Osteopenia
Osteopenia is a loss of bone mineral density (BMD) that exhausts bones. It is more usual in individuals older than 50, specifically women. Osteopenia does not have any kind of signs or symptoms, but a painless screening test may measure bone strength. Certain lifestyle changes may help a person to preserve bone density and prevent osteoporosis.
Table of Contents
Epidemiology
- Worldwide, Asia has reported the minimum average t-scores by region.
- Overall, females have a four-fold higher overall prevalence of osteopenia compared to men.
- Australia reported an incidence rate of osteopenia in 42% of male and 51% of female.
- India reported a 52% overall incidence in its people in 2005.
- In the United States, 54% of postmenopausal females are osteopenic.
What causes osteopenia?
- Bones are made of living tissue. Up until about age thirty, a healthy person builds more bone than he or she loses.
- But after age thirty-five, bones start to break down faster than they build up.
- Even in a healthy person, bone density reduces throughout life, by less than 1 percent per year.
- Some things may make bone loss happen more quickly, leading to osteopenia, like:
- Medical conditions like hyperthyroidism.
- Medications like prednisone and some treatments for cancer, heartburn, high blood pressure, and seizures.
- Hormonal changes during menopause.
- Poor nutrition, specifically a diet too low in calcium or vitamin D.
- Surgery on the gastrointestinal system may affect the body’s ability to absorb needed nutrients and minerals.
- Unhealthy lifestyle choices, like smoking, drinking too much alcohol or caffeine, and not exercising.
What are the symptoms of osteopenia?
Osteopenia usually does not cause any signs or symptoms until it progresses to osteoporosis. Rarely, some individuals with osteopenia can feel bone pain or weakness. The condition is generally identified when a person has a BMD screening. About half of Americans older than age fifty get osteopenia. The more of these risk factors persons have, the higher their risk is:
- Being female
- A family history of low BMD
- Being older than age 50
- Menopause before age 45
- Removal of ovaries before menopause
- Not getting enough exercise
- A diet lacking calcium and vitamin D
- smoking or using other forms of tobacco
- Drinking too much alcohol or caffeine
- Taking prednisone or phenytoin
Certain other conditions may also at the risk of developing osteopenia:
- Anorexia nervosa
- Bulimia nervosa
- Cushing’s syndrome
- Hyperparathyroidism
- Hyperthyroidism
- Inflammatory conditions such as rheumatoid arthritis, lupus, or Crohn’s Disease
Diagnosing osteopenia
The National Osteoporosis Foundation suggests that a person has her BMD tested if the persons are:
- A woman age 65 or older
- younger than sixty-five, postmenopausal, and have one or more risk factors
- postmenopausal and a person have broken a bone from normal activity, like pushing a chair to stand up or vacuuming
- The doctor can suggest that a person has the BMD tested for other reasons.
- For example, about one in three white and Asian men older than age 50 have minimal bone density.
DEXA test
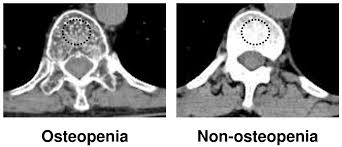
- Dual-energy X-ray absorptiometry, called DEXA or DXA, is the most usual way to measure BMD.
- It is also identified as a bone mineral density test.
- It uses X-rays that have minimal radiation than a typical X-ray.
- The test is painless. DEXA generally measures bone density levels in the spine, hip, wrist, finger, shin, or heel.
- DEXA contrasts the density of the bone to the density of a 30-year-old of the same sex and race.
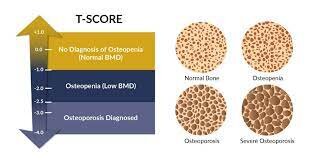
- The result of a DEXA is a T-score, which the doctor may use to diagnose a patient.
| T-score | Diagnosis |
| +1.0 to –1.0 | Normal bone density |
| –1.0 to –2.5 | Low bone density or osteopenia |
| –2.5 or more | Osteoporosis |
If the T-score shows persons have osteopenia, the DEXA report can involve the FRAX score. If it does not, the doctor may calculate it.
The FRAX tool uses bone density and other risk factors to estimate the risk of breaking the hip, spine, forearm, or shoulder within the next 10 years.
Treatment of Osteopenia
There is no cure for osteopenia, but it is necessary to preserve bone density as much as possible. Treatment includes simple strategies to keep the bones as healthy and strong as possible and prevent progression to osteoporosis:
- Calcium treatment.
- Exercise.
- Healthy diet.
- Supplements for vitamin D deficiency and exposure to the sun help the body absorb vitamin D.
- The doctor will also want to monitor the bone density over time in case a person develops osteoporosis.
Physiotherapy treatment in Osteopenia
Before a person starts, Consult the doctor prior to starting any exercise program for osteoporosis. A person might need some tests first, including:
- Bone density measurement
- Fitness assessment
- In the meantime, think about what kind of activities a person enjoys most.
- If a person chooses an exercise he or enjoys, a person is more likely to stick with it over time.
- Choosing the right form of exercise.
- These types of activities are frequently recommended for people with osteoporosis:
Strength training exercises,
- specifically those for the upper back
- Weight-bearing aerobic activities
- Strength training involves the use of free weights, resistance bands, or the own body weight to strengthen all major muscle groups, specifically spinal muscles important for posture.
- Resistance training may also help maintain bone density.
- If a persons use weight machines, take care not to twist the spine while performing exercises or adjusting the machines.
Resistance exercises
- When you add resistance to the routine, the muscles release calcium, magnesium, and other minerals that strengthen the bones, These exercises use mechanical resistance from weight-bearing, like resistive bands or weights. Resistance training should be altered to the ability and tolerance, specifically if a person has pain. A physical therapist or personal trainer with experience working with individuals with osteoporosis may help a person develop strength-training routines. Proper form and technique are important to prevent injury and get the most from the workout. perform 3 sets of 10 repetitions of these exercises,. “You’ll get the toning and a little bit of cardio.”
Pushups:

- Pushups may be done in a variety of positions.
- Try something different from a common pushup.
- Standing pushups:
- Stand approximately three feet away from a wall, facing it.
- Place the hands shoulder-width apart at chest level against the wall.
- Bend the elbows as a person leans into the wall.
- Straighten the elbows, pushing the body weight away from the wall.
Seated pushups (adapted):
- Grasp a lightweight pole, such as a broomstick, with palms down with the arms shoulder-width apart at chest level.
- Push the pole away from the chest, straightening the arms.
- Then bend the elbows, returning the arms to the chest.
Resistance bands:
- Resistance bands (like TheraBand) are a light, movable way to strengthen.
- They are color-coded to indicate different resistance levels.
- For those who are just starting an exercise program or have joint issues, it is best to use a lighter resistance band and slowly work up to moderate and then heavier resistance bands.
- Remember, how important it is not to force any movement.
Band pull

- A person may perform this exercise while seated or standing.
- Again, if seated, it is necessary to support the feet on the floor or footrests.
- Hold onto the band approximately five inches away from the chest, arms shoulder-width apart.
- Hands are palms-down at chest level. Gently pull the band, extending the arms beyond shoulder width.
- Try to straighten the arms as far as possible while creating tension in the arms.
- Gently back to the beginning position, releasing the tension in the arms.
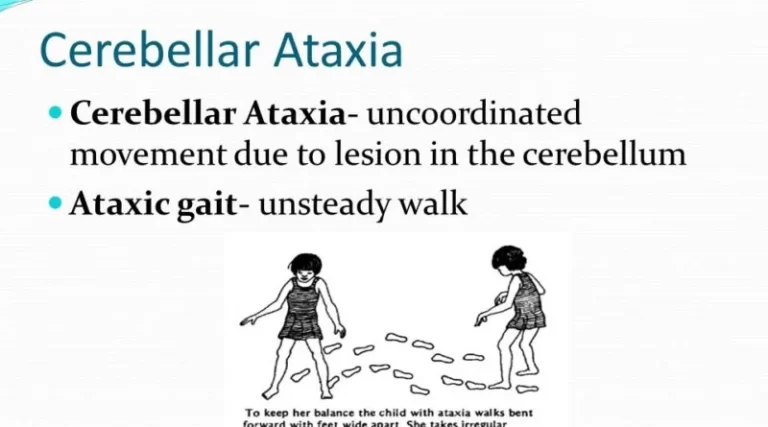
Balance and core exercises
- The core encompasses the stomach muscles, back muscles, and pelvic girdle.
- “A core workout does not necessarily mean doing sit-ups,”. “Everything we do engages the core.”
One-leg stand:

- Stand with your hands supported on a table or the back of a firm chair.
- Balance on one leg while raising the other off the floor.
- Count to ten while engaging the stomach muscles. Return the leg to the floor and alternate legs.
- Repeat 3 times.
- When a person first tries it, stabilize it with two hands on the kitchen counter.
- As the core strengthens and the balance increase, a person may transition to stabilizing with just one or two fingers from each hand. Eventually, a person will be able to eliminate the hands.
Standing straight:
- Contract (hold in) the abdomen (belly), so the belly button pulls toward the spine. Stand straighter as a person stabilize the core.
Seated core:

- Even seated, a person may build the core muscles by Sitting on a firm seat, arms crossed over the chest, legs bent.
- Alternate raising each thigh one to 2two inches, engaging the core.
- Lower thigh to starting position.
- Sitting on a firm seat, arms crossed over the chest, straighten one knee and then back to the starting position.
- Change the legs.
Flexibility
- Stretching is necessary to elongate the muscle fibers.
- There are many variations of stretches for the upper body and lower body, incorporating the hamstrings and calf muscles, which may get very tight from sitting.
Hamstring stretch:

- Start with lying on the back, a pillow under the head.
- Bend the knees with the feet flat on the floor or bed.
- Straighten one knee and lift one leg up toward the ceiling. Using both hands, grasp and hold behind the thigh for 20 to 40 seconds.
- A person can wish to interlock the fingers to better support the leg.
- Do not force the stretch.
- Lower the leg to initiate a position.
- Change the legs and repeat.
- Do one to two sets.
Shoulder stretch:
- Standing or sitting, stretch the arms out in front of you with elbows straight.
- Interlock fingers.
- Lift both arms up toward the ceiling.
- Hold for 10 to 20 seconds.
- Gently return to starting position.
- Do 2 to 4 sets.
Prevention
Too many different strategies can help you maintain bone strength and prevent bone loss:
- Avoid smoking.
- Try to eat a healthy, balanced diet with lots of fruits, vegetables, calcium, and vitamins.
- Exercise every day. Walking, jogging and other activities that make a person bear their own weight are particularly helpful, as is weight training.
- Get at least 1,200 mg of calcium on a daily base.
- Get at least 800 to 1,000 IU of vitamin D on a daily base.
- Go outside for exposure to the sun, which helps the body absorb vitamin D into the bloodstream.
- Limit alcohol.
FAQ
Though osteoporosis is considered the more severe form of osteopenia, osteopenia may be just as dangerous as osteoporosis
when merged with other risk factors, like smoking, a low-calcium diet, lack of vitamin D, hormonal changes because of age
(specifically menopause), and the presence of autoimmune conditions.
Salt. Doctors advise individuals with osteopenia to limit their salt intake because eating foods high in salt may remove calcium
from your bones.
Caffeine.
Inflammatory Foods.
Sugary foods.
Alcohol.
Soft Drinks.
Processed meats.
Natural treatments and prevention involve: eating a nutrient-dense diet with enough calcium and vitamin D; getting proper exercise; maintaining a healthy weight; not smoking; and preventing vitamin D deficiency by getting proper sunlight exposure.
Weight-bearing exercises, like walking, jogging, and climbing stairs, may help people build strong bones and slow bone loss.
Those over age fifty are encouraged to consume fortified foods or supplements containing B12. This study recommends adequate vitamin B12 intake is important for maintaining bone mineral density.



One Comment