Atherosclerosis
Table of Contents
What is Atherosclerosis?
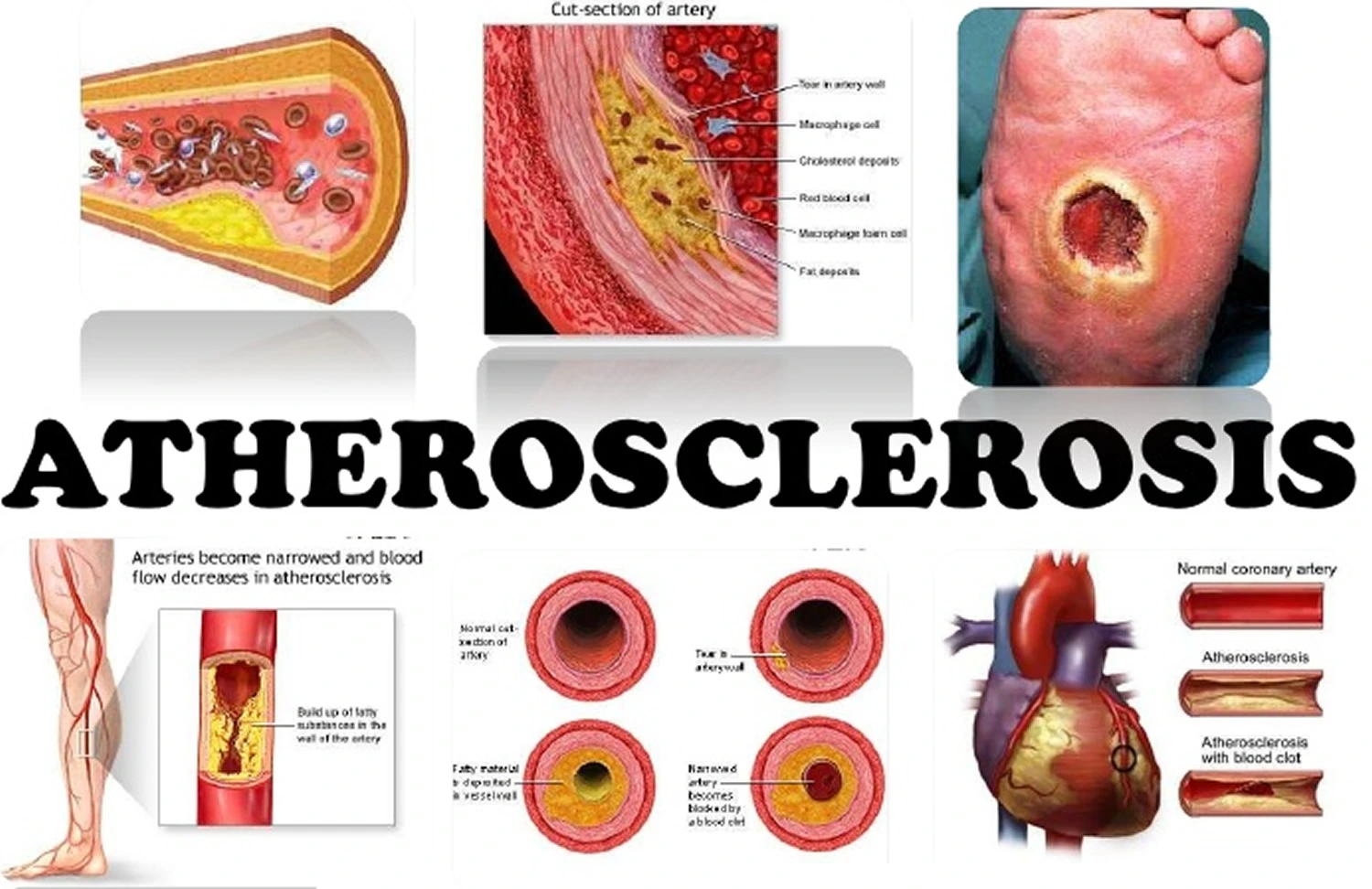
Atherosclerosis is a chronic disease characterized by the accumulation of plaque inside the arteries. It is the leading cause of cardiovascular diseases, including heart attacks, strokes, and peripheral arterial disease.
Arteries are blood vessels that bring oxygen-rich blood to organs & tissues throughout the body. Plaque is a sticky substance made of fat, cholesterol, calcium, & other substances. As plaque builds up, the artery wall grows thicker & harder.
