SPASTICITY TREATMENT :
Table of Contents
What is a Spasticity?
- Spasticity is motor disorder characterised by a velocity dependent increase in tonic stretch reflexes (muscle tone) with exaggerated tendon jerks, resulting from hyperexcitability of the stretch reflex, as one component of the upper motor neurone syndrome.
- The most well-known and referenced description of spasticity is the physiological definition proposed by Lance in 1980.
- ‘Spasticity is a motor disorder characterised by a velocity-dependent increase in tonic stretch reflexes (muscle tone) with exaggerated tendon jerks, resulting from hyperexcitability of the stretch reflex, as one component of the upper motor neurone syndrome’.
- Disordered sensorimotor control, resulting, resulting from an upper motor neuron lesion (UMN), presenting as an intermittent or sustained involuntary activations of muscles.
- Spasticity can cause significant problems with activity and participation in people with a variety of neurological disorders.
- spasticity is only one of the many different features of the upper motor neurone (UMN)syndrome.
- A characteristic feature of spasticity is that the hypertonia is dependent upon the velocity of the muscle stretch – in other words, greater resistance is felt with faster stretches (this results in the clinical sign of a ‘spastic catch’). Thus, spasticity resists muscle stretch and lengthening. This has two significant consequences. First, the muscle has a tendency to remain in a shortened position for prolonged periods, which in turn may result in soft tissue changes and eventually contractures . The second consequence is that attempted movements are obviously restricted. If, for example, the individual attempts to extend the elbow by activation of the triceps, this will stretch the biceps, which in turn will induce an increase in