Tetraplegia
Table of Contents
What is tetraplegia?
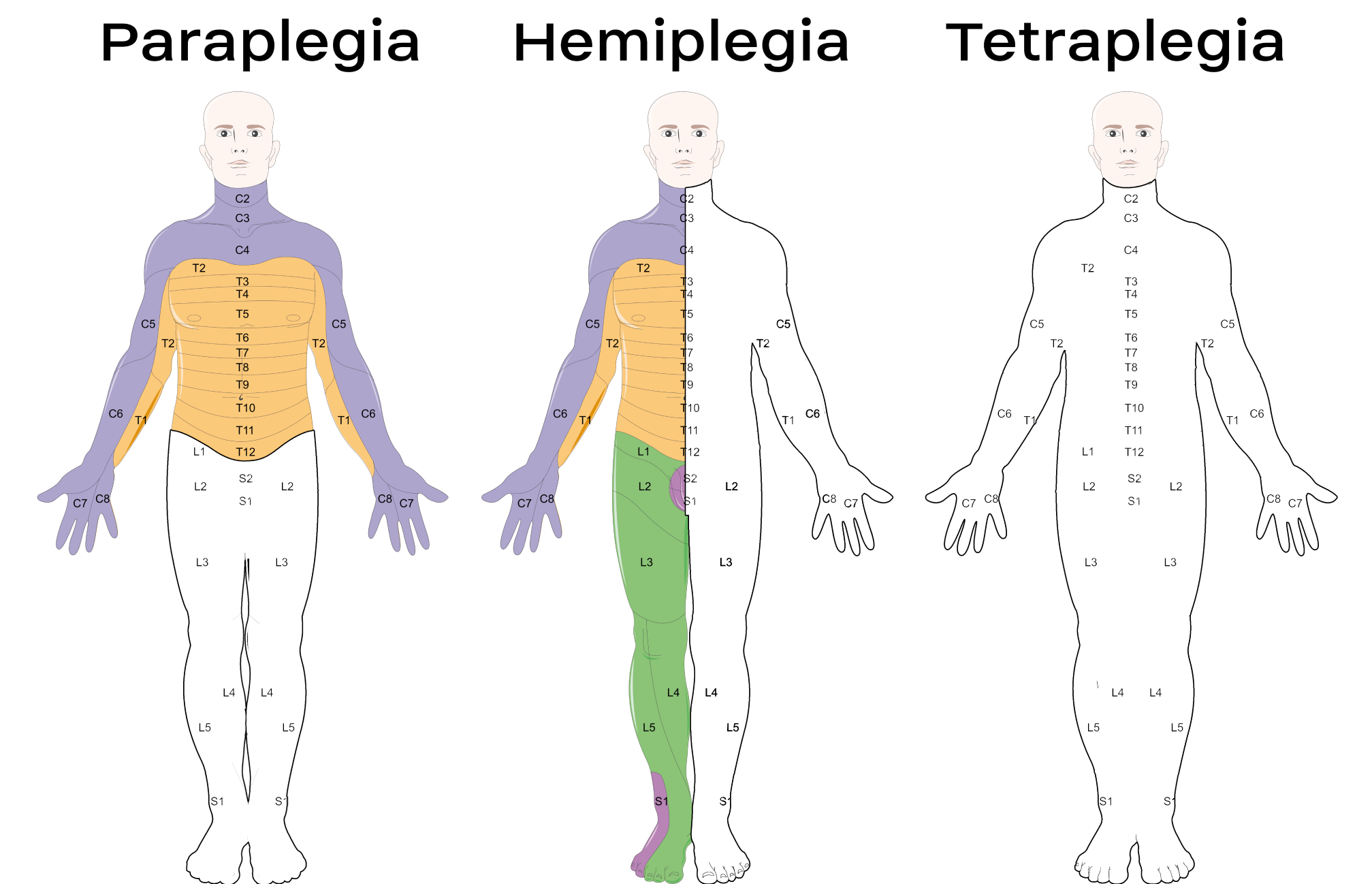
Tetraplegia is a type of paralysis that results in the loss of movements and sensations in all four limbs.
It affects all four limbs, and in some people, it also affects parts of the chest, abdomen, and back.
Signs and Symptoms:
The main symptom is paralysis. It may cause severe impairments to mobility, and it can have a major impact on a person’s ability to perform daily tasks. The patient is unable to walk and needs a wheelchair.
They may also be not able to bathe, dress, or eat without assistance. This can severely restrict a person’s independence.