This “hardening of the arteries” is generally a silent process in the early stages. May not notice any signs and symptoms for a long time. But eventually, as the plaque grows, the opening [lumen] of the artery narrows, leaving less room for blood to flow. This signifies less blood can reach the organs & tissues. The constant force of blood flow can cause plaque erosion or rupture, causing a blood clot to form.
A constricted artery is like a highway decreased to one lane. But a blood clot is like a barrier in the middle of the road. It stops blood flow to specific organs or tissue the artery typically provides. The effects on the body depend on where the blood clot forms. For instance, blockages in a coronary artery deprive the heart of oxygen-rich blood, leading to a heart attack. Can lower the risk for atherosclerosis, or slow its progression, by making lifestyle changes & managing underlying diseases. Research shows some treatments can decrease the size of plaque in your arteries [plaque regression)] or change its chemical makeup.
Causes of atherosclerosis
Injury to the artery’s inner lining endothelium leads to atherosclerosis to begin. The injury generally occurs slowly & over time.
Stages of atherosclerosis
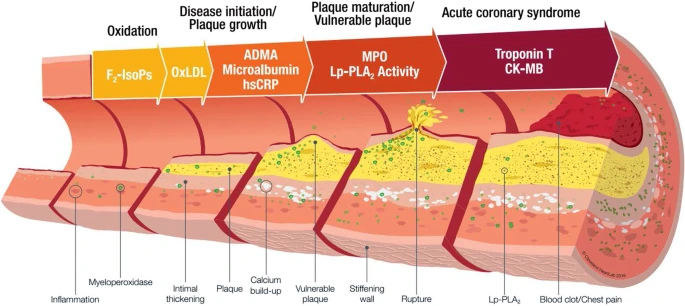
The stages of atherosclerosis occur over many years & contain:
Endothelial damage & immune response: Atherosclerosis starts with endothelial injury. The endothelium is a thin lining of cells that covers the inner layer of the artery wall intima. Many factors can lead to endothelial injury, involving high LDL cholesterol levels & toxins from tobacco products. The injury triggers chemical processes that lead white blood cells to travel to the damaged site. These cells gather & cause inflammation within the artery.
Fatty streak formation: A “fatty streak” is the 1st visible sign of atherosclerosis. It’s a yellow streak or patch started of dead foam cells at the site of endothelial injury. Foam cells are white blood cells that destroy invaders to try to get rid of them. In this circumstance, they consume cholesterol and thus appear foamy. Continued foam cell movement causes further damage to the endothelium. So, the fatty streak shifts into a larger piece of plaque. A fibrous cap that is made of smooth muscle cells forms over the plaque. This cap contains bits of plaque from breaking off into the bloodstream. As the plaque grows, it slowly narrows the artery’s opening lumen, so there’s less room for blood to flow through.
Plaque break or erosion: In this stage, blood clot disorders in the artery are due to plaque erosion. Plaque rupture occurs when the fibrous cap that protects the plaque breaks open. With plaque erosion, the fibrous cap stays unchanged, but endothelial cells around the plaque get tattered away. Both events cause the formation of a blood clot. The clot blocks blood flow & can cause a heart attack or stroke.
High cholesterol: Cholesterol is a waxy, yellow substance that’s found inherently in the body as well as in specific foods eaten. If the levels of cholesterol in the blood are too high, it can clog the arteries. It becomes a hard plaque that slows or blocks blood circulation to the heart & other organs.
Aging: As you age, the heart & blood vessels work harder to pump & receive blood. The arteries may stiffen & become less elastic, making them more susceptible to plaque buildup.
Diet: It’s important to eat a healthy diet. A healthy dietary pattern that stresses:
- A wide range of fruits & vegetables
- Whole grains
- Low-fat dairy products
- Poultry & fish, without skin
- Nuts & legumes
- Non-tropical vegetable oils, like olive or sunflower oil
Some other diet tips:
Avoid foods & drinks with added sugar, like sugar-sweetened beverages, candy, & desserts. The AHA suggests no more than 6 teaspoons or 100 calories of sugar per day for most women & no more than 9 teaspoons or 150 calories per day for most men.
Avoid foods high in salt. The main goal is to have no more than 2,300 milligrams of sodium per day. Ideally, consume no more than 1,500 milligrams a day.
