Hemiparesis
Table of Contents
What Is Hemiparesis?
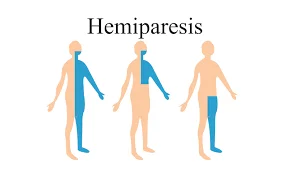
Hemiparesis is a common after-effect of Brain related conditions such as stroke that causes weakness on one side of the body. This one-sided weakness can restrict your movement and affect all day-to-day activities, such as walking, sitting, standing, dressing, eating, and Bathing.
People often confuse hemiparesis and hemiplegia. Both conditions occur as a result of a stroke or other related condition. In cases of hemiplegia, you will experience one-sided complete paralysis, which could make it difficult or impossible to move. Hemiplegia may lead to loss of bladder/bowel control, and trouble swallowing, breathing, and speaking while in Hemiparesis there is a mild form of one-sided paralysis.
What are the symptoms of Hemiparesis?
In hemiparesis mostly one side of the body affected which may be may be ipsilateral (the side of the brain injury) or contralateral (opposite the side of the brain injury).
The one-sided weakness may be on either the right or left side of your body if you suffer a stroke on the right side of your brain.
A common hemiparesis sign is a difficulty in standing, walking, or even keeping balance. On your weak side, you can also feel tingling or numbness.
A person with hemiparesis sometimes finds it difficult to grasp objects or move precisely. This may be accompanied by a loss of coordination and tired muscles.
Different physiological processes may be impacted depending on the type of hemiparesis that has been diagnosed. Some results are anticipated. (e.g., partial paralysis of a limb on the affected side). However, some deficits may initially appear to have nothing to do with limb weakness but are actually a direct outcome of the harm done to the affected side of the brain.
The arms, hands, face, chest, legs, or feet of a person with hemiparesis may also be affected by their one-sided weakness.
This can lead to one or more of the following symptoms in person:
- loss of balance
- difficulty walking
- difficulty grasping objects
- decreased movement precision
- muscle fatigue
- lack of coordination
Types of Hemiparesis
Some forms of hemiparesis include:
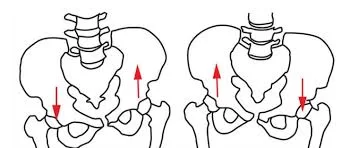
Ipsilatera or Contralateral Hemiparesis
Some persons develop weakness on the side of their body that corresponds to the side of their brain where the stroke occurred. Ipsilateral hemiparesis is the medical term for it.
2017 research According to Trusted Source’s analysis of 8,360 participants, the majority of persons with ipsilateral hemiparesis had a stroke in the past on the opposite side of the brain from their most recent stroke. In contrast to the brain damage brought on by the earlier stroke, this resulted in movement issues on the opposite side of the body.
Ataxic hemiparesis
When people struggle to coordinate their voluntary muscular movements, they are said to have ataxia. This issue only manifests on one side of the body in ataxic hemiparesis.
Numerous conditions can result in ataxia, which might manifest suddenly or gradually. Reliable Source. Ataxic hemiparesis, for example, is typically brought on by a stroke and progresses rapidly with potentially harmful effects.
Spastic hemiparesis
The term “spasticity” describes a condition when a person has unusually high degrees of muscle stiffness or tone. For instance, spasticity may be present in about 80%Trusted Source patients with cerebral palsy.
Spastic hemiparesis is the medical term for having abnormally tight muscles on one side of the body. normally the arm is further affected than the leg.
Hemiparesis vs. Hemiplegia
Hemiplegia differs from hemiparesis. A person may experience either condition after having a stroke.
Hemiplegia results in complete loss of muscle function, whereas hemiparesis produces muscle weakening. Paralysis is another word for the loss of muscle function.
What are the Causes of Hemiparesis?
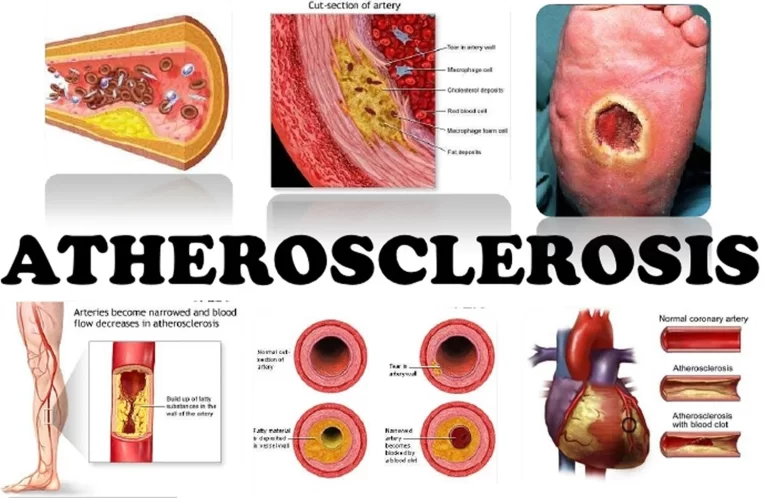
Most strokes occur when a part of the brain is deprived of new oxygen, which results in the death of brain cells. Hemiparesis can result from damage to the parts of the brain that control movement and strength.
