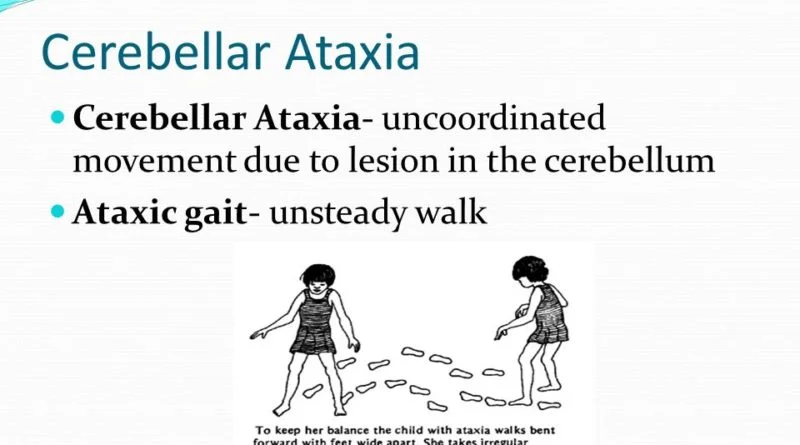
Cerebellar Ataxia: Physiotherapy Treatment
Table of Contents
What is a Cerebellar Ataxia?
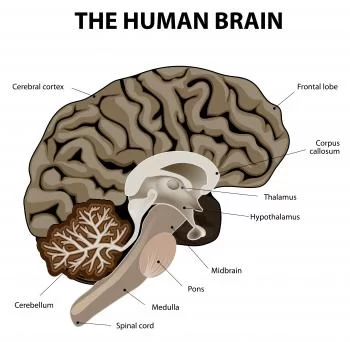
Acute cerebellar ataxia (ACA), also known as cerebellitis, It is a disorder that occurs when the cerebellum becomes inflamed or damaged.
The cerebellum is the area of the brain responsible for controlling gait and muscle coordination.
It is a term used to describe certain behaviors like postural unsteadiness, difficulty in co-coordinating movements & clumsiness experienced by an individual with cerebellar dysfunction.
Treatment for ataxia depends on the cause, and symptoms. Regular Physiotherapy treatment helps to gradually improve coordination and balance and with the helps of stick or walker you can start walking. Other therapist may involve in the treatment plan are occupational therapy and speech therapy
Causes of Cerebellar Ataxia:
Following are the list of conditions in which the cerebellar area of the brain may inflamed or damaged which are the main causes of ataxia, these are:
- Viral infections that may cause this include chickenpox, Coxsackie disease, Epstein-Barr, and echovirus.
- bleeding in the cerebellum
- exposure to mercury, lead, and other toxins
- bacterial infections, such as Lyme disease
- head trauma
- CNS vasculitis, multiple sclerosis
- Developmental abnormality e.g. Hydrocephalus, Arnold Chiari Malformation
- Trauma, focal lesion
- Cerebellar Stroke
- tumour in the Cerebellar area
- infection in the Cerebellar area
- Demyelinating diseases like MS
- Degenerative disease
- Hereditary (Fredriech’s ataxia)
- Metabolic disease (B12 deficiency)
- Vascular disease
- Drug intoxication or exogenous substance (ethanol causes reversible cerebellar & vestibular ataxia)
Symptoms of Cerebellar Ataxia :
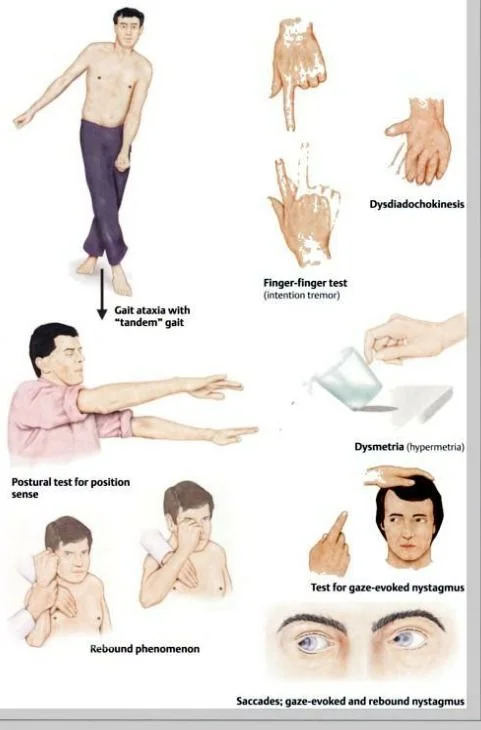
- coordination difficulties
- loss of Balance
- Hypotonia
- Dysmetria
- Dysdiadokokinesis
- Tremor
- Movement decomposition
- Ataxic gait
- Scanning speech
- Asthenia
- Rebound phenomena
- Difficulties in swallowing
- Dysarthria/ scanning speech
- Nystagmus (Central nystagmus)
Types of Ataxia and their characteristics:
Peripheral nerve disease and injury to various motor or sensory parts of the central nervous system can both cause ataxia (Bastian 1997). Ataxia can generally be caused by issues with the cerebellum, the proprioceptive system, the visual system, the vestibular system, and/or any issue with how these systems are connected.
