Supracondylar Humerus Fractures
Table of Contents
Definition
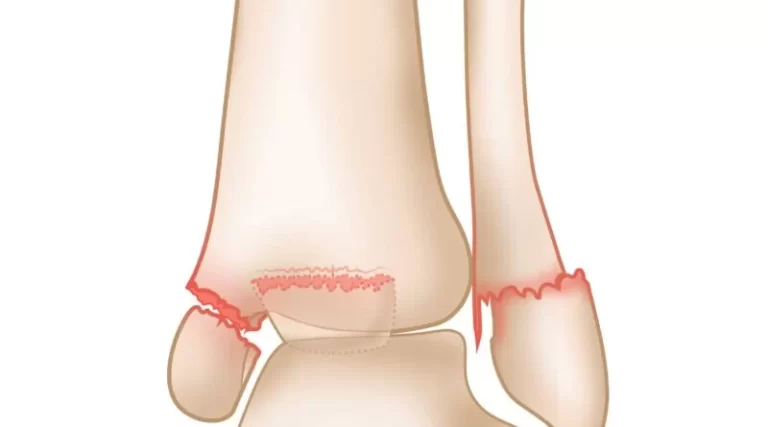
A supracondylar humerus fracture is a fracture of the distal humerus slightly above where the elbow joint is situated. The fracture is generally transverse or oblique in type and occurs above the medial and lateral condyles and epicondyles of the humerus. This fracture pattern is fairly infrequent in adults but is most common in children.
In children, most of the fractures are non-displaced and can be treated with a splint or casting. Few are angulated or displaced and are sufficiently treated with surgery. In children, most of these fractures can be treated effectively with the anticipation of a complete recovery. Few of these damages can be problematized by inadequate recovery or by a related blood vessel or nerve injuries with serious complications.
Clinical Anatomy
Association of the distal end of the arm with brachial artery and median nerve. The Supracondylar fracture is the fracture of the humerus bone at the distal portion of the humerus slightly above the elbow joint. The transverse section of the shaft of the humerus is somewhat circular which brings more flattered as it drops to complete the distal of the humerus.
The distal end of the humerus includes the articular and non-articular structures. Non-articular structure constitutes the medial epicondyle, lateral epicondyle, volar coronoid and radial fossa, and dorsal aspect olecranon fossa. Whereas the articular structure contains the lateral capitulum communicating with the head of the radius and the medial trochlea communicating with the ulna.
The medial epicondyle is the region where a common origin of flexor musculature of the forearm is situated and the ulnar nerve pass in a groove on the posterior of this epicondyle. The lateral epicondyle is the region where a common origin of extensor musculature of the forearm is situated. These muscles’ attachments are answerable for the displacement and rotation of the distal segment.
The volar aspect of the distal humerus permits the course of the brachial artery and median nerve. Entrapment of the brachial artery is one the most common and serious complications of supracondylar fracture of the humerus fibs along the anteromedial part of the distal humerus barely superficial to the brachialis muscle. The radial nerve pass between the brachialis and brachioradialis muscles before intersecting the elbow and piercing the supinator muscle
Epidemiology
- Supracondylar fractures of the humerus are the most common fractures of the pediatric humerus, with the age existing at 6 years and a top incidence at the ages of 5 to 8 years.
- It is the 2nd most typical bony injury in pediatric individuals.
- Out of the total fifty percent to eighty percent of entire elbow fractures in children and up to two-thirds of pediatric elbow injuries need hospitalization admission. Their incidence has been estimated at 177.3 per 1 lakh.
- Approximately 10 percent to 20 percent of displaced supracondylar fractures exist with alterations in the vascular situation. In most circumstances, fracture reduction restores perfusion.
- Neural damages happen in 6.5 percent to 19 percent of matters concerning displaced fractures. Majorities are neurapraxias.
Cause of Supracondylar Humerus Fractures
The most common causes of supracondylar fracture is a H/O fall from height from sports or leisure or a history of falls on an outstretched hand( FOOSH).
Extension-type injury of the Supracondylar fracture of the humerus.
The distal humerus anatomy is particularly predisposed to injury due to its composition of two columns joined by thin bone means a site of weakness.
Extension-type injury (97 percent to 99 percent is more typical than flexion-type (1-3 percent).
Fall on an outstretched hand ( FOOSH) During a fall on the outstretched hand happens, the olecranon engages the olecranon fossa, and if the elbow in extension continues, the olecranon ultimately serves as a fulcrum on the fossa. While the capsule of the elbow at the anterior aspect has an anterior tensile load, resulting in fracture and aggravation of the anterior periosteum. Thus, the bone starts to crack at first anteriorly and the fracture goes posteriorly. If the power is high, the posterior cortex disrupts, and eventually, full posterior displacement of the distal fragment happens with the posterior periosteum working as a hinge. This is the means of extension-type fractures.