Depressed functioning and immobility, people with tetraplegia often have more complications such as pressure sores, osteoporosis and fractures, frozen joints, spasticity, respiratory difficulties, infections, autonomic dysreflexia, deep vein thrombosis, and cardiovascular disease.
What are the Causes of Tetraplegia?
Tetraplegia is caused by injury to the brain or the spinal cord. The injury, which is called a lesion, causes the loss of half or total function of all four limbs, meaning the arms and the legs.
Some possible causes of such damage include:
Falls or injuries(from the vehicle or sporting accidents)
Autoimmune diseases, such as multiple sclerosis or Guillain-Barre syndrome(GBS)
Neurological conditions, such as stroke.Tumors and lesions in the brain or spinal cord injury.Neurological conditions, such as cerebral palsy.Spinal cord infections, such as due to polio.
Diagnosis:
To diagnose tetraplegia, a doctor would check the person’s symptoms and medical history. For example, they may ask questions about any recent accidents or trauma, or they might ask if the person has any family history of such conditions or medical conditions such as blood pressure.
It is important that the doctor establish the cause of the tetraplegia to determine suitable treatment options for the patient.
The diagnosis would also include some tests to check the damage and the functioning of the muscles and nerves in the body.
Tests will involve medical imaging such as an MRI scan, a CT scan, or an X-ray. To test nerve functioning, the doctor may use electromyography, which measures the body’s responses to the stimulation of the muscles.
Treatment of Tetraplegia
Medical Treatment
Paralysis is not totally curable. However, treatment may help people regain partial or complete control over the affected areas. Treatment may also help decrease some of the symptoms and difficulties.
The treatment may vary depending on the cause:
For example, If the paralysis is due to an autoimmune disease, a doctor might prescribe immunosuppressant drugs. Doctors also prescribe medicines to help with the pain and to relax the affected muscle which may also be necessary to decrease muscle atrophy. Sometimes people with tetraplegia cannot able to speak normally, so in such cases, a doctor may give treatment such as speech therapy to help. Wheelchairs and other assistive devices can build on a person’s mobility. Some surgeries such as stem cell therapy and nerve transfer surgery may help people regain some control over their movement or affected areas.
Physical Therapy Treatment in Tetraplegia
Physical therapy is generally recommended to keep muscles and joints as strong and mobile as possible. Usually, someone who experiences an injury that causes tetraplegia is put into a lengthy rehabilitation program that includes physical therapy to learn how to adjust to daily life with a change in:
- Mobility
- Function
- Independence
The ability to use the limbs is considered important to regain independence.
Task-specific training with functional electrical stimulation (for e.g. if the grasp function is too weak) is to help the hand use.
The physiotherapist’s task will be to strengthen the muscle and teach the patient to control his muscle individually.
Different techniques such as
- Use of functional electrical stimulation
- Lower extremities cycling, treadmill gait
- Electrical stimulation during gait is used to regain or maintain muscle mass in the legs and strengthen the bones.
- Stretching
- Strengthening of weakened muscles
- Improve muscle tone
- Improve balance and posture
- Circulatory exercises before standing up may be helpful to stimulate blood flow in the body
The management of a person with a Spinal Cord Injury can be divided into 3 Phases;
- Acute
- Sub-acute (Rehabilitation)
- Chronic (Long Term)
During the acute and subacute phases of treatment, rehabilitation strategies focus more on the prevention of secondary complications and promoting neuro recovery, addressing underlying impairments, and improving function. In the chronic phase, assistive approaches are often used.
Acute Phase
In the acute phase, prevention of complications arising from spinal instability or neurological compromise is the main aim. In this early phase post-injury, physiotherapy management is mainly involved in the prevention and management of respiratory and circulatory problems, as well as minimizing the effect of immobilization on the patient e.g. pressure ulcer – and deep vein thrombosis development.
Objectives:
Treatment objectives in the acute phase include:
- To manage respiratory conditions and any complications as a result of the spinal cord injury e.g. improve breathing, and enhance clearance of secretion.
- To maintain the full range of movement of all the joints within the limitations seeing the stability of the fracture.
- To monitor the neurological status.
- To maintain and strengthen all unaffected muscle groups to support and educate the patient, carers, family, and staff about the condition.
Respiratory Function
Common secondary complications include hypoventilation, atelectasis, secretion retention, cough, and pneumonia.
The respiratory function is affected due to damage in the spinal cord relevant to the neurological level of the spinal cord injury.
Physiotherapy interventions should always include clearing of secretion and increased ventilatory techniques.