While ataxia is classified into two categories by some researchers (Bastian 1997), it is classified into three categories by others (Morgan 1980), including vestibular, cerebellar, and sensory ataxia. According to Erasmus (2004), there are scholars that classify frontal ataxia as a fourth category. Mixed ataxia is the term used to describe a situation in which two or three different ataxia types exhibit symptoms (Edwards 1996).
Sensory ataxia:
Since the dorsal columns of the spinal cord transmit proprioceptive information to the brain, ataxia resulting from loss of proprioception—or sensitivity to joint and body part position—is referred to as sensory ataxia. The thalamus and parietal lobes, among other brain regions that receive that information, may malfunction in certain situations. When proprioceptive input is lacking and cannot be replaced by visual input, especially in poorly illuminated surroundings, sensory ataxia manifests as an unsteady “stomping” walk with heavy heel strikes and postural instability.
When a patient stands with their feet together and their eyes closed, their instability worsens, perhaps leading to large oscillations and a fall. The most important finding that distinguishes sensory ataxia from other forms of ataxia is that this indicates a positive Romberg’s test result (Bannister 1992). Among the key features of sensory ataxia are loss of deep tendon reflexes and vibration perception in the extremities. Another sign of sensory ataxia is a worsening of the finger-pointing test when the eyes are closed.
Hereditary ataxias such Friedreich’s ataxia and spinocerebellar ataxia can exhibit sensory ataxia. Additionally, disorders including vitamin B12 insufficiency neuropathy, diabetic or alcoholic neuropathy, tabes dorsalis, tumor situations located in the posterior cord of the medulla spinalis, and multiple sclerosis can also cause sensory ataxia (Edwards 1996).
Vestibular ataxia:
Diseases affecting the peripheral or central nervous system that directly impact the vestibular nuclei or their afferent and efferent connections can cause vestibular ataxia. When sitting or standing, a patient with vestibular ataxia experiences balance problems. The patient has a wide base of support, staggers when walking, and occasionally leans to the side of the lesion or back. Arm mobility is frequently reduced as a result of head and trunk movements (Borello-France et al. 1994).
The patient is restricted because it is difficult for him or her to maintain equilibrium when making head or eye movements, especially when crossing the street and shopping at the market. Due to the vestibular system’s function in detecting and perceiving self-motion and stabilizing gaze through the vestibulo-ocular reflex, vestibular ataxia may be accompanied with vertigo, nausea, vomiting, blurred vision, and nystagmus (Horak & Shupert 1994). Vestibular ataxia by no means exhibits extremity ataxia. It is thought that deep tendon reflexes are normal.
Both central (such as multiple sclerosis and medullar stroke) and peripheral vestibular disorders (such as Menier’s, hydrops, benign paroxysmal vertigo, or vestibular neuronitis) can cause vestibular ataxia.
Cerebellar ataxia:
Lesioning the cerebellum or its afferent and efferent pathways can lead to the development of cerebellar ataxia.