Flexion-type fractures are usually driven by a direct hit when the flexed elbow is flexed. In these circumstances, the anterior periosteum serves as a hinge, and the progress of the injury moves from the dorsal to the volar aspect of the distal humerus. The distal fragment also tends to be translated into the coronal plane.
Symptoms of Supracondylar Humerus Fractures
Supracondylar fractures frequently exist linked to forearm fractures, soft tissue injury, neurologic damage, and consequential danger of producing compartment syndrome, thus an assessment of the whole upper extremity should be conducted thoroughly. It possesses:
History
- Classical H/O of fall on an outstretched hand followed by pain and swelling present around the elbow with the defective function of the upper extremity, the start of pain keeps certain concern.
- It is very fundamental to comprehend whether the source of the pain is because of a fracture or due to muscle ischemia which has late-onset normally hours after the trauma.
Observation
- Painful swollen elbow and forearm with uncertainty to move. Ecchymosis, skin puckering (this symptom occurs when the proximal fragment transects the brachialis muscle, ‘puckering’ the in-epidermis), bruises, Bleeding puncture injury(tells open fracture)
- In displaced extension-type fractures, the so-known as ‘S-deformity’ commonly exists.
Vascular status examination:
- Vascular compromise is present in up to 10 percent to 20 percent of displaced fractures. Both radial and ulnar pulses must be palpated at the wrist region of the affected limb. In the circumstance, Pulseless hand, other clinical manifestations of perfusion must be inspected for example color (the hand must be pink), temperature, capillary refill ( less than 2 seconds), and oxygen saturation on the pulse oximeter.
Classification:
- Class i – well perfused (warmness and redness) with radial pulse
- Class ii – well perfused despite radial pulse absent
- Class iii – poorly perfused (which is cool and blue or blanched) and radial pulse diminished
Neurologic status:
The degree of involvement and potential advancement or relapse of clinical manifestation of the nerve is should before and after therapy. Neuropraxias is expected and typically settles with the restoration of normal alignment and lengths.
Neuropraxias commonly settle within 2 to 3 months.
- The Anterior Interosseous Nerve Branch (AIN) of the median nerve is more venerable to getting involved in the postero-lateral displacement of the distal fracture segment. A child may have no sensorial loss in the hand region but a weak” OK sign” (e.g., more of a pincer grasp than an OK sign) on physical assessment.
- Radial nerve impingement most typically happens when the distal fracture segment is displaced posteromedially. It can be investigated with decreased sensation in the posterior aspect of the hand and weakness present in the wrist extensors muscle.
- The Ulnar nerve is predisposed to injury following flexion type of supracondylar fractures and lack of sensation in its distribution can be investigated following weakness of intrinsic muscles of the hand.
Compartment syndrome: Extreme swelling or ecchymosis, anterior skin puckering, and vascular compromise with extreme pain.
Diagnostic Procedures
X-ray must apply true anterior-posterior of the distal humerus and true lateral elbow views in displaced Supracondylar fracture. If there is just least or no displacement these fractures can be occult on X-ray. The singular sign will be a positive fat pad sign.
On lateral view
The lateral view also permits estimating the degree of displacement and the integrity of the posterior cortex.
On the lateral view, the subsequent X-ray parameters are examined for (a) an Anterior humeral line; (b) a Coronoid line; (c) a fishtail sign; (d) a Fat pad sign; (Anterior and Posterior).
The anterior humeral line to capitulum exposure on a lateral view:
- Normal elbow line resumes the anterior cortical of the humerus and must traverse the capitulum in its middle third line.
- Extension type injury: capitulum lies posterior to the line
- Flexion type injury: capitulum lies anterior to the line
On AP view
The Baumann angle or Humeral capitular angle on anterior-posterior view
- The angle between linea perpendicular to the long axis of the humeral shaft and the physical line of the capitulum is used to set the varus or valgus alignment of the distal humerus.