The area of your brain that was impacted by the stroke determines which side of your body is weaker. For instance, you can experience muscle weakness on the left side of the body if your stroke affected the left side of the brain. This is referred to as being ipsilateral, or on the injured side. The weakening may, however, occasionally be contralateral, or on the side opposite the damage.
Your brain’s cells die when some regions receive insufficient oxygen during a stroke. Damage to these areas, especially if they are involved in bodily movement and strength, might result in hemiparesis.
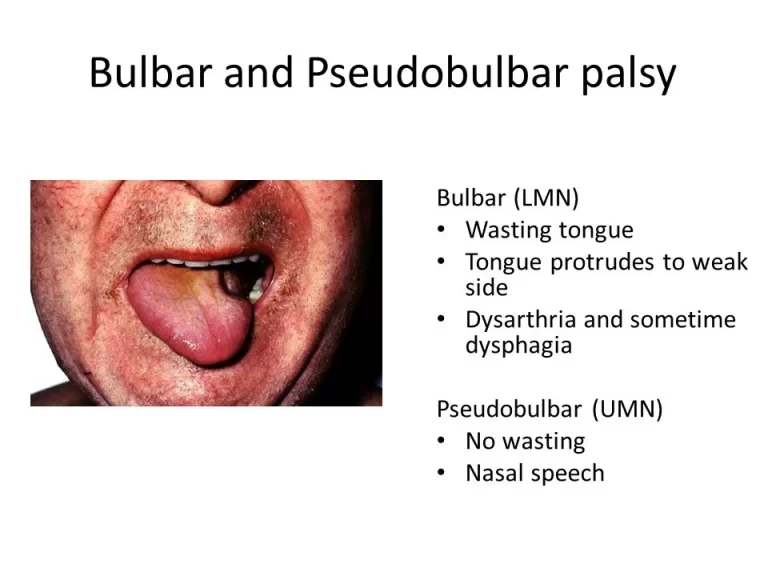
Stroke is the most frequent reason for hemiparesis and hemiplegia. Depending on the location and the severity of the lesion, strokes can result in a range of mobility problems. When a stroke affects the corticospinal tract, hemiplegia is frequently experienced. Hemiplegia can also result from diseases that affect the brain or spinal cord, such as Brown-Séquard syndrome and traumatic brain injury. Hemiplegic cerebral palsy can result from a permanent brain injury that happens during intrauterine life, at delivery, or early in life. Hemiplegic muscles exhibit characteristics of the upper motor neuron syndrome when a lesion that causes hemiplegia occurs in the brain or spinal cord. Other characteristics include impaired movement control, spasticity, increased deep tendon reflexes, clonus (a series of uncontrollable fast muscular spasms), and weakness.
Premature babies are much more likely than term babies to experience hemiplegia. Hemiplegia occurs frequently during pregnancy as well, and specialists speculate that this may be due to a difficult birth, the use of forceps, or another incident that results in a brain injury. There is a possible link between improvement after eliminating gluten from the diet and undiagnosed celiac disease.
Common Causes of Hemiparesis
- Vascular: cerebral hemorrhage, stroke, cerebral palsy
- Infective: brain abscess, spinal epidural abscess, cerebral palsy, encephalitis, meningitis
- Neoplastic: glioma, meningioma, brain tumors, spinal cord tumors
- Demyelination: neuromyelitis optical, disseminated sclerosis, ADEM, multiple sclerosis
- Traumatic: subdural hematoma, epidural hematoma, vertebral compression fracture, cerebral palsy, cerebral lacerations
- Iatrogenic: local anesthetic injections are given intra-arterially rapidly, instead of given in a nerve branch.
- Ictal: seizure, Todd’s paralysis
- Congenital: Neonatal-Onset Multisystem Inflammatory Disease (NOMID), Cerebral palsy
- Degenerative: ALS, corticobasal degeneration
- Parasomnia: sleep paralysis
Diagnosis
Your Doctor will examine you physically if you complain of any hemiparesis related symptoms. It can be challenging to discern whether your symptoms are brought on by pain, weakness, or another factor.