Avoid foods high in unhealthy fats, like trans fats. Replace them with unsaturated fats. If you need to lower your blood cholesterol, lower saturated fat to no more than 5 to 6 percent of total calories. For someone eating 2,000 calories a day, that’s about 13 grams of watery fat.
Symptoms of Atherosclerosis
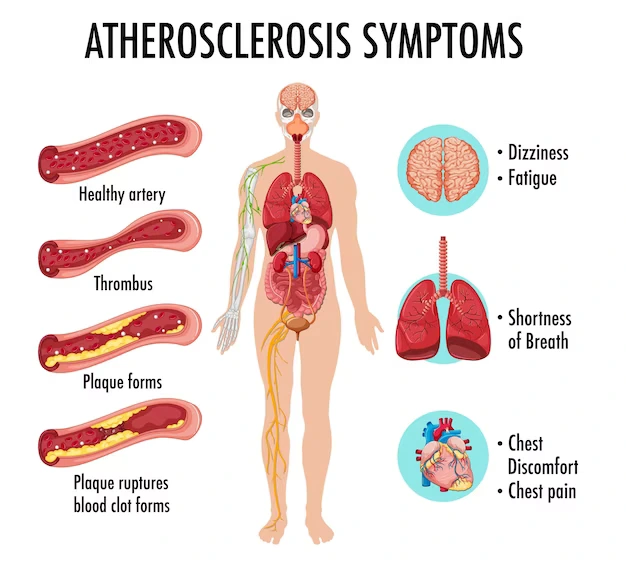
Atherosclerosis usually doesn’t generate symptoms until an artery is very narrow or blocked. Many people don’t know they have plaque buildup until a medical crisis, like a heart attack or stroke, happens. May notice symptoms if the artery is more than 70% blocked. Some comprehensive plaque buildup can cause complications, which in turn generate symptoms. The chart below lists some symptoms may feel depending on the complication.
A complication of atherosclerosis possible symptoms
Coronary artery disease:
- Stable angina,
- Shortness of breath is called dyspnea during light physical movement, sometimes, the first symptom is a heart attack.
Heart attack:
- Chest pain or discomfort [angina]
- Pain in the back, shoulders, neck, arms, or belly
- Shortness of breath or trouble breathing
- Feeling dizzy or lightheaded.
- Heart palpitations
- Fatigue
Mesenteric ischemia:
- Pain or cramping in your belly (stomach) after eating
- Bloating, nausea, & vomiting
- Diarrhea
- Unintentional weight loss due to “food fear” which means fear of pain after eating.
Peripheral artery disease (PAD):
- Intermittent claudication: This is leg pain or cramping feeling when you’re active. It goes away when the rest. It’s the first symptom of Peripheral artery disease
- Burning or aching pain in the feet & toes when resting, specifically when lying flat.
- Changes in skin color like redness.
- Cool skin on the feet.
- Frequent skin & soft tissue infections, often in the legs or feet.
- Sores on the feet or toes that don’t heal.
Renal artery stenosis:
- Elevated blood pressure that’s invulnerable to multiple medications.
- Changes in how one usually pees.
- Swelling (edema).
- Feeling drowsy or tired.
- Skin that feels dry, itchy, or numb.
- Headaches.
- Unexplained weight loss.
- Nausea, vomiting, or loss of appetite.
Stroke or transient ischemic attack (TIA):
- Dizziness
- Drooping on one side of the face.
- Loss of feeling, loss of muscle strength, or weakness on one side of the body.
- Severe headache.
- Slurred speech or problem in forming words.
- Vision loss in one eye. May notice a dark shade coming down over the field of sight.
Carotid artery disease:
- Generally, the first symptoms are a TIA or stroke.
- Most common symptoms of atherosclerosis don’t show up until a blockage happens.
Common symptoms include:
- Chest pain or angina
- Pain in the leg, arm, & anywhere else that has a blocked artery
- Cramping in the buttocks while walking
- Shortness of breath
- Fatigue
- Confusion, which happens if the blockage involves circulation to the brain
- Loss of motor or sensory function on one side of the body, which occurs if the blockage involves circulation to the brain muscle deficiency in the legs from lack of circulation.
It’s also necessary to know the symptoms of heart attack & stroke. Both of these can be led by atherosclerosis & need immediate medical attention.