- Normal range – 64 degrees to 82 degrees
- Reduction in angle–varus angulated fracture with potential medial column comminution
The Ulnohumeral angle or X-ray carrying angle on the AP view
- It is utilized to evaluate varus or valgus deformity and it is more precise and helpful than Baumann’s angle
Classification of Supracondylar Humerus Fractures
Modified Gartland classification of supracondylar fractures (depend on lateral X-ray view):
Type I
- Nondisplaced or minimally displaced (<2mm) with intact anterior humeral line
- No disruption of periosteum – stable fracture
- Fat pad signs may be only found
Type II
- Displaced (>2mm) with hinged intact posterior cortex
- The anterior humeral line does not intersect via the middle third of the capitulum on lateral X-ray view
- No rotational deformity on the AP radiograph
Type III
- Displaced with no adequate cortical communication, usually sagittal plane extension and a frontal plane or horizontal plane rotation
- Marked periosteum disrupture, soft tissue, and neurovascular damages expected
- Medial cue comminution and failure with malrotation in the frontal plane
Type IV
- Multidirectional instability
- Incapable periosteal hinge circumferentially, with poor stability in flexion and extension direction
Complications of Supracondylar Humerus Fractures
Primary complications are related to neurovascular involvement possessing
- Vascular impairment involvement of the brachial artery is most regarded with Type II and III supracondylar fractures, usually located in posterolaterally displaced fractures.
- Compartment syndrome: It can happen in 0.1 percent to 0.3 percent of circumstances.Related forearm fractures and elbow flexion of more than 90-degree enhanced compartment pressures. To underrate the danger of compartment syndrome, the elbow must be immobilized in about 30 degrees of flexion in the emergency room and 60 degrees to 70 degrees after surgery.
- Neurologic impairment presents around 10 to 20 percent of supracondylar fractures and is especially linked with Type IIIsupracondylar fractures.
- Open or related forearm fractures.
Long-term difficulties in the Pediatric population because the point that bones in this age class have an immense growth as well as remodeling capacity. So the long-term functional result and radiological appearance of a fracture may be completely different from that of the immediate post-management situation.
- Cubitus varus deformity: It happens because of the malunion and is also called a “gunstock” deformity. After trauma cubitus varus deformity has common big concerns, which are correlated to the tardy ulnar nerve palsy, tardy Postero-Lateral RotatoryInstability (PLRI), the transition of the medial head of the triceps muscle, and secondary distal humeral fractures. Current surgical procedures (such as closed reduction with percutaneous pinning) have decreased their commonness from 58 percent to roughly 3 percent in children ministered for supracondylar fractures. Humeral osteotomy is utilized to fix this deformity and to evade such later complications.
- Volkmann’s ischemic contracture: If compartment syndrome is not treated timely, the related ischemia may continue to infarction, and following the formation of Volkmann’s ischemic contracture which is fixed flexion or deformity of the elbow, pronated forearm, flexion of the wrist, and extension of the metacarpal-phalangeal joint.
Treatment of Supracondylar Humerus Fractures
Medical
Treatment of supracondylar fracture is chosen depending on the kind of fracture established on the Modified Gartland Classification.
Type I ( Non-displaced fracture)
- Immobilization with a long-arm cast or splint.
- With the elbow kept in flexion, up to 80 percent to 90 percent and mid-pronation-supination are tolerable for around three weeks.
- X-ray check at one and two weeks
Types II
- A closed reduction(CR) and percutaneous pinning fixation are indicated in this type of case as the possibility of complication is not high. Pins are removed in the hospital around three weeks later surgery.
Type III and Type IV
Closed reduction and percutaneous pinning are the gold standard for all displaced fractures and are broadly used in Type III and IV fractures.
Open reduction is done when:
- When the surgeon is not capable to reduce the fracture by closed reduction means
- When there is soft-tissue entrapment (that is muscle, median nerve, brachial artery) or
- When a cold hand stays without perfusion after an attempt at closed reduction has been executed.
There is a high incidence of infection, stiffness of the joint, and myositis ossificans complication in open reduction. The anterior approach is a broadly employed approach for open reduction especially when vascular restoration is essential. The lateral approach is traditional for elbow surgery but supracondylar fracture raises the risk of injury of radial nerve and stiffness of the joint. The bilaterotricipital posterior approach (Alonso-Llames approach) is not advised as it has a high risk of complications described, for example, stiffness of the joint, bad cosmetic scarring, and risk of trochlea osteonecrosis.
Physiotherapy Treatment
Physical therapy treatment is critical among patients with a supracondylar fracture to quicken recovery and provide an optimal result. The objective, of physical therapy treatment, are given below:
- To achieve decreased pain and maximum mobility of the elbow joint.
- To enhance the healing process.
- To strengthen the affected musculature.
- To improve the general functional capabilities of children.
Result estimates that can be operated to correspond to and assess the result of treatment are:
- Numerical pain rating scale (NPRS)/ Faces Pain Scale
- Range of motion- Goniometry
- Manual muscle testing ( MMT)
- ASK-p (Activities Scale for Kids-performance version)
- Flynn’s standards have two aspects first “cosmetic factor” (lack of carrying angle) and the other ‘The functional factor’ (motion lack in degrees).
- The neuro-vascular examination is a must post-operatively and during rehabilitation.
