Vertebroplasty
Table of Contents
What is the Vertebroplasty procedure?
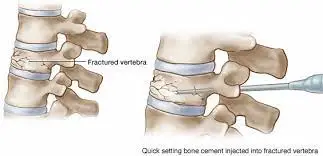
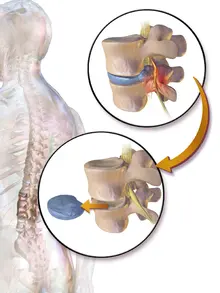
Vertebroplasty is a medical procedure used to treat vertebral compression fractures, which are fractures that occur in the spinal vertebrae. Vertebroplasty is a surgical treatment that injects cement into a cracked or broken spinal bone to assist relieve pain.
Spinal bones are called vertebrae. Vertebroplasty is used most frequently to treat a type of injury called a compression fracture. These injuries are generally caused by osteoporosis, a condition that weakens bone. Osteoporosis is most common in aged people.
numerous compression fractures do not bring on any symptoms and do not need any treatment. But if you have patient or severe pain, vertebroplasty might help.
with the aim of relieving your spinal pain and restoring your mobility. Not all people with fractured vertebrae are applicants for the procedure, nevertheless. Some research also suggests that vertebroplasty provides small benefits over a more conservative approach, which can include
- Bed rest
- Pain relievers
- Muscle relaxants
- Back braces
- Physical remedy
Percutaneous vertebroplasty has grown extensively accepted as a safe & effective minimally invasive technique for the treatment of painful vertebral body compression fractures refractory to medical remedy. The aim of a vertebroplasty procedure is to stabilize the vertebral compression fracture to cease its painful movements.
Why the Vertebroplasty procedure is done?
The most common suggestion for vertebroplasty is the treatment of painful acute and subacute VF in cases who have failed to respond to a 4- to 6-week course of applicable medical remedy. Failure to respond to medical remedy is defined as minimum or no pain relief with specified painkillers, or shy pain relief in cases who are unfit to tolerate opiates secondary to unwanted side goods similar as sedation, confusion, and constipation.
By far, the most common bearing etiology of painful VF is osteoporosis. Other often encountered causes are metastatic conditions, multiple myeloma, and painful aggressive hemangiomas. Uncommon suggestions for management include pain related to osteonecrosis( Kummel disorder), Langerhans cell histiocytosis, osteogenesis imperfecta, spinal pseudarthrosis, Paget condition, & intravertebral vacuum phenomena. vertebroplasty has also been executed in the treatment of painful Schmorl lumps and for the reinforcement of pathologically frail vertebral bodies previous to surgical stabilization.
Vertebroplasty can relieve pain caused by compression fractures in the vertebral column. Compression fractures most frequently occur when osteoporosis or cancer weakens the spinal bones.
Weakened spinal bones can fracture or break into many particles. The fractures can happen during exercise that wouldn’t generally break a bone. Examples include
- Twisting
- Bending
- Coughing or sneezing
- Lifting
- Rolling over in bed
What are the risk factors of Vertebroplasty procedures?
In vertebroplasty, a form of bone cement is injected into a damaged spinal bone. Similar procedures include kyphoplasty, which involves initially inserting a balloon into the spinal column. To increase the amount of room inside the bone, the balloon is inflated. The balloon is then inflated and taken out before the cement injection.
The following are risks connected to each procedure:
- Leaking cement. The spinal bone may allow some of the cement to leak out. If the cement presses on the spinal cord or nerves, this may result in new symptoms. Small fragments of this cement leak may also enter the bloodstream and travel to the kidneys, heart, lungs, or brain. Rarely, this can harm these organs and occasionally even result in death.
- further fractures. These operations could make it more likely that nearby spinal bones will fracture.
- Hemorrhaging
- losing blood
- Fever
- irritated nerve roots
- Infection
- delayed action. In comparison to nonsurgical treatment options, vertebroplasty is less likely to offer significant pain relief if it is not performed within 8 weeks of the initial fracture. One explanation could be that the fracture has most likely already begun to heal after a few months.
- medication allergic responses.