The symptoms of a heart attack contain:
- chest pain or discomfort
- discomfort in the shoulders, back, neck, arms, & jaw
- abdominal pain
- shortness of breath
- sweating
- lightheadedness
- nausea and vomiting
- a sense of impending doom
The symptoms of stroke contain:
- weakness in the face or limb
- trouble speaking
- trouble understanding speech
- vision issues
- loss of balance
- sudden, intense headache
Diagnosis of atherosclerosis
To analyze atherosclerosis or calculate the risk of inventing it, a healthcare provider will:
- Perform a thorough physical exam: Use a stethoscope to listen to the heart & blood flow via the arteries. For instance, the provider will check the carotid streets in the neck for a whooshing sound called a “bruit.” This sound may suggest the presence of plaque.
- Medical history & family history: These points can help show the threat of atherosclerosis & its difficulties.
- Ask about your lifestyle: The provider may ask about lifestyle factors like past or present use of tobacco consequences.
- Order blood tests: Cardiac blood tests show cholesterol levels & many details about heart function.
What examinations will be done to diagnose this condition?
The healthcare provider may request additional tests to diagnose atherosclerosis & plan treatment. These tests contain:
- Angiography: This test utilizes special X-rays to discover & measure blockages. The healthcare provider will infiltrate a contrast dye into the arteries to help the blockages show up on the X-rays.
- Ankle or brachial index: This test compares the blood pressure in the ankle to the pressure in the arm to measure blood flow in the arms & legs.
- Chest X-ray: A chest X-ray takes images inside of the chest.
- CT scan: This scan takes images inside of the body & can show any hardening & narrowing of the large arteries.
- Echocardiogram (echo): An echo takes pictures of the heart’s valves & chambers and measures how well the heart is pumping.
- Electrocardiogram (EKG): An EKG measures the heart’s electrical activity, rate, & rhythm.
- Exercise stress test: This test measures the heart function while you’re physically involved.
- Carotid ultrasound: This test assumes ultrasound images of the arteries in the neck [carotid arteries]. It can notice the hardening or narrowing of these arteries as blood streams to the brain.
- Abdominal ultrasound: This ultrasound takes images of the abdominal aorta. It checks for ballooning [abdominal aortic aneurysm] or plaque buildup in the aorta.
What experts might require to see for Atherosclerosis?
If have atherosclerosis, the healthcare provider may suggest seeing a professional, such as a:
- Cardiologist: who specializes in the heart.
- Nephrologist: who specializes in the kidneys.
- Neurologist: who specializes in the nervous system (brain & spine).
- Vascular surgeon: who specializes in blood vessels.
Treatment for Atherosclerosis
Atherosclerosis treatment contains one or more of the following:
- Medications
- Procedures or surgeries
- Lifestyle changes
The healthcare provider will develop a plan based on the requirements. Common treatment plans include:
- Lowering the risk of blood clots.
- Controlling complications like a heart attack or stroke.
- Easing signs and symptoms.
- Helping them develop patterns of eating that support the heart and blood vessels.
- Slowing and preventing plaque buildup in the arteries.
- Improving blood flow by widening the arteries or bypassing blockages or avoiding the blockages.
Medications
Medications can help control atherosclerosis from worsening.
Medications for treating atherosclerosis contain:
- Cholesterol-lowering drugs, including statins
- Beta-blockers, which “rest” the heart
- Antiplatelet drugs such as aspirin prevent blood from clotting & clogging your arteries
Aspirin can be extremely useful for people with a history of atherosclerotic cardiovascular disorder, involving heart attack & stroke. An aspirin regimen consulted with the doctor may potentially lower the risk of having another health event if they already have atherosclerosis.
The U.S. Preventive Services Task Force recently dismissed updated guidelines on using aspirin for the prevention of cardiovascular conditions. These guidelines may be appropriate in discussions with the doctor. If have no history of atherosclerotic cardiovascular condition, only use aspirin as a preventive medication if the risk of bleeding is low & the risk of atherosclerotic cardiovascular disorder is high. Always consult an aspirin regimen with the doctor first.
Surgery
If symptoms are particularly severe or if muscle or skin tissue are endangered, surgery may be required.
Possible surgeries for treating atherosclerosis contain:
Bypass surgery: this involves using a vessel from somewhere else in the body or a synthetic tube to divert blood around the blocked or restricted artery.
Thrombolytic therapy: which affects dissolving a blood clot by injecting a drug into the affected artery.
Angioplasty & percutaneous coronary intervention: which concerns using a catheter & a balloon to expand the artery, sometimes inserting a stent to maintain the artery open.
