Medial tibial stress syndrome
Table of Contents
What is Medial tibial stress syndrome?
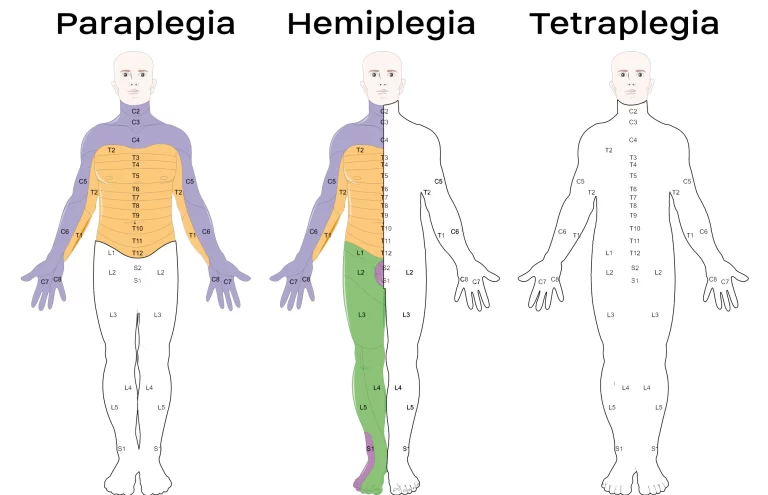
- Medial tibial stress syndrome (MTSS) is a frequent overuse of lower extremity injury in athletes or military personnel. MTSS is exercise-induced pain over the anterior tibia(shin area) or is an early stress injury in the continuum of tibial stress fractures.
Epidemiology
- The incidence of medial tibial stress syndrome ranges between 13.6% to 20% in runners or up to 35% in military recruits. Increasing loads, volume, and high-impact exercises can predispose to MTSS or bone stress injury. Intrinsic risk factors include improved female gender, previous history of MTSS, high BMI, navicular drop (a measure of arch height or foot pronation), ankle plantar flexion range of motion, or hip external rotation range of motion. Studies in military basic training recruits have linked vitamin D deficiency to an improved risk of stress injury.
Pathophysiology
- The underlying pathophysiologic process resulting in the MTSS is related to unrepaired microdamage accumulation in the cortical bone of the distal tibia. There is typically an overlying periostitis at the sites of bony injury, which also correlates with the tendinous attachments of the soleus, flexor digitorum longus, or posterior tibialis. Given the mechanical connections of Sharpey’s fibers, which are perforating fibers of connective tissue linking the periosteum to the bone, the belief is that repetitive muscle traction may be the underlying cause of the periostitis or cortical microtrauma. However, it remains unclear if periostitis occurs before cortical microtrauma and vice versa.
Definition of medial tibial stress syndrome
- Medial tibial stress syndrome (MTSS) is an overuse injury and repetitive-stress injury of the shin area. Various stress reactions of the tibia or surrounding musculature occur when the body is unable to heal properly in response to repetitive muscle contractions or tibial strain.
What are the Causes of Medial tibial stress syndrome?
- Shin splints are caused by repetitive stress on the shinbone or the connective tissues that attach your muscles to the bone.
Symptoms of Medial tibial stress syndrome
- vague, diffuse pain along the middle-distal tibia that is reduced with running (early stage) differentiates from exertional compartment syndrome, for which pain increases with running earlier onset of pain with many frequent training (later stages)
- tenderness along the posteromedial borders of the tibia
- 4cm proximal to the medial malleolus, extending proximally up to 12cm
- Flat Foot (pes planus)
- tight Achilles tendon
- weak core muscles
- provocative test
- pain on the resisted plantar flexion
Radiographic features
Plain radiograph
- For medial tibial stress syndrome, plain radiographs are considered insensitive or are often normal. It may, however, demonstrate a subtle periosteal reaction and callus around the cortex of the tibia medially 11.
CT Scan
- CT Scan is not particularly sensitive for the medial tibial stress syndrome (~40%) 3. It may reveal mild osteopenia as an early sign of fatigue damage of the cortical bone in tibial diaphysis 3,4.
Ultrasound
- Medial tibial stress syndrome may show focal hyperechoic elevation of the periosteum with irregularity over the distal tibia or improved flow on Doppler interrogation.
MRI
- MRI is the more sensitive radiological examination (~88%) for medial tibial stress syndrome 3. It may demonstrate a spectrum of findings ranging from normal to periosteal fluid or marrow edema in medial tibial stress syndrome to a complete stress fracture 5. The medial cortex (+/- posterior cortex) is commonly affected 3. The axial fluid-sensitive, fat-saturated sequences are often the many helpful.