- heart or breathing issues if under general anesthesia
Before having vertebroplasty or kyphoplasty, you might need to wait several hours before eating or drinking. You might be able to take any daily prescriptions the morning before the surgery with a few sips of water. For a few days prior to the surgery, you might need to refrain from using blood thinners. Observe the advice given to you by the doctor.
Leave your jewelry at home and dress comfortably. The majority of folks return home that day. You should make plans in advance for a ride home.
What happens before the Vertebroplasty procedure?
The doctor will probably take an X-ray, take a complete medical history & do a physical test to determine the precise position and nature of your backbone-related pain. the doctor might also utilize Magnetic Resonance Imaging( MRI) or a Computed Tomography Scan( CT or CAT scan).
Tell your doctor about all prescription and over-the-counter drugs and any herbal supplements you’re taking.
Tell your doctor if you have a history of bleeding diseases or if you’re taking any anticoagulant(blood-thinning) medicines, aspirin, or other medicines that affect blood clotting.
It’s common for no food or drinks to be allowed lower than 6 hours before the vertebroplasty procedure. For instance, if the surgery is listed in the morning, the doctor might need that no food or drinks to be consumed after midnight before the procedure. However, If you smoke, try to stop, If you have been drinking a lot of alcohol. A small quantity of water is generally allowed up to 2 hours before the surgery.
In addition, some restrictions on medicines might be put in place in the days leading up to the surgery. Some medicines might need to be discontinued, and others might need tablets to be adapted. These restrictions can vary extensively, depending on the patient’s particular health status.
What happens during the Vertebroplasty procedure?
A hospital gown will be on you. Most likely, a vein in your arm or hand will receive the insertion of a flexible, slender tube.
Your level of anesthesia is determined by the nature of the procedure and the quantity of affected spinal bones. During the procedure, general anesthesia keeps you in a sleep-like state. Most people, though, only require sedation. Sedatives induce relaxation and sleep.
You will receive numbing shots in your skin as you lay face down. A vertebroplasty typically lasts one hour. If more than one spinal bone requires treatment, the process could take longer.
During the surgery, specialized X-rays or CT scans are performed to help guide the needle into the spinal bone. It takes 20 minutes for the cement to harden.
Technique:
vertebroplasty is smartly performed using high-quality fluoroscopy for needle placement, and cement injection should be accomplished under nonstop fluoroscopy. Although not as ideal, a movable c- arm unit can be used. Biplane fluoroscopy, if available, can drop procedure time. In some technically grueling cases, CT guidance combined with CT fluoroscopy or conventional fluoroscopy may be required.
The procedure is performed using a maximum surgical barrier approach. Preprocedural precautionary antibiotics should be used in all immunocompromised cases. Although there’s no clear agreement on routine antibiotic use in non-immunocompromised patients, numerous interpreters administer precautionary intravenous antibiotics to all cases instantly before the beginning of the procedure. The authors generally administer 1 g of cefazolin 1 hour before the beginning of the procedure; in patients with an allergy to penicillin or cefazolin, 500 mg of vancomycin can be substituted.
Thoracic and lumbar vertebroplasty is performed with the patient in the prone position. Padding should be applied to maximize patient comfort and reduce the curve of the spine. The skin, subcutaneous tissues, and periosteum are locally anesthetized with lidocaine, which may need the use of a spinal needle for length. The patient’s heart rate, blood pressure, & oxygen saturation are continuously monitored throughout the time period of the procedure. In numerous practices, including the authors’, vertebroplasty is performed under conscious sedation using intravenous acquainted and fentanyl. Infrequently, deeper sedation with an anesthesiologist may be needed for patients with a severe pulmonary concession or those unfit to tolerate prone positioning without general anesthesia.