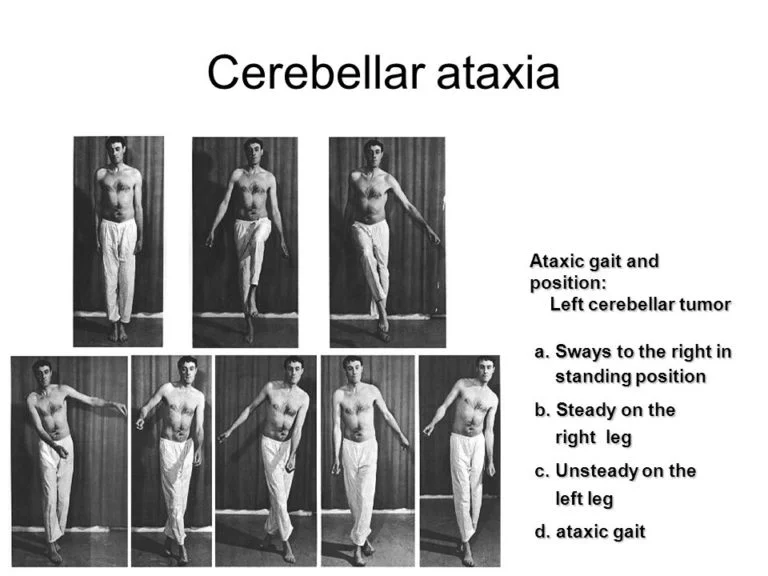
Vestibulo-cerebellar dysfunction pertains to issues with balance regulation and eye movement control, and it is associated with the flocculonodular lobe (flocculus and nodulus). Postural instability manifests as a tendency to separate feet when standing in order to create a wider base and prevent oscillations, particularly posterior-anterior ones; standing with feet together exacerbates instability regardless of whether the eyes are open or closed, as demonstrated by a negative Romberg’s test (en.wikipedia.org, Liao et al. 2008, Morton&Bastian 2004).
Patients with spinocerebellar dysfunction, which affects the vermis and paravermis, will have a wide-based gait with irregular patterns of inter-joint coordination, lateral deviations, uneven steps, and erratic start and stop. Gait ataxia or walking incoordination is the result of injury to this area of the cerebellum (Timmann et al. 2008, Morton & Bastian 2007).
Dysfunction of the cerebral-cerebellum link is indicative of a lesion in the deep pontine nuclei. Damage to the cerebrocerebellum, which is involved in movement planning and monitoring, impairs the ability to perform voluntary, planned motions (Chmahmann 2004).
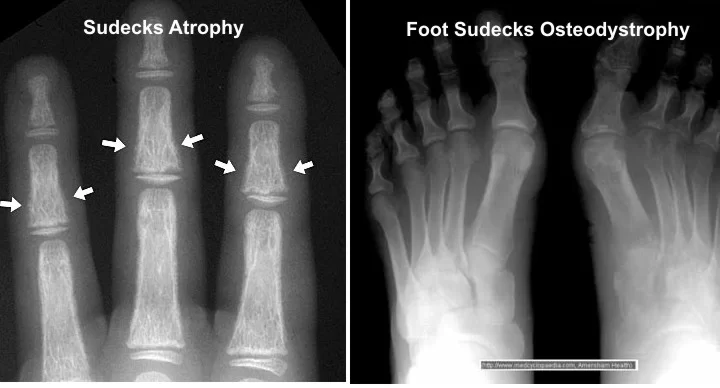
Investigation
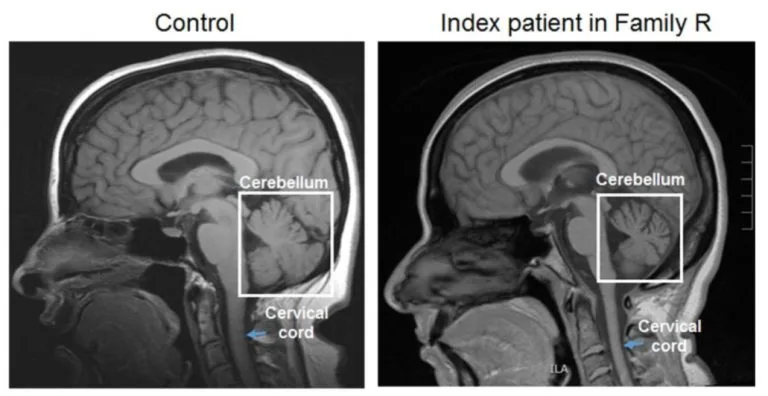
- MRI or CT scan – to determine whether there is any brain damage.
- Cerebellar atrophy
- Cerebellar tumour
- Cerebellar infarction
- Tonsilar invagination & hydrocephalus
- Arnold chiari malformation
Genetic tests – to determine whether the patient has inherited ataxia.
Blood tests – some types of ataxia affect the make-up of blood.
Urine tests – urinalysis may suggest specific systemic abnormalities that are linked to some forms of ataxia.
If the specialist suspects Wilson’s disease, the patient may be asked for a 24-hour urine collection to determine how much copper is in the system.
Treatment of Cerebellar Ataxia
Medical treatment depends on the cause and also depends upon symptoms:
- If the acute cerebellar ataxia is due to haemorragic bleeding, emergency craniotomy surgery may require.
- For an ischemic cerebellar stroke, medicine to thin the blood can be given.
- To control Infections treatment is antibiotics or antivirals medicine.
- Corticosteroids also prescribed to control inflammation of the cerebellum such as multiple sclerosis.