Differential Diagnosis
- Anterior tibial stress syndrome
- Medial tibial stress syndrome
- Tibial/fibular stress fracture
- Exertional compartment syndrome
- Leg Tendinopathy
- Sural or SPN entrapment
Treatment of Medial tibial stress syndrome
Navicular drop test
- Management of MTSS is conservative, focusing on rest or activity modification with less repetitive, load-bearing exercise. No specific recommendations on the duration of rest required for the resolution of symptoms, or it is likely variable depending on the individual.
- Other therapies stay (with low-quality evidence) include iontophoresis, phonophoresis, ice massage, ultrasound therapy, periosteal pecking, and extracorporeal shockwave therapy. A main study on naval recruits showed prefabricated Introduction to Orthotics reduced MTSS.
Physical Therapy Management
- Patient education or a graded loading exposure program seems the most logical treatment. Conservative therapy should initially aim to correct functional gait or biomechanical overload factors. Recently ‘running retraining’ has been advocated as a promising treatment strategy or a graded running program has been suggested as a gradual tissue-loading intervention.
- Prevention of MTSS was investigated in a few studies or shock-absorbing insoles, pronation control insoles, or graduated running programs were advocated.
- Over-stress avoidance is the main preventive measure for MTSS or shin splints. The main goals of shin-splints treatment are pain relief and a return to pain-free activities.
Acute phase
- 2-6 weeks of rest combined with medication is recommended to improve the symptoms and for a quick or safe return after a period of rest. NSAIDs or Acetaminophen are often used for analgesia. Also, cryotherapy with Ice-packs and eventually analgesic gels can be used after exercise for a period of only 20 minutes.
- There are a number of physical therapy modalities to use in the acute phase but there is no proof that these therapies such as ultrasound, soft tissue mobilization, or electrical stimulation would be effective. A corticoid injection is contraindicated because the can give a worse sense of health. Because the healthy tissue also must be treated. A corticoid injection is given to decrease the pain, but only in connection with rest. Prolonged rest is mainly not ideal for an athlete.
Subacute phase
- The treatment should aim to modify training conditions or address eventual biomechanical abnormalities. Changes in training conditions could be reduced running distance, intensity, or frequency and intensity by 50%. It is advised to avoid hills or uneven surfaces.
- During the rehabilitation period, the patient can do less-impact or cross-training exercises (like running on a hydro-gym machine). After a few weeks, athletes may slowly improve training intensity and duration or add sport-specific activities, or hill running to their rehabilitation program as long as they remain pain-free.
- A stretching or strengthening (eccentric) calf exercise program can be introduced to prevent muscle fatigue. Patients also benefit from strengthening mainly core hip muscles. Developing core stability with strong abdominal, gluteal, or hip muscles can increase running mechanics and prevent lower-extremity overuse injuries.
- Proprioceptive balance training is crucial in neuromuscular condition education. This can be done with a one-legged stand and balance board. Improved proprioception will improve the efficiency of joint or postural-stabilizing muscles and help the body react to running surface incongruities, also key in preventing re-injury.
- Choosing good shoes with good shock absorption can help to prevent a new and re-injury. Therefore it is important to change the athlete’s shoes every 250-500 miles, a distance at which most shoes lose up to mainly 40% of their shock-absorbing capabilities. In the case of biomechanical problems of the foot, individuals may benefit from an Introduction to mainly Orthotics. An over-the-counter orthosis (flexible or semi-rigid) can help with excessive foot pronation or pes planus. A cast and a pneumatic brace can be necessary in severe cases.
- Manual therapy can be used to control several biomechanical abnormalities of the spine, the Sacroiliac joint, and various muscle imbalances. They are often used to prevent relapsing from the old injury. There are also acupuncture, ultrasound therapy injections, and extracorporeal shock-wave therapy but their efficiency is not yet proven.
FAQ
Medically also known as medial tibial stress syndrome, shin splints often occur in athletes who have recently intensified and changed their training routines. The improved activity overworks the muscles, tendons, and bone tissue.
These include how long you have had your symptoms, the location of the bone injury and fracture, your previous activity levels, or other factors that are specific to you. However, as a general guideline, bone can take up main to 6 weeks to heal. The majority of people get back to the sport and their activities within 10-16 weeks.
The most common muscles involved in MTSS are the posterior tibialis, flexor digitorum, or soleus muscles. These muscles primarily help stabilize the lower leg or foot and aid in pushing off while running. Another muscle more commonly involved is the tibialis anterior muscle.
Your physiotherapist will assess the severity of the injury or then focus on reducing pain and inflammation. The therapist will also help determine the cause of the shin splints (for example, improper biomechanics, overuse, and others) so an appropriate treatment plan can be developed.
Although often not serious, it can be quite disabling or progress to more serious complications if not treated properly. Often, the cause of MTSS is multi-factorial and involves training errors or various biomechanical abnormalities.




One Comment