Evidence
Physical therapy treatment in pediatric people is extremely contentious, in both its effect and its necessity. A randomized controlled trial accomplished by Schmale et al. in 2014, had indicated that children with supracondylar fracture ministered with either casting or closed reduction with percutaneous pinning followed by casting were not helped from a short period of physical therapy (six sessions of physical therapy conducted over a five-week period starting the week after cast removal) in times of either return of function or motion. Keeping the above analysis, another investigation done in 2018, also reveals that children managed with closed reduction for uncomplicated supracondylar fracture with immobilization for 3 weeks recover their functional range of motion within twelve weeks of mobilization by itself, with no added usefulness from physiotherapy.
Physiotherapy treatment has not demonstrated a significant difference, it may be because of the involvement of children ( five-ten years) more involved in everyday household activities from an earlier period and the desire for a motion for playing.
On the opposite, in a more extreme kind of damage with neurovascular involvement and in an adult patient, physiotherapy treatment has an important role. And in the pediatric population, proof has been lacking to address the strength of the upper extremity as a result of physiotherapy treatment.
Therefore,
- Optimal loading(pain-free movements based on a child) is very essential for pediatric residents with supracondylar fractures as pain-aggravating activities may interrupt the healing process and result in further damage as they are in a growing phase.
- Thus, active exercise and active involvement in sports and activities of daily living are suggested instead of passive joint mobilization and stretching exercises.
- Weight lifting, weight-bearing, or pushing movements that possess enormous quantities of stress through the humerus must also be prevented in the initial week after immobilization removable.
- Progressive strengthening exercises can be addressed.
Advice and Exercises During the Immobilization Period
- Commonly elbow is immobilized for three weeks so, during that time, neighboring joints ( which are the Shoulder joint and wrist joint, and hand) must be maintained by moving actively or active-assisted exercises often during the day.
- The elbow must not be moved and the use of an arm sling must be correct.
- Postural education ( sitting upright with a relaxed shoulder and retraction of the scapula) must be instructed.
1-2 Weeks After the Removal of the Cast
- Hot fermentation can be utilized to reduce the stiffness of the joint.
- Gentle soft tissue release can be done in the arm and forearm musculature.
- Gentle active and active-assisted exercises by utilizing a wand and be trained in the pain-free range- often in a day.
- Isometric exercises for arm and forearm musculature may be given.
- Educate parents and children to use the involved hand to use in ADLs for example brushing, writing, eating, dressing, etc.
- Avoid weight lifting and pushing activities.
Guidance and Exercise After 2 Weeks of Cast Removal
- Progressive and interactive range of motion activities and strengthening exercises must be given for example passing a ball, donning, and doffing clothes.
Conclusion
- Supracondylar fractures of the humerus are the most typical among juveniles at the ages of five to eight years.
- History of FOOSH is the common mechanism of injury of the Supracondylar fracture of the humerus.
- The Neurovascular assessment is a must pre and post-operatively.
- Closed reduction with percutaneous pinning is the suggested medical management for displaced fracture without neurovascular involvement.
- Active exercise is recommended for pediatric elbow fractures rather than passive treatment.
FAQ
Gunstock deformity also understood as Cubitus varus or bow elbow is the consequence of malformation after happening as an expected complication of supracondylar fracture of the humerus. It happens in only the extension type of supracondylar fracture of the humerus, provoking a decrease or loss of the carrying angle.
Complications:
Malunion: caused by cubitus varus (varus deformity of the elbow, also called gunstock deformity)
Ischemic contracture (Volkmann contracture) because of damage or occlusion to the brachial artery and causing in volar compartment syndrome.
Injury to the nerve of the arm which is the ulnar nerve, median nerve, or radial nerve.
Complications. palsies of the nerve of the arm which is the ulnar nerve, median nerve, or radial nerve are expected with the type of supracondylar fractures, with neuropraxia rates roughly 10 percent; regardless, this rare outcome is permanent impairment. The anterior interosseous nerve is most generally influenced by the initial injury, regardless ulnar nerve palsy is the most typical postoperative complication.
A supracondylar humerus fracture is a fracture of the distal humerus slightly above where the elbow joint is situated. The fracture is generally transverse or oblique in nature and above the medial and lateral condyles and epicondyles of the humerus. This fracture pattern is fairly infrequent in adults but is most common in children. This is named a supracondylar (soo-pruh-kaan-duh-lr) humerus fracture. It is the most familiar type of elbow fracture and occurs most frequently in children younger than 8 years old.
The most threatening complications are those that may be disastrous for patients, provoking a significant lack of function or even amputation of the extremity; such as vascular damage and compartment syndrome.






3 Comments