cord in patients presenting with neurological impairment.
Classification of Odontoid Fractures
- Type I—consists of the tops of the dens and is primarily stable. Dynamic radiographic imaging is advised if instability caused by the avulsion of the alar ligament is suspected.
- Type II- included the neck of the odontoid procedure. They are categorized relying on the type of fracture line into anterior diagonal, posterior diagonal, and horizontal deviation. They are the most typical subtype and are almost considered not stable types. Type IIA alternative has comminuted fractures at the base of the dens and is not stable.
Grauer Classification
- Type IIA- un-displaced and no comminution
- Type IIB- fracture line passing anterosuperior to the posteroinferior direction
- Type IIC- Fracture line passing anteroinferior to posterosuperior direction, or with important comminution.
- Type III- fracture widens into the body of the second cervical vertebrae. Non-operative management stays the preferable alternative for the all most all of these patients.
Medical Management
In the literature, primarily 4 management strategies are reported, each with separate pros and cons. Operatively, the two management techniques discussed are volar screw fixation and dorsal C1-C2 fusion. Conservatively, the two primarily reported management alternatives are the Halo vest and the rigid cervical collar.
The management of Type I and Type III odontoid fractures has been revealed to be useful in a conservative way. The positive result of conservative management in terms of a greater union rate is associated with the higher stability of Type I and III fractures in comparison to Type II fractures.
The problem depends on the treatment of Type II odontoid fractures, which are the most frequent. More than a few aspects have been reported as being associated with the greater un-union rates of conservatively treated Type II fractures :
- the existence of cortical bone and poor vascularization of the axis;
- gapping because of the apical ligaments’ traction;
- displacement more than 5mm; angulation more than 10 degree;
- late start of management of more than 4 days
- age more than 65 years
Considering which management alternative to going for, co-morbidities must be examined first, so that insight might be gained into potential difficulties
Neurological management must also be present to identify eventual spinal cord trauma. Secondary myelopathy is an uncommon consequence of non-union, and although it is associated with a greater risk in the elderly, it may take years following follow-up before symptoms manifest.
Additionally, there have been a few case reports of Type III odontoid fractures leading to Brown-Séquard syndrome, but this is extremely rare.
Surgical Treatment of odontoid fracture
Operative indications informed in the literature are poly-trauma, neurological deficit, symptomatic non-union (myelopathy), and not stable un-union. Patients showing threat as noted earlier aspects for un-union are also regarded as being indicative of operation.
In order to stabilize the fracture, one or two screws are placed via the anterior-inferior corner of the C2-endplate. The Type IIB fracture, which runs anterior-superior to posterior-inferior, is said to have the best shape for this approach.
Volar C1-C2 fusion: different methods are reported. Gallie wiring technique, Magerl C1-C2 trans articular screw fixation, Harms posterior C1 lateral mass, and C2 pars screws.
Morbid obesity and thoracic kyphosis can interrupt perfectly reaching screw trajectory.
Conservative Treatment
According to an 11-year retrospective investigation, non-surgical treatment of stable Type II fractures has been shown to have positive long-term functional results in a younger population. The elderly (more than 65 years ) demonstrated inadequate long-term functional outcomes with higher rates of un-union.
There’s a big challenge in the reality that non-surgical treatment with external immobilization is associated with greater rates of morbidity (complications) and mortality in the elderly, particularly with the Halo vest. Yet, in several retrospective studies, the authors claim not to know the exact reasons for death, which could be just age-associated.
Halo vest immobilization has similarly been reported to have an un-union rate ranging from 26 percent to 80 percent.
The use of a semi-rigid cervical collar is said to be the manager of preference in the elderly (and younger patients with stable fractures), regarding the problems correlated to Halo vest immobilization and the operative chances of surgical management.
Non-union rates vary up to 77 percent for cervical collar immobilization, but when achieving an asymptomatic stable fibrous union is considered a favorable result, the union rates increase up to 92 percent.
Regarding the complexity of the management of Type II odontoid fractures in the elderly and inadequate total union rates, decreasing the work expectancy from complete union to the asymptomatic fibrous union could be brought into consideration.
The evidence does not support any particular management strategy for (Type II) odontoid fractures; hence, a customized strategy is needed.
FAQs
Diagnosis can be constructed with traditional lateral and open-mouth odontoid radiographs. Several fractures may be challenging to imagine on X-rays and need a CT scan to diagnose. MRI is very uncommonly indicated as these fractures are generally not correlated with neurologic symptoms.
Odontoid fractures have been separated into 3 primary kinds according to the type of Anderson and D’Alonzo. Type I is a relatively rare condition in which the alar ligaments avulse the odontoid tip. Type II happens at the base of the odontoid process and represents the most general fracture kind.
Extreme C2 fractures may need an operation and physiotherapy. If a C2 fracture does not outcome in paralysis, the victim may experience pain or problems moving the head until the fracture fully recovers. The prognosis for a C2 fracture is commonly good if the fracture did not result in paralysis.
Fractures of the odontoid are one of the most typical cervical spinal fractures in these residents. These fractures are associated with significant mortality rates of 25 percent to 37.5 percent, especially in older patients following low-velocity trauma.
The front section of the middle of the axis vertebra gives birth to the upward-pointing projectile of bone known as the odontoid process or dens. (The axis is the 2nd highest spinal bone.) The atlas is the first bone of your neck; it seats on top of the axis. (The atlas sits above the skull.)
The transverse ligament of the atlas (TLA) is a substantial, 20 mm long band that spans the atlas’ ring and maintains contact between the odontoid process and the anterior arch. It is concave in front, convex behind, and broader in the middle than at the ends.