Atherectomy: which affects removing plaque from the arteries by using a catheter with a sharp blade at one end
Endarterectomy: which affects surgically removing fatty deposits from the artery.
Lifestyle Changes for Atherosclerosis
Lifestyle changes lower the chance of complications. The provider will create a plan specific to the requirements. General tips contain:
- Avoid all tobacco products (involving smoking & vaping).
- Build exercise into the daily routine.
- Specific lifestyle changes can slow or even reverse the progression of atherosclerosis & are generally the first-line treatment for people analyzed with the condition.
The doctor may recommend one or more of the following steps:
There are 7 Self-care Steps to Take after a heart attack
Follow a heart-healthy diet: This can help control risk factors for atherosclerosis & heart disease such as weight, blood pressure, & blood cholesterol, and glucose levels by focusing on eating certain foods while avoiding others.
A heart-healthy diet is widely comprehended to be high in fruits, vegetables, & whole grains, & low in advanced carbohydrates, saturated & trans fats, & sodium.
Practical tips contain switching from white to whole-grain bread, eating fruits & vegetables instead of chips or crackers as snacks, using olive oil instead of solid fats like butter, & decreasing sugar and sugar substitutes as much as possible.
Heart-Healthy Diet Makeovers
Stop smoking: Smoking or using tobacco in another form hurts the arteries. If you’re a smoker, quitting is the single most useful way to stop your atherosclerosis from getting worse & decrease the risk of complications.
Get enough exercise: Exercising can help circulation & let the body use oxygen more efficiently, which can help limit the injury induced by reduced blood flow from atherosclerosis. Should try to get 2 hours & 30 minutes of moderate aerobic exercise each week, or 1 hour & 15 minutes of vigorous aerobic exercise. Aerobic exercise is any physical exercise that raises the heart & breathing rates. While exercising in breaks of at least 30 minutes is ideal, Can break up the movement into segments as short as 10 minutes & still get substantial help.
Aim for a healthy weight: If overweight, losing just 5-10 pounds can lower the risk for high blood pressure & unhealthy cholesterol levels both factors that can donate to atherosclerosis. In grown-ups, healthy body weight is generally described as a body mass index (BMI) a measurement based on height &weight between 18.5 & 24.9. Should also keep checks on the waist circumference, which may be considered unhealthy if it’s above 35 inches [88.9 cm] in women or 40 inches [101.6 cm] in men.
Try to manage stress: Techniques like directed relaxation, deep breathing, meditation, & yoga can help the healthily cope with stress. You may also find comfort from stress through exercise, talking with friends & family, or visiting a mental health professional.
Alternative Therapies for Atherosclerosis
There’s some evidence that certain foods & dietary supplements may help decrease high LDL cholesterol & blood pressure 2 risk factors for atherosclerosis.
Talk to the doctor before starting any dietary complements. Some treatments may be useless or even harmful to the health, as they can interact with prescription medication & cause dangerous side results.
Possibly healthy foods and dietary supplements contain:
- Alpha-linolenic acid (ALA)
- Barley
- Beta-sitosterol
- Calcium
- Cocoa
- Cod liver oil
- Coenzyme Q10
- Fish oil
- Folic acid
- Garlic
- Oat bran
- Omega-3 fatty acids
- Psyllium
- Sitostanol
- Tea (black or green)
- Vitamin C
Some of these products are widely available as stand-alone supplements, while others are components in foods or supplement instructions.
Prevention
May not be able to control atherosclerosis. But can decrease the risk and lessen the effects of the disease.
Here are some steps can take:
- Eat foods low in watery fat, trans fat, cholesterol, sodium, and sugar.
- Exercise regularly starts with short walks and builds up to 30 minutes a day most days of the week.
- Manage any health disorders, especially diabetes, high blood pressure, and high cholesterol.
- Don’t use tobacco products.
- Yearly checkups with a Doctor
Prognosis
What is the outlook for people with atherosclerosis?
Early diagnosis & treatment can help people with atherosclerosis live healthy, energetic lives. But the condition can cause medical emergencies & even be fatal. That’s why knowing the risks & working with the healthcare provider to lower them is important.
Risk factors for atherosclerosis
There are several risk factors for atherosclerosis. May be able to decrease modifiable risk factors, involving some medical conditions & lifestyle factors, in some cases.