You will be tested on your reflexes, sensitivity, and strength throughout the physical examination. Your medical professional will grade your physical stamina on a scale of 1-5.4.
This rating can be used as a benchmark when the same healthcare provider or other healthcare professionals evaluate your strength at a later date.
Muscle Strength Rating Scale
The scale to measure muscle strength are:
- 0/5: No movement
- 1/5: Mild muscle movement (Flickr contraction)
- 2/5: Movements from side to side, however unable lift the arm or leg up against gravity
- 3/5: Can move up against gravity, but not against any force, such as mild pushing by the examiner
- 4/5: Can move against force, such as pushing by the examiner, but not with normally expected strength
- 5/5: Can move against resistance
- One side of the body may become completely weak; this condition is called hemiplegia.
A computer and several X-rays are used in a computerized tomography (CT) scan to produce a three-dimensional image.
Most often, hemiparesis is a stroke symptom. To diagnose a patient, doctors use computed tomography (CT) scans of the brain and the blood arteries that supply it. In order to do a CT angiography, a specific dye must be injected into the brain before a CT scan of the brain’s blood arteries and tissues can be taken.
When a stroke is suspected, a doctor may also perform an MRI scan to look for any blocked blood flow to the brain. Older studies from 2007 claim MRIs are more reliable than CTs at spotting stroke.
A person’s muscle strength in their hands and feet may be a valid approach to judge a person with long-term hemiparesis following a stroke, according to earlier research from the 2016 Trusted Source.
What is the Treatment for Hemiparesis?
Hemiparesis treatment may include medical and nonmedical:
stimulation with electricity. This technique involves applying tiny electrical pads to the hemiparesis-affected side’s weak muscles. The body receives an electrical charge that aids in the contraction of the muscles. Once you learn how to operate them, several of these devices can be utilized at home.
stimulation of the cortex. Similar to electrical stimulation, but with the electric current going to the thick membrane protecting the brain instead of the brain itself (called the dura). You must perform rehabilitation exercises while your brain is exposed to this current.
MCAT. A therapeutic approach called modified, constraint-induced therapy compels you to use your body’s weaker side. The nerve function may become more efficient in the area with continued practice. When combined with other treatments, mCIT is effective.
Falls are more common when one side of your body is weaker than the other. By modifying your lifestyle, you can reduce your risk of falling and getting hurt:
Increase your activity level and use the afflicted side as much as possible. Be cautious about speaking with your doctor before engaging in any activity that is out of the ordinary for you.
Put on wide-toed, flat-bottomed footwear. They’ll lessen the chance of falling and aid in maintaining balance.
Don’t navigate your home on the furniture. Use an approved assistance device your doctor has prescribed, such as a cane or walker.
When you’re walking, pay attention. Pay attention to your movements.
Additionally, be cautious when walking after taking any heart disease medications that could make you feel sleepy. If the effects are too powerful for you to tolerate, consult your doctor.
For the treatment of hemiparesis, a variety of rehabilitation techniques are available:
Modified constraint-induced therapy (CMT)
This is a successful method of improving upper limb function in stroke survivors. Daily activities might be significantly affected by upper limb impairment.
This type of therapy focuses on assisting in limiting the use of the upper limbs on the side of the body that is not affected while encouraging the use of the more affected limbs. It might be necessary to restrain the unaffected upper limbs with slings or mittens. It often entails focused, repeated training.
It is possible to apply other therapies, including mental imagery, to improve mCIT.
However, more study is required to determine the effects of the mind over the long run.
Mental imagery
Movement with mental visualization stimulates the parts of the brain. This could imply that if someone imagines moving the portion of their body that is weak, it may engage the muscles and parts of their brain that they would use if they were allready doing the activity.
People with hemiparesis may benefit from combining mental imagery with other therapy to reduce disability and increase the use of their upper extremities.
Electrical stimulation
Small electrical pads are applied to a person’s weaker muscles to provide electrical stimulation. This procedure shocks the muscle with electricity to induce contraction.
Depending on how intense the shock is, it may feel like a burning sensation or like a light tingle.
This treatment has the advantages of better motor control and mobility.
Cortical stimulation
A small electrode is applied by medical professionals to the dura, the membrane that covers the brain in a person undergoing cortical stimulation. The electrode transmits an electrical charge to the brain as the user performs rehabilitative exercises.
The Everest phase III trial, an older study from 2016, that examined the efficacy of cortex stimulation in aiding a person to acquire hand motor skills, was inconclusive.