Secretion clearance techniques such as percussions, vibrations, and shaking, as well as postural drainage and suctioning.
Treatment to improve breathing includes abdominal binders, positioning, deep breathing exercises, incentive spirometry, and inspiratory muscle training.
Range of movement for all joints
Reduced ROM may cause contractures or shorten due to immobility and poor positioning, as well as increased tone and spasticity.
Treatment techniques should include:
1. Passive stretches,
2. Positioning in the lengthened position
3. Other common Tone increase treatment techniques such as compression, heat, and sustained deep pressure.
Prevention of Pressure Ulcers
Areas prone to pressure ulcers include; the occiput, scapulas, sacrum, and heels when lying in supine and the same position for a long period, While the greater trochanter and malleoli are more prone in side-lying.
In the acute phase, interventions include passive care, such as frequent rolling technique and mobilizing, as well as adequate skin moisturizing, massage, nutrition, and monitoring.
Later, in the sub-acute and long-term phases, individuals will be taught how to do the frequent self-lift technique in order to relieve pressure.
Maintaining and strengthening innervated muscles
Progressive resistance training and functional strength training are clinically identified to achieve favorable results in maintaining and strengthening innervated muscle groups.
Dosage for strengthening (progressive resistance training):
one to three sets of 8-12 reps (rest 1-3mins between per set)
load 60-70% of one-repetition maximum
2-3 times per week
In order to target endurance; decrease weight and increase repetitions.
Sub-acute (Rehabilitation) Phase
The rehabilitation needs of individuals with an SCI are best at a specialized Spinal Cord Injury Unit, but often rehabilitation begins in the Acute or Trauma Hospital while the individual is awaiting transfer to a Spinal Injuries Unit. Rehabilitation requires consideration of the whole person; their physical, psychological, educational, vocational, and social background. The rehabilitation process is a goal-based, and time-limited process aimed at facilitating maximum independence and optimal reintegration back into the individual’s normal role and lifestyle.
Physiotherapy is the most important component during the rehabilitation process following spinal cord injury and includes a variety of interventions to get the individual back to his normal life. Quality of Life including community participation, gainful employment, interpersonal relationships, and can-do activities have become the overriding focus of management.
Objectives:
Treatment objectives of the rehabilitation phase include:
- To address physical motor functional activities
- Management to prevent further problems
- To improve individual independence in ADL, such as bathing, eating, dressing, grooming, and mobility
- To achieve functional independence, using pieces of equipment
- To achieve successful reintegration into the community.
The range of movement activities used by physiotherapists during rehabilitation varies, depending on the level of injury and type of injury.
The three most common individual therapy for individuals with high-level tetraplegia were:
- range of movement/stretching,
- strengthening, and
- transfers;
Range of movement of all joints and movement
UPPER LIMB
- Shoulder: Flexion, Extension, Rotation
- Elbow: Flexion Extension
- Wrist: Flexion, Extension, Rotation
- Finger movements
LOWER LIMB
- Hip: Flexion, Extension, Rotation
- Knee: Flexion Extension
- Ankle: DorsiFlexion, Plantarflexion, Rotation
- Toes movements

While for those with low tetraplegia, more effort is on transfers than strengthening.
In order to perform motor tasks successfully individuals should have proper strength, balance, ROM, and knowledge regarding the specific motor tasks. All these can be achieved through frequent progressive training.
Bed mobility and transfers
C6 and lower level of SPINAL CORD INJURY have the ability to attain 5 motor skills;
- rolling (using momentum)
- mobilizing from supine to long-sitting
- unsupported sitting (short & long sitting)
- lifting vertically
- transfers
C6 tetraplegia may have some difficulties, but these 5 motor skills are still possible with some modifications. With rolling, C6 tetraplegia should laterally rotate their shoulders and swing their arms across their body instead of over-head. During an unsupported sitting, C6 tetraplegia should laterally rotate shoulders and lock elbows in extension to maintain balance. Vertical lifting for individuals with C6 tetraplegia can be possible by passively extending elbows, laterally rotating shoulders, and depressing shoulders to weight bear with hands placed anteriorly to the pelvis.
Wheelchair mobility
Individuals with C1-C4 tetraplegia require powered-WheelChairs(WC). These WCs may be controlled by chin movements, sip, puff, or head array.
Individuals with C5 tetraplegia most commonly use powered-WCs controlled by wrist and hand movement. Most individuals with C6-8 tetraplegia can be able to independently mobilize with manual WC, however, might use a hand-controlled WC as optional.
Individuals with Spinal cord injury lower than C8 would be able to independently mobilize with the use of manual WC.
Individuals with Spinal cord injury should be orientated to their new way of mobilization. Turning, opening and closing doors, going up and down inclines, going around and over obstacles, as well as mobilizing indoors and outdoors are important activities to practice in order to ensure safe and independent mobility.
Gait and standing

Gait training, strengthening, and balance exercises are the most common physiotherapy activities in individuals with spinal cord injuries. Overall, strengthening is the most common group therapy activity across all levels and types of spinal cord injury.
Spasticity Management
For this, a therapist works on
-Active ROM (Range of Motion)
-Stretching
-MAT Exercise: For weight bearing
Sit-to-stand activities with assistance and then independent
Bridging, rolling, half kneeling, quadruped
The ability to stand or walk is dependent on several factors however, standing has many benefits even if independent standing might not be possible. Benefits include emotional well-being, orthostatic hypotension, bone mineral density, spasticity, bladder, and bowel function improvement.
Standing can be achieved by using assistive devices such as; tilt tables, standing Wheelchairs, and/ or standing frames. Individuals might be able to stand in parallel bars using knee-extension splints or orthoses.
Gait training is possible among individuals with complete paralysis to partially paralyzed lower extremities by using orthoses and walking aids such as; knee-ankle-foot and hip-knee-ankle-foot orthoses.
- Normal Walking
- Parallel bar walking
- shuffle gait
- Sidewalk
- Forward and backward
- Stepping activities
- Pertubation
- Walking on footprint
Balancing:
Wall standing with an open and then closed eye
-Eyes close walking
-Obstacle walking
-Pertubation
Biofeedback
Functional training
The main aim is to assist individuals to perform ADL
-For feeding and eating( utensil with modified handle, rocker knife, wrist splint, cuff)
-For self-care and bathing (shower tubs, hand-held shower, raised toilet seat, elastic toothbrush, bathing benches)
-For the dressing (zipper, hooks, buttons, velcro straps, elastic shoelaces).
Long Term Phase
Individuals with an SCI, depending on the level and type of injury, may have many complex needs and face wide-ranging, long-term restrictions in their ability to live independently, drive a vehicle or use public transport, return to work or education, and participate in leisure and social activities and functions.
To ensure successful long-term management coordinated community rehabilitation services and long-term support is needed to meet the long-term and ongoing requirement of individuals with a spinal cord injury.
Objectives:
Treatment objectives of the long-term phase include:
1. To achieve high-level mobility aims required for community participation
2. To monitor the recovery of function and improvement
3. To Educate family and carer training
Outlook
There are currently no ways to treat paralysis in tetraplegia. Therefore, people with tetraplegia need lifelong care.
However, by using a range of treatments and management techniques, some people may be able to achieve partial or complete control over the affected extremity.
In many cases, people with tetraplegia would need lifelong help with most daily activities, such as eating, clothing, and using the bathroom. They are generally unable to live independently.
Psychotherapy and family therapies may help patients with the psychological impacts of tetraplegia. Ongoing physical therapy and medication may be necessary to help a person deal with other difficulties that occur over.
People with tetraplegia might experience difficulties over time, such as tightness. They generally need daily care and treatment. It is not currently curable, but treatment may help people regain or achieve partial or complete control over the affected areas and extremities.
FAQ
What is tetraplegia vs quadriplegia?
The terms “quadriplegia” and “tetraplegia” means the same thing: paralysis below the neck that affects all of a person’s four limbs. The reason that there are two words with the same meaning is because of differences in ancient languages.
Can you recover from tetraplegic?
It is possible for some people to get the recovery and can achieve some function up to 18 months after the injury. However, many people will experience a permanent loss of movement that requires long-term care.
Can someone with a tetraplegic walk?
Most people with tetraplegia have significant paralysis below the neck, and many are completely not able to move.
Why do people get tetraplegic?
Damage to the brain, spinal cord, or both is the main cause of tetraplegia. The brain and spinal cord normally pass signals to muscles around the body to perform a movement. Damage to the brain or spinal cord disrupts this signal and muscle can not perform its function. If the damage is severe enough, it causes tetraplegia.
What is the difference between tetraplegia and tetraparesis?
Tetraplegia (quadraplegia) refers to paralysis (loss of voluntary motor function in the limbs). Similar involvement of all four limbs is termed tetraparesis, in which paresis means weakness.




2 Comments