It’s essential to note that some risk factors vary based on the sex assigned at birth. For instance, people designated male face a higher risk of atherosclerosis at a more youthful age than people designated woman at birth.
Non-modifiable risk factor: Increasing age people designated man at birth face a higher risk after age 45. People assigned females at birth face a higher risk after age 55. Family history of premature cardiovascular condition. This means a close biological family member whose AMAB was analyzed with cardiovascular disease before age 45. One whose AFAB was analyzed before age 55.
Medical conditions:
- Diabetes.
- High blood pressure (hypertension).
- hyperlipidemia [High cholesterol], especially high LDL cholesterol or high levels of a specific lipoprotein named lipoprotein
- Metabolic syndrome.
Lifestyle factors:
- Smoking or tobacco use.
- Lack of physical activity.
- A diet is high in saturated fat, trans fat, sodium, & sugar.
Family history: If atherosclerosis runs in the family, may be at risk for hardening of the arteries. Can inherit this circumstance, as well as other heart-related difficulties.
Lack of exercise: Regular exercise is good for the heart. It keeps the heart muscle strong & encourages oxygen & blood flow throughout the body. Lack of exercise increases the risk for a host of medical conditions, involving heart disease.
High blood pressure: High blood pressure can damage the blood vessels by making them weak in some areas. Cholesterol & other substances in the blood may lower the flexibility of the arteries over time.
Smoking: Smoking tobacco products can damage the blood vessels & heart.
Diabetes: People with diabetes have a much higher incidence of coronary artery disorder.
Complications of atherosclerosis
Atherosclerosis interferes with the normal workings of the cardiovascular procedure. It can restrict or block blood flow to various regions of the body, including the heart & brain. Possible complications of decreased blood flow contain:
- Carotid artery disorder
- Coronary artery disorder
- Heart attack
- Mesenteric ischemia
- Peripheral artery disorder
- Renal artery stenosis
- Stroke
Transient ischemic attack (TIA)
Atherosclerosis can also weaken the artery walls, showing the formation of aneurysms.
Early diagnosis & therapy of atherosclerosis can help them avoid complications.
The coronary arteries are blood vessels that provide the heart’s muscle tissue with oxygen & blood. CAD( Coronary artery disease) arises when the coronary arteries become hard.
Carotid artery disease
The carotid arteries are discovered in the neck and supply blood to the brain.
These arteries are compromised if plaque constructs up in their walls. The absence of circulation may decrease how much blood & oxygen reach the brain’s tissue & cells.
Peripheral artery disease
The upper and lower body depend on the arteries to provide blood & oxygen to their tissues. Hardened arteries can lead to circulation difficulties in these areas of the body.
Kidney disease
The renal arteries supply blood to the kidneys. Kidneys purify waste products & extra water from the blood.
Atherosclerosis of these arteries may cause kidney failure.
How do take care of yourself?
It’s important to work closely with the healthcare provider. They’ll keep a close eye on the condition & tell you how frequently u should come in for appointments. Go to all of your appointments & follow-ups, & be an active partner in the care. Tell your provider right away about any unique or changing symptoms.
Also, take care of mental health. May also feel overwhelmed by the requirement to make lifestyle changes. But those feelings shouldn’t prevent them from enjoying life. Some tips for managing thoughts & worries include:
Share feelings with a counselor or support group.
Join with others who have cardiovascular disease. Talk to your family & friends about the lifestyle changes you’re making. Describe why these changes are necessary to you & ask them to help you stay on track.
Summary:
Atherosclerosis is a typical condition. Many other people are in your shoes. The healthcare provider is willing to help you manage your condition so you can live a long & healthy life.
FAQ
Atherosclerosis is the thickening or hardening of the arteries induced by a buildup of plaque in the inner lining of an artery. Risk elements may contain high cholesterol & triglyceride levels, high blood pressure, smoking, diabetes, obesity, physical activity, & eating saturated fats.
Optimal Vitamin K2 intake is important to avoid the calcium plaque buildup of atherosclerosis, thus keeping the risk & rate of calcification as low as possible. Matrix GLA protein (MGP) found in the tissues of the heart, kidneys, and lungs plays an important function in vascular calcium metabolism.
Strawberries, blueberries, blackberries, & raspberries are jam-packed with important nutrients that play a major role in heart health. Berries are also rich in antioxidants like anthocyanins, which guard against oxidative stress & inflammation that donate to the development of heart conditions.


3 Comments