The subjects who underwent cortex stimulation demonstrated functional improvements when compared to the control group 24 weeks following rehabilitation, the researchers discovered.
However, they cautioned against drawing conclusions from the findings too quickly because the benefits might have been at least partially the product of the cortex stimulation group receiving more attention from the researchers, a phenomenon known as the “Hawthorne effect” in science.
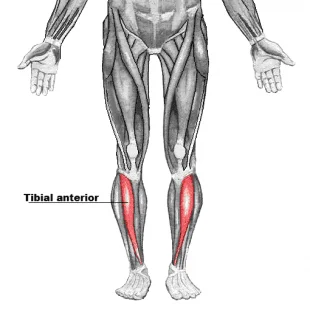
Assistive devices
Most often, physical therapists suggest appropriate equipment, such as an ankle-foot orthosis (AFO), canes, walkers, or a walking aid with four points of contact with the ground wheelchairs, to help a person with hemiparesis gain strength and movement.
Regular practice with an assistive device can promote mending damaged nerves and enhance movement control and flexibility. A plan that incorporates the right exercises should be created in collaboration with a healthcare practitioner.
Physiotherapy treatment of Hemiparesis
Your demands will be thoroughly evaluated by our expert neurological physiotherapists, who will then choose the best treatment plan and objectives for you. The type of treatment will depend on how weak the patient is. In extreme situations, the primary goal of treatment may be to improve the patient’s ability to sit correctly unassisted. In all cases, treatment will aim to maximize your potential and may include:
Exercise helps to strengthen your weak muscles to improve the functional use of your arm or leg
- Facilitation of normal patterns of movement
- Exercises to improve hand function and dexterity
- Exercises to improve your trunk control and core stability
- Exercises to maintain or improve the range of movement
- Gait training with walking aids to improve your independence and safety
- Exercises to improve your balance and coordination
- Home assessment to advise on appropriate equipment or aids which may be useful to improve your independence
- Liaison with your family or carers on the best ways to assist you with day-to-day activities
- Required to Occupational Therapists or Speech Therapists depending on the condition
- Hydrotherapy treatment to work on improving muscle flexibility
Is it possible to recover from Hemiparesis?
Hemiparesis can be cured, but you mostly fully restore your pre-stroke level of strength.
Start your therapy as soon as possible to improve properly. Make sure to follow your doctor’s recommended course of treatment and inform your healthcare team of any changes to your condition. Working towards more manageable, short-term objectives may also make you feel like your treatment is more effective.
Living with Hemiparesis
Making minor changes to your daily routine as you undergo treatment can make life easier for you:
- Become active to keep your muscles working.
- Make adjustments to your house to make managing daily duties simpler and safer. For instance, ramps, grab bars, and handrails can all be installed.
- By using an electric razor and adding non-slip mats to the shower, you can keep your bathroom safe.
- Wear Comfortable sports shoes (Avoid leather shoes).
- Use any prescribed assistive aids, such as a cane or walker.
To complete some tasks, you might need to acquire new techniques. Inform your doctor of any difficulties you are facing as well as the activities you want to resume in your life. You and your medical team can create a treatment plan to preserve or enhance your quality of life by establishing your priorities.
The ASA also offers a variety of lifestyle and home changes that a person with hemiparesis can implement to aid with the development of their motor abilities.
You might need to learn new skills in order to complete some assignments. Let your doctor know about any challenges you are having as well as the activities you want to start back up. By deciding on your priorities, you and your medical team can develop a treatment plan to maintain or improve your quality of life.
A person with hemiparesis can also use the ASA’s list of lifestyle and housing modifications to help them strengthen their motor skills.
the toilet seat is raised
Putting grab bars and ramps wherever they are useful in the house adding a bench with adhesive strips on the bottom of the tub buying an electric toothbrush and razor if necessary
The following lifestyle modifications can improve rehabilitation and prevent falls:
- Keeping your lifestyle activities to stay fit helps to maintain your muscle strength and enhance balance
- Putting on flat, wide-toed footwear to aid with balance
- Using one of the above-mentioned prescribed assistive devices instead of grasping onto furniture for support.
- Avoiding risky actions while taking drowsy-inducing medications
- Walking with awareness to prevent falling
Summary
A one-sided weakness is known as Hemiparesis. Loss of coordination, muscle weakness, and difficulties in balance are among the symptoms. Hemiparesis may be brought on by a stroke or another kind of brain-related condition.
Physiotherapy treatment, regular exercises with the use of assistive gadgets, and electrical stimulation are also forms of treatment. A person’s recovery might also be aided by a variety of home and lifestyle changes.



3 Comments