- Cerebellar ataxia caused by a recent viral infection may prescribed antivirals medicine or sometimes rest with not need for any particular treatment.
Other treatment methods:
Transcranial direct current stimulation (tDCS) is a form of neuromodulation of the brain that uses continuous, low direct current applied via electrodes over the head. It was initially developed to help patients with brain-related conditions / neuropsychiatric conditions such as major depressive disorder. Cranial electrotherapy stimulation, which mainly uses alternating current with same method, in addition to transcranial magnetic stimulation.
Transcranial magnetic stimulation (TMS) is a non-invasive treatment option in which magnetic fields stimulate nerve cells of the brain.
Physiotherapy treatment in Cerebellar Ataxia:
- Relaxed passive motion
- General rocking movement
- Relaxed positioning
- Deep breathing exercise
- PNF technique
- Relaxation techniques
- A ROM exercise & other free exercises
Frankel’s Co-ordination Exercise:
Frenkel coordination exercises are a series of exercises invented by Professor Heinrich Sebastian Frenkel (a physician from Switzerland) for the treatment of cerebellar ataxia.
This set of exercises consists of controlled, repeated movements. This exercise increases the difficulty of movement over time to improve coordination. The patient practices their hand or arm movements and corrects them as needed. Frenkel’s exercises helped to improve the rhythmic, smooth, and coordinated movements.

Gait training
- Lengthen stride length
- Concentrate on heel-to-toe pattern, Improve arm swing
- Parallel bar activities
- Walk on printed foot prints
- Marching on the spot with an arm swing
- Walking in a straight line
- Walking in circle
- Walking sideways with an outstretched hand

Ataxia management
Promote accuracy of limb movements by using aids, cues & feedback
Combined activities of the trunk & limbs to improve coordination, balance & automaticity of movement
Frenkel’s coordination exercise
Small weight cuffs, ankle & wrist bands can be used during activities to increase awareness of the limbs
Weight-bearing exercise of the Upper Limb & Lower Limb


Approaches for improving proprioception:
By manually stimulating the joint surfaces, muscles, and tendons, the goal is to increase proprioceptive input. It also aims to reduce postural instability by enhancing body awareness. There are numerous methods that can be applied in this way.
Proprioceptive Neuromuscular Facilitation (PNF), rhythmic stabilization, slow reversal techniques (Adler et al. 2000), resistive exercises (DeSouza 1990), using Johnstone pressure splints (Armutlu et al. 2001), practicing gait on various surfaces (hard, soft) with eyes open and closed, plyometric exercises (Risberg et al. 2001), and practicing balance on a board-ball and minitrampoline Exercises (Diracoglu et al. 2005).
Vibration has become a commonly used application in recent times. Both direct application of vibration to the muscle and tendon as well as total body vibration exposure are possible (Schunfried et al. 2007).
Suit therapy is an additional approach. The suit consists of a vest, shorts, knee pads, and unique shoes that are fastened to the body using bungee-style bands. These bands are designed to generate resistance and ensure proper body alignment during movements. Its main objectives are to enhance weight-bearing for normalized sensory input regarding posture and movement, as well as proprioception (feeling from joints, fibers, and muscles) (Semenova 1997).
Program components that promote body awareness include yoga, body awareness exercises, and approaches like the Feldenkrais and Alexandre Techniques (Jain et al. 2004).
First and foremost, strengthening the proximal muscles and trunk stabilization is necessary (Edwards 1996). It is appropriate to use the PNF techniques’ mat activities for this aim. The patient should be taught to crawl, come to the bridge position from lying on their back, come onto the forearms from face down, come onto the knees, half-knees, and sit, and to establish both static and dynamic stability in these positions, all in accordance with the neuro-developmental order. Static stabilization should be reinforced by external disturbance (pulling and pushing in different directions) once the patient has been kept in the desired position initially via approximations and spoken instructions.
In order to get ready for dynamic stabilization, the patient should next be trained in these positions for weight transfer and functional extension. In order to make the balancing exercises challenging, the patient should then be trained in situations where the center of gravity is shifted or the support surface is restricted. (For instance, stabilizing oneself on two or three limbs when crawling, or raising one’s arms to raise one’s center of gravity while sitting on the floor) (Addler et al. 2000).
One leg balancing exercises should be done while standing, after shifting weight to the front, back, and sides, narrowing the support surface, and practicing balance in tandem. Patients with ataxia struggle greatly in this position.