resistance and indeed may prevent full extension of the elbow. However, it is worth emphasizing that the situation is usually more complex. In the above example, relief of the spasticity in the biceps may not lead to improvement in the function of the arm, as other features of the UMN syndrome, particularly muscle weakness, may have a part to play.
- Spasticity is generally caused by damage or disruption to the area of the brain and spinal cord that are responsible for controlling muscle and stretch reflexes. These disruptions can be due to an imbalance in the inhibitory and excitatory signals sent to the muscles, causing them to lock in place. Upper motor neuron lesions causes the spasticity.
Anatomy and Etiology:
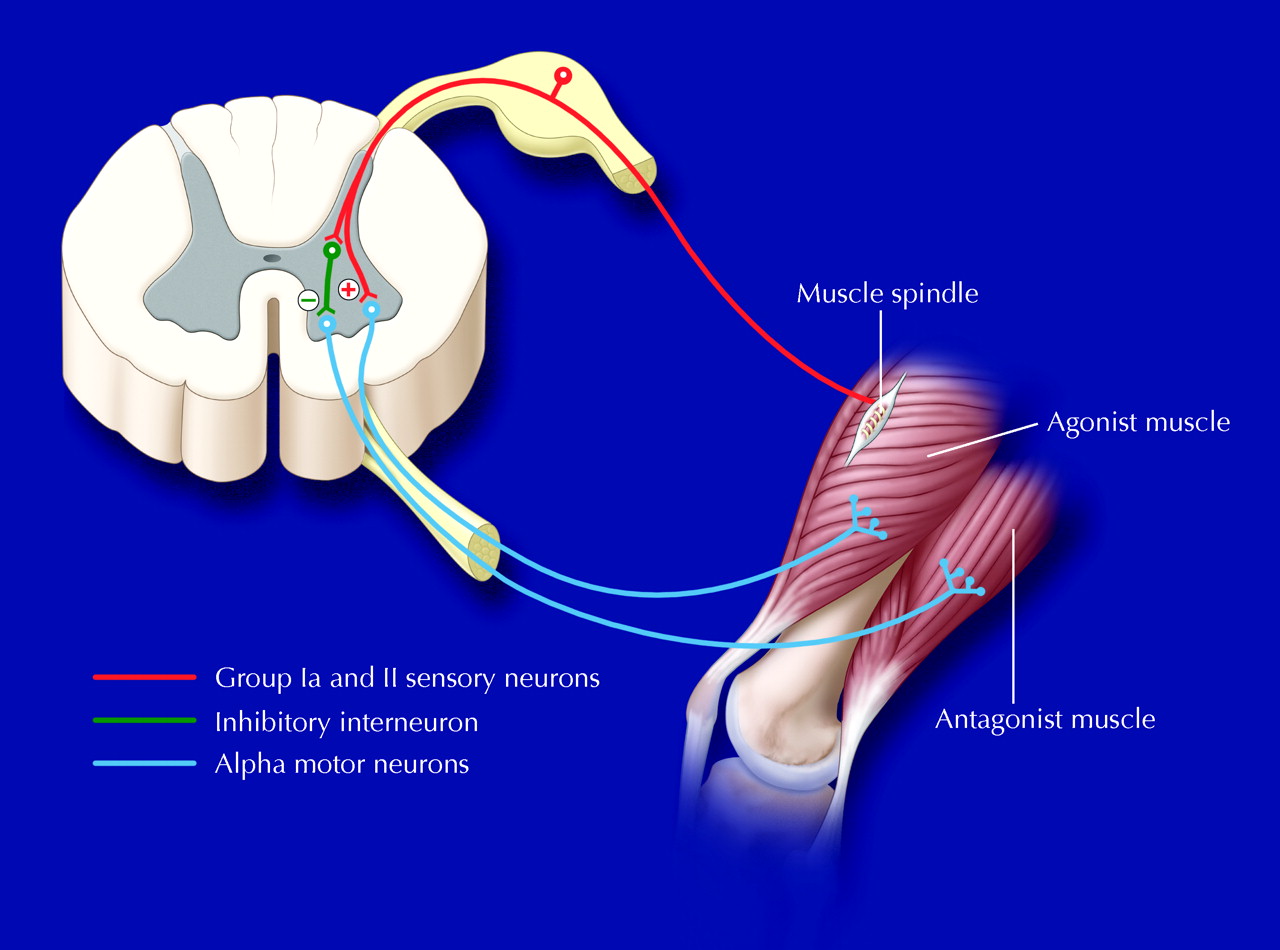
- A UMN injury leads to loss of inhibition downstream and hypersensitivity of the reflex arc within the spinal cord
- Primary impairments from an upper motor neuron lesion (UMNL) are usually due to the disruption of supraspinal control of descending pathways that control excitatory and inhibitory influences on proprioceptive, cutaneous and nociceptive spinal reflexes.
The Inhibitory System
- Corticoreticular Spinal Tract: These tracts travel with, but are separate from, the Corticospinal Tract, and are responsible for the facilitation of the inhibitory area within the medulla called the ventromedial reticular formation. Here, the Dorsal Reticulospinal Tract originates, which is responsible for an inhibitory action on both the stretch and flexor reflexes.
The Excitatory System
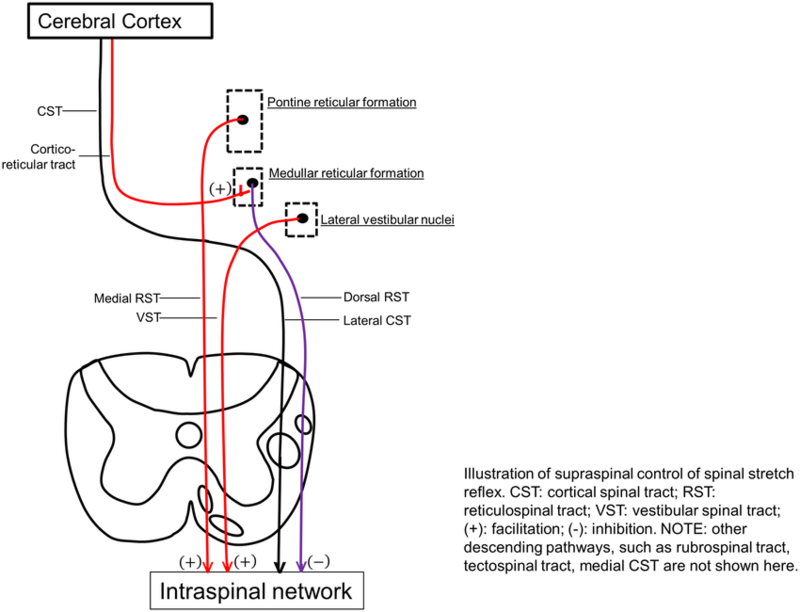
- The bulbopontine tegmentum gives rise to the Medial Reticulospinal Tract and, acting weakly with the Vestibulospinal Tract, is excitatory to both stretch and extensor reflexes and like the Dorsal Reticulospinal Tract, is also inhibitory to the flexor reflexes.
Different Lesions and Their Presentations:
- The signs and symptoms between Cortical UMN Lesions and Spinal Cord UMN Lesions vary due to the location of where the disruption has taken place.
Normal
- Both the inhibitory system (Corticospinal Tract and Dorsoreticulospinal Tract) and excitatory systems (Medial Reticulospinal and Vestibulospinal Tract) are in dynamic balance and therefore the inhibition to the spinal cord is easily adjusted according to demand.
Corticospinal Tract Lesion
- Although the Corticospinal Tract has an inhibitory influence on stretch and flexor reflex, the main inhibitory system produced by the Dorsal Reticulospinal Tract remains intact and therefore the balance of excitatory and inhibitory influences are maintained.
Internal Capsule Lesion
- Leads to interruption of both the Corticospinal Tract and Corticoreticular Tract pathways that are responsible for the inhibitory response and some loss of inhibition to stretch and flexor stretches. The excitatory systems from both the Medial Reticulospinal and Vestibulospinal Tract are more dominant which leads to the facilitation of extensor and stretch reflexes but inhibition of flexors.
Incomplete Spinal Cord Lesion
- Signs and symptoms will vary dependant on site and extent. If the inhibitory system is affected then there will be an unopposed excitatory drive to stretch and extensor reflexes with partial inhibition of flexor reflexes.
Complete Spinal Cord Lesion
- Spinal reflexes are unopposed due to the complete loss of supraspinal control. Both flexor and extensor reflexes are disinhibited and therefore people may experience both flexor and extensor spasms.
Spasticity Symptoms:
- Symptoms of spasticity can vary from being mild stiffness or tightening of muscles to painful and uncontrollable spasms. Pain or tightness in joints is also common in spasticity.

- Muscle stiffness, causing movements to be less precise and making certain tasks difficult to perform.
Muscle spasms, causing uncontrollable and often painful muscle contractions.
Involuntary crossing of the legs.
Muscle and joint deformities.
Muscle fatigue.
Inhibition of longitudinal muscle growth.
Inhibition of protein synthesis in muscle cells.
CLINICAL PRESENTATION:
- Mobility:
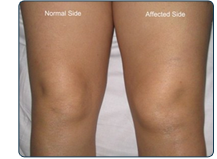
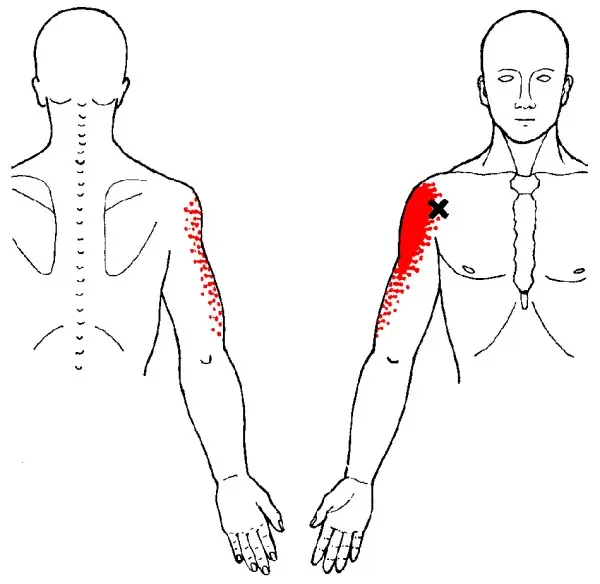
- High muscle tone in muscle groups such as the shoulder adductors, elbow, wrist, and finger flexors, and forearm pronators. In the lower extremities, the increased tone is especially prominent in the hip adductors, knee flexors and extensors, and plantar flexors and invertors of the ankle. Antigravity muscles are predominantly affected.
- Probably the most common consequence of the UMN syndrome is difficulty walking. The gait can be clumsy and uncoordinated, and falling can become a common event. Eventually walking may become impossible owing to a combination of soft tissue contractures, flexor or extensor spasms and unhelpful associated reactions.
- Even if the individual cannot walk, the UMN syndrome can cause further problems with regard to difficulty maintaining a suitable seating posture. Spasticity may make it difficult to self-propel a wheelchair.
- Extensor spasms may constantly thrust the individual forward while sitting in the chair, giving rise to an increased risk of shear forces that can cause pressure sores. Seating will often require a considerable range of bracing, supports and adjustments in order to allow the person to maintain a useful and comfortable position.
- Loss of dexterity:
- In the arm, the UMN syndrome can cause further difficulties with, for example, feeding, writing, personal care and self-catheterization. Mobility in bed may be hampered and loss of dexterity in the arm may make it difficult to self-ambulate in a wheelchair. All these problems can slowly lead to decreased independence and a consequent increased reliance on a third party.
- Patients may report difficulty with footwear if their spasticity involves constant, high tone of the extensor hallucis longus or long toe flexors.
- Bulbar and trunk problems:
- Although most of the functional consequences of spasticity occur in the arm or leg, it is worth remembering that truncal spasticity can cause problems with seating and maintaining an upright posture – necessary for feeding and communication. Bulbar problems can give rise to difficulty swallowing, with consequent risk of aspiration or pneumonia. Further problems can arise with communication, secondary not only to inappropriate posture but also to spastic forms of dysarthria.
- Pain:
- It is not widely recognized that spasticity and the other forms of UMN syndrome can be extremely painful. This is particularly the case with flexor and extensor spasms, and sometimes treatment is needed simply for analgesia rather than improvement of function. Abnormal postures can also give rise to an increased risk of musculoskeletal problems and osteoarthritic change in the joints. Any peripheral stimuli from problems such as ingrowing toenails or small pressure sores can, in turn, exacerbate the spasticity, and a vicious circle of increased pain and increased spasticity can ensue.
- Spasticity varies with speed of movement (velocity dependent); meaning the faster the muscle is moved or stretched, the greater the resistance to stretch or passive elongation is felt.
- Clonus, spastic co-contractions, and spastic dystonia may be evident. i.e., Clonus is defined as an alternating muscle contraction and relaxation of the agonist and antagonist muscles. Spastic co-contractions are abnormal antagonist contractions that present during voluntary agonist effort. Spastic dystonia is a muscle contraction that is present at rest, leading to a constant clinical posture that is highly sensitive to stretch.
- Clasp knife phenomenon: Limb initially resists movement and then suddenly gives way .
- Stroking Effect: Stroking the surface of the antagonist muscle may reduce tone in spasticity.
- Permanent loss of joint range has been known to occur 3-6 weeks after both stroke and brain injury and therefore it is important that spasticity is identified early on in the assessment in order for it to be monitored and managed as required.
- In a person with hemiplegia the lower limb pattern is plantar flexion and inversion of the ankle with hamstring tightness limiting knee range of motion as well as adductor spasticity. Upper limb presentation is usually shoulder adduction, internal rotation, elbow flexion, forearm pronation with wrist and elbow flexion.
DIAGNOSIS:
Neurophysiological approaches to measurement:
- The three common techniques that have been used for clinical quantification are spasticity tendon jerks, H-reflex
- studies, and F-wave studies.
Tendon jerks :
- The most commonly used method to illustrate a spinal reflex is the tendon jerk that is obtained by a rapid (but small) stretch of a muscle. The ensuing response is reported primarily to involve the monosynaptic pathway, although it has also been suggested that this action could be influenced by oligosynaptic pathways . It has been reported that tendon jerks are more readily elicited in people with spasticity, i.e. they can be elicited with smaller levels of stimuli than normal, and the response to these stimuli has a higher amplitude and is more diffuse – that is, it can involve muscles which were not originally stimulated). Therefore, it has been hypothesised that the tendon jerk can be a quantifiable measure of spasticity. However, it is important to note that increase in tendon jerk is not exclusive to spasticity. Furthermore, whether the increase in the tendon jerk response is related to increased gain, decreased threshold or a combination of both needs to be resolved.
H – REFLEX
- The H reflex is a long-latency reflex obtained by electrically stimulating a mixed nerve submaximally. The
- muscle response that follows results from conduction via the Ia afferent pathways. Although these
- reflexes are thought of as being primarily monosynaptic, there is evidence that oligosynaptic reflex pathways could also be involved.In order to normalize for this variability, the H-reflex response has been
- expressed as a percentage of the M-response (i.e. the stimulus of a muscle to supramaximal stimulation).
- It should be noted that when using this ratio, there is an assumption that the presynaptic component in the reflex response is fixed. While there are reports that H/M ratios are increased in spasticity, it has also been demonstrated that the ratios did not decrease following treatment of spasticity. It has also been reported that the correlation between
- H/M ratios and the severity of spastic hyperreflexia was poor .Since, in normal subjects, the vibration of muscle inhibits
- H-reflex activity, it has been hypothesised that, in spastic limbs, this inhibition should be reduced.
F waves
- F waves are obtained by the supramaximal stimulation of a mixed nerve and have been used as a measure of -motor neurone excitability. Unlike H reflexes, the F wave does not result from stimulation of a sensory nerve but from the antidormic stimulation of the -motor neurone. Furthermore, unlike the H reflex that shows an inverse relationship with the M wave, the F wave, which follows the M wave, shows no correlation with M-wave amplitudes. In addition, the amplitude of the Fwave is much smaller than that of the H reflex. Although the F wave provides a more stable signal which is less influenced by resting posture and the ability of a subject to relax, the average F-wave response from repeated tests is often used because of variations in latency and amplitude. It has been demonstrated that spastic subjects show increased F-wave amplitudes, suggesting increased motor neuronal excitability.
Outcome measures :
Useful objective measures to monitor changes in spasticity can include:
Subjective:
- Pain:
- Numeric Pain Scale (e.g. for pain, comfort, stiffness)
- Observing grimacing / pulling away
- Arm A and Arm B
- LegA
Objective:
- Resting position: photographs, description, measuring bony landmarks
- Passive range of movement
- Adductor Tone Rating
- Active range of movement
- Muscle strength: Oxford Scale
- Spasms:
- Modified Penn Spasm Frequency Scale
- Clonus and Spasm Score
- Function :
- Walking: 10m times walk
- Transfers: Times up and go
- Upper Limb Function: 9 hole peg test
- Speech: Speech comprehension score
- Walking and Falls Score
- Muscle tone: Ashworth Scale / Modified Ashworth Scale
ASHWORTH SCALE :
- In the clinical setting, the most commonly used technique of measurement is the Ashworth scale .The Ashworth
- test is based upon the assessment of the resistance to passive stretch by the clinician who applies the
- movement.
- The scale is as follows:
- Ashworth Scale :

- Grade Description
- 0 No increase in muscle tone
- 1 Slight increase in tone giving a catch when the limb is moved
- 2 More marked increase in tone but limb easily moved
- 3 Considerable increase in tone – passive movement difficult
- 4 Limb is rigid in flexion or extension
MODIFIED ASHWORTH SCALE :
- Modified Ashworth Scale‘ scores exhibited better reliability when measuring upper extremities than lower. The scale is as below:
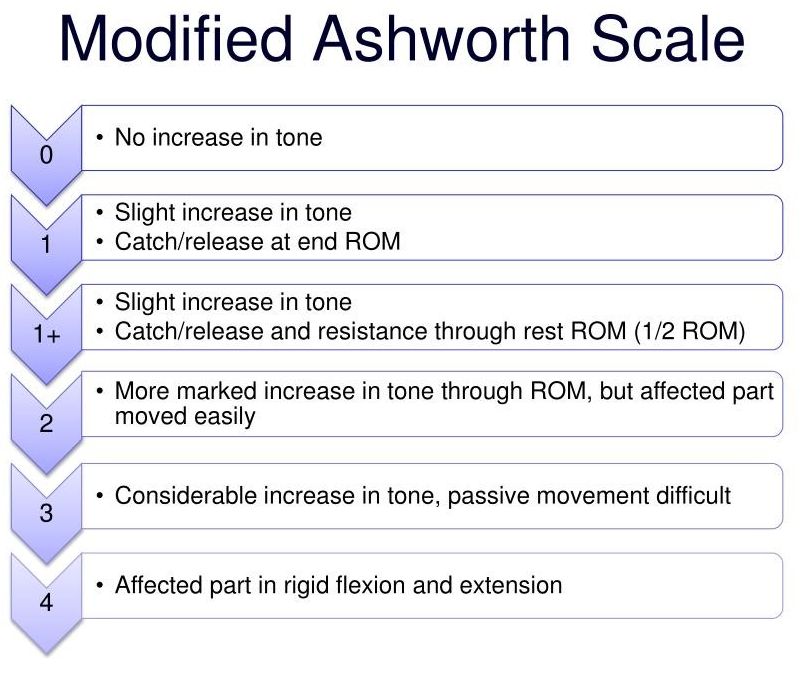
- Grade Description
0 No increase in muscle tone
1 Slight increase in muscle tone, manifested by a catch and release or by minimal resistance at the end of the range of motion when the affected parts is moved in flexion or extension - 1+ Slight increase in muscle tone, manifested by a catch, followed by minimal resistance throughout the remainder (less than half) of the ROM
2 More marked increase in muscle tone through most of the ROM, but affected part(s) easily moved
3 Considerable increase in muscle tone, passive movement difficult
4 Affected part(s) rigid in flexion or extension
DIFFERENCE BETWEEN SPASTICITY / RIGIDITY/ CONTRACTURE / STIFFNESS:DIFFERENCE BETWEEN SPASTICITY / RIGIDITY/ CONTRACTURE / STIFFNESS:
RIGIDITY :
- Rigidity seen in extra piramidal lesions ( ex. parkinson’ s Disease ) is such as the rubrospinsl / vestibulospinal tracts .
- subtypes include:-

- Cog wheel rigidity ( parkinson’s ) – tremor superimposed on this hypertonia that results in intermittent increase in tone during the movment.

- Lead pipe rigidity :– same resistance in all direction ( agonists & antagonist muscles both )
- Not velocity dependant – does not very with speed of movement of muscles groups involved .
CONTRACTURES :
- Spasticity & contactures are conditions in which muscles imbalance across a joint leads to abnormal positioning and tightness.
- Spasticity refers to involuntary tightening or stiffness of muscles.
- A contracute develops when the normally stretchy ( elastic ) tissues are replaced by nonstretchy ( inelastic ) fiber like tissue. This tissue makes it hard to stretch the area and prevents normal movement.
- Contracture are a loss of full active & passive ROM in a limb that vcan be due to limitations imposed by the joint,
- muscle or soft tissue.
- The term contracture refers to abnormal positioning of a joint.
Stiffness :
- Muscle stiffness is when your muscle feel tight and you find it more difficult to move than you usally do, especialy after rest.
- You may also have muscle pains, cramping and discomfort.
SPASTICITY TREATMENT :
Medical Treatment :
Some individuals may benefit from medications to manage spasticity. These can be generalised, focal or intrathecal interventions.
If the spasticity is widespread then systemic medication is used. This includes:
- Dantrolene (Dantrium)
Baclofen (Lioresal and others)
Tizanidine (Zanaflex)
Diazepam (Vallium)
Benzodiazepines
Gabapentin
Pregabalin
Canabinoids
If the spasticity is locallised then local medication is used. This includes: - Boutulinum Toxin (Botox)
Regional Nerve Block
Intrathecal medications can also be used. These include: - Baclofen
Phenol
Spasticity Surgical Treatment :
- Surgery for Spasticity:
- Selective dorsal rhizotomy for spasticity:
- Treatment for spasticity begins with non-invasive, nonsurgical approaches that may improve function and quality of life. When the spasticity is severe and chronic, however, surgery may be recommended as part of the treatment plan.
Orthopedic surgeries:
- Orthopedic surgeries may involve altering tendon, muscle, and bone to restore movement and flexibility, used to maintain function as a child grows.
Neurological surgeries:
- Neurological surgeries include a procedure called selective dorsal rhizotomy, in which the damaged nerves carrying sensory information from the spastic limbs are cut where they enter from the spinal cord. Healthy nerves are left intact. This procedure is often used in children with mild cerebral palsy and has been shown to improve leg function and the ability to walk independently.
Intrathecal baclofen for spasticity:
- Another effective surgery is the implantation of a pump and a catheter to deliver liquid medication to the fluid around the spinal cord. This treatment option, called intrathecal baclofen therapy, uses a pump under the skin to deliver a steady, constant flow of baclofen, which is a medicine that can help relieve spasticity. Surgery to implant the pump and catheter requires only a short hospital stay followed up by doctor visits to monitor the dosage
PHYSIOTHERAPY TREATMENT FOR SPASTICITY :
- Physiotherapy treatment to reduce spasticity are mainly long stretching exercise, Positional stretching, weight bearing exercise, opposite group muscle strengthening exercise and use of Ice pack and cold pack: These exercise have following effects
- Minimising changes in the viscoelastic properties of the connective tissue;
- Altering the neural patterns of spasticity or spasms; and
- Maintaining levels of function for the individual.
- Standing:
- Tilt table/standing frame :
- The beneficial effects of standing, using either a tilt table or a standing frame are postulated to be secondary to the promotion of anti-gravity muscle activity in the trunk and lower limbs, maintenance or improvement in soft tissue and joint flexibility, modulation of the neural component of spasticity through prolonged stretch and altered sensory input, reduction of lower limb spasms, and positive psychological effect.
Stretching Exercise to reduce Spasticity :
- Relax Passive movement/long stretching of the muscles are highly useful in reducing sspasticity.
- The aim of stretch interventions is to maintain or increase joint mobility by influencing the extensibility of the soft tissues spanning the joints . Stretch interventions can be self-administered by patients or applied manually by therapists. All techniques involve the mechanical elongation of soft tissues for varying periods of time. Some techniques can only be applied for short periods of time. Other techniques, such as positioning, provide a way of administering stretches for sustained periods of time. Splints or serial casts are used to provide stretch for even longer periods of time and are sometimes used to provide uninterrupted stretch for many days or even weeks.
How ICE are Used for Reducing spasticity?

- Ice Pack : Local application of cold is used clinically to reduce the resistance of spastic muscle to rapid stretching and to decrease or abolish clonus . Cold can be applied to the body in three different ways: (1) immersing in cold water; (2) rubbing with ice cubes or ice packs; or (3) using evaporative sprays such as ethyl chloride. To avoid a complete conduction block of nerve fibres, 30°C has been suggested as a safe intramuscular temperature. The alteration caused by cold therapy in muscle may retrogradely influence the excitability in the spinal cord to decrease spasticity. This could be suggested as one of the mechanisms of relieving spasticity by cold therapy. Changes in the mechanical properties of muscles after the application of cryotherapy could also contribute to decreased spasticity.
How HOT PACK are used for reducing spasticity ?

- Hot Pack (i.e. bathing in hot water ) plays an important role in the rehabilitation of patients with spasticity . This modality has been used to change motor neuron excitability in spasticity for post-stroke patients. F-wave parameters (amplitude, F-wave/M-wave ratio) of motor-neuron excitability, have been used to illustrate changes in spastic muscles, after the application of thermotherapy (e.g. immersing muscles in water at 41°C for 10 minutes). A decrease in F-wave parameters after the application of thermotherapy has indicated the anti-spastic effects of thermotherapy.
Static Positioning :
- Muscle length positioning refers to the influence of a muscles’ length on stretch reflex activity. Because spasticity is known to be length-dependent, the position of patients during testing is likely to influence the results of the spasticity assessment, particularly when bi-articular muscles are involved . The influence of different positions on stretch reflex activity has been demonstrated with Root mean square (RMS) values of muscle activity higher in spastic muscles during supine positions compared to sitting positions . This is possibly because of changes in intrinsic muscle characteristics, and a muscle in an elongated state shows more stretch reflex activity compared with a muscle in a shortened state. This factor should be taken into account when assessing and treating spasticity with different interventions.
Reflex inhibitory thermoplastic splinting/orthotics :

- Wrist splints are thought to prevent or reduce contracture; the aim of splinting is to influence muscle extensibility, according to the degree of stretch provided by the splint . Both static and dynamic passive movements/stretching of joints affected by spasticity have been shown to have an effect on decreasing motor neuron excitability, increasing flexibility, and reducing tensile stress on the soft tissues . Thus a combination of reflexive and mechanical factors appear to result in decreased spasticity. It is unclear if passive movements/stretching in a weight bearing or non-weight bearing position are more beneficial towards reducing spasticity.
Mechanical gait trainer (treadmill training)
- The mechanised gait trainer are uses an overhead suspension system and harness to support a percentage of the patient’s body weight as the patient walks on a treadmill. The device stimulates the phases of gait, supports the patients according to their abilities, and controls the centre of mass in the vertical and horizontal directions. It has been reported to reduce spasticity by allowing early training of postural and stepping reactions. It facilitates motor relearning of gait cycles.



21 Comments