Proper positioning of the fluoroscopic C arm is important to the success of the process. The C arm should be disposed of cranially or caudally to view the vertebral body “ straight on, ” that is, the anterior wall projected directly over the posterior wall. To pierce the vertebral body using the transpedicular approach, the VP needle is advanced “ down the barrel ” of the pedicle under intermittent fluoroscopic guidance. Prior to needle placement, the C arm is deposited in a 20- to 30-degree ipsilateral oblique view. The pedicle, especially the medium and the inferior walls, must be plainly imaged. Single-shot radiographs may be needed for advanced image resolution. In the author’s experience, needle advancement is stylishly performed with a diamond-shaped multi-beveled stylet while using a mallet to gently tap and drive the needle into place. the original use of a single-beveled stylet may be more tricky and lead to problems with the needle having a tendency to slide or skid off the pedicle. Taking the redundant time to appropriately seat the needle on the pedicle is prudent, as the needle will tend to continuously elect the original “ hole, ” making repositioning delicate if the original needle placement is sour. While advancing the needle, it’s imperative that the needle doesn’t violate the medium and inferior walls of the pedicle to drop the pitfalls of a nerve root or spinal cord injury. As similar, the needle should be advanced toward the upper and external half of the face of the pedicle.
Intermittent side views should also be acquired to assure applicable cranial to caudal angulation, access into the fractured vertebral body, and to determine when the needle reaches the posterior( rearward) wall of the vertebral body. Until the needle enters the posterior vertebral body, AP( ipsilateral oblique) protuberance should be used to advance the needle. With experience, the posterior wall can frequently be detected with slightly increased resistance in the needle, as well as a subtle change in the “ tapping sound ” encountered while advancing the needle with a mallet. Once the needle has been advanced just beyond the posterior wall of the vertebral body, a biopsy can be carried out as necessary through the external cannula with a bone biopsy needle. Once the posterior vertebral body has been reached, the single-beveled stylet may help by steering the tip of the VP needle to the intended position, or toward the midline. generally, the needle will advance toward the appropriate pointed edge of the bevel.
Multiple types of bone cement are commercially available and differ in terms of cost, radio-opacity, rate of polymerization, and biocompatibility. The advantages and disadvantages of colorful different types of cement have been beforehand described. Although newer compounds and calcium phosphate cement exist, PMMA remains the most extensively used in the treatment of osteoporotic and malignance-related vertebral body fractures.
Intraosseous venography previous to the injection of PMMA has been used by some interpreters as a way of assuring no direct communication with central or epidural venous structures, and potentially forecasting the direction of cement flow within the vertebral body. still, a discrepancy from intraosseous venography can eventually obscure the capability to confidently fantasize about cement at the time of its injection. besides recently, authors have shown no significant difference in clinical consequences or significant added benefit with intraosseous venography, and the practice has afterward dropped in prevalence. The authors don’t routinely perform intraosseous venography.
Cement injection should be performed in the side protuberance using nonstop fluoroscopy. The aim is the delivery of cement equally in the vertebral body or to the targeted area while avoiding extra-vertebral cement delivery, for sample, the epidural vein or beyond the posterior wall of the vertebral body. Cement should be taken to deliver with care at a controllable pace to avoid over-pressurization of the cement delivery system. Cement may “ shoot out ” when the pressure makes- up ultimately overcomes the inhibition and lead to cement spreading to unintended places. Turning the external cannula intermittently will release any pressure that may build. As cement is injected, the needle is slowly pulled back to ease the even distribution of cement throughout the vertebral body.
To further minimize the danger of cement leakage, PMMA should immaculately be injected when it reaches the thickness of a paste. Injection of cement is stopped once cement reaches the posterior one-quarter of the vertebral body. However, the injection should be temporarily stopped to “ cast ” the vein, averting further cement accumulation in the vein and avoiding pulmonary embolism, If cement is noted to travel into a vein. generally, once the cement has thickened within the vein, the injection can be continued. also, if leakage outside of the vertebral body is noticed, the injection should be temporarily stopped. dragging the needle back or twisting it to redirect the cement might be useful in stopping leakage when it is encountered.
As mentioned over, the aim is cement delivery across the midline( if unilateral) and even distribution in the superior-inferior and anterior-posterior vertebral body. Bilateral access may be necessary when compression is severe or if cement doesn’t spread to the midline when using a unilateral approach. With experience, a contralateral needle can be rapidly placed if a unilateral approach is shy. When doing so, it’s suggested that the first needle be left in place within the pedicle to avert leakage of cement backward along the original needle tract. Studies have failed to display any difference in clinical results when using a unilateral versus bilateral approach. When removing the needle, caution must be taken to prevent leaving a “cement tail”. This can be avoided by clearing the needle of cement utilizing a stylet, or by gently spinning and rocking the needle once retracted to the