To take use of the visual feedback that comes from seeing how long the patient can maintain his or her postural oscillation in the center of gravity, another alternative is to use the posturography device for balance training (Qutubuddin et al. 2007).
Gait is the best measure of dynamic stabilization and balance. Thus, gait training should cover the following exercises: walking in two narrow lanes; tandem walking; backward walking; slowed-down walking (soldier’s gait); stopping and turning in reaction to abrupt directions; and head flexion, extension, and left-right rotations.
Activities in disciplines like yoga and tai chi (Hackney & Earhart, 2008) help people gain balance.
Vestibular exercises:
Cawthorne and Cooksey exercises (Dix 1979) and repetitive head motions are very important because dizziness follows balance impairment in vestibular issues. A vestibular exercise program consists of a series of eye, head, and body motions that are repeated and get harder and harder in order to promote movement and help with sensory substitution. Physical and occupational therapists still use many of the exercises in this program (Ribeiro et al. 2005,Brown et al. 2006).
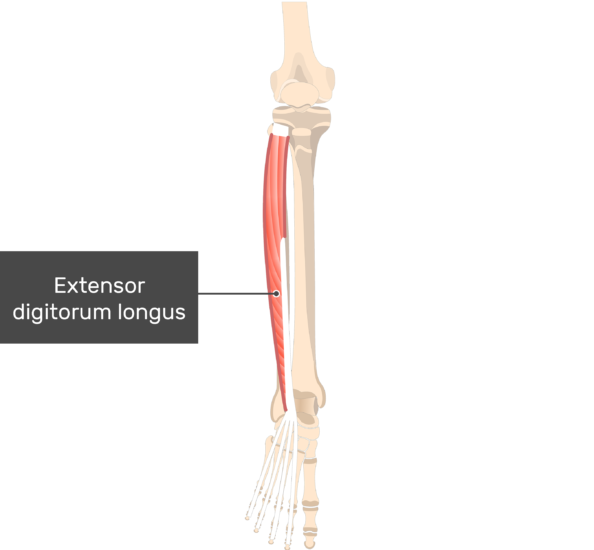
Approaches to extremity ataxia:
Fixation is achieved by establishing equilibrium between the eccentric and concentric contractions within the multi-joint movements of the lower limbs, and the upper extremities in particular, using exercises intended for the treatment of extremity ataxia. It is crucial to establish gradual, controlled, reciprocal multi-joint movement as well as stabilization when performing these exercises. For this reason, Freenkel’s coordination exercises were created (Edwards 1996). Actively repeated contractions that resemble PNF can be used alone or in conjunction with the coordination exercises developed by Frenkel (Armutlu et al. 2001).
Although these two forms of exercise are useful for those with mild symptoms of ataxia of the extremities, they may not be enough for more severe cases. PNF is less successful in these situations than a combination of isotonic methods and rhythmic stabilization (Adler et al. 2000).
The creator of Coordination Dynamics Therapy (CDT) is Dr. Giselher Schalow. By practicing incredibly precise coordinated arm and leg movements on a specialized device (GIGER MD), this therapy enhances the self-organization of the CNS’s neuronal networks for functional repair. This, in turn, leads to the coordinated firing of the human CNS’s billions of neurons (Schalow 2006).
Conclusion
The patient’s upper extremity and mobility are their most vital functions, according to the physiotherapist. When compared to other neurological disease symptoms like muscle weakness and spasticity, ataxia is a serious neurological issue that can often be more difficult to manage and persistent.
Applications of physiotherapy are therefore crucial to the treatment of cerebellar ataxia. The success of the treatment program greatly depends on the patient’s evaluation, the choice of appropriate treatment techniques and approaches, the use of issue solving techniques, and the frequent performance of the exercises.
FAQ
Can cerebellar ataxia be cured?
There is no specific treatment option available for ataxia. In a few cases, where treating the cause of ataxia may help to recover from the ataxia. In a few cases, where ataxia occurs due to chickenpox or other viral infections, it is likely to recover as it is on its own.
How long can you live with cerebellar ataxia?
Life expectancy is generally reduced than normal people as compared with hereditary ataxia, although some patients can live long enough into their 50s, 60s, or beyond. More severe conditions can be fatal in childhood or early adulthood.
Is cerebellar ataxia a stroke?
A stroke that damage the cerebellum can cause trouble with Balance, coordination, and loss of movement control. This means that your nervous system may not be able to coordinate and balance properly, which is a condition known as ataxia.
Does cerebellar ataxia affect eyesight?
Ataxia can make it difficult to maintain balance, have difficulty in walking, slurred speech, and vision problems mainly the ability to decide distances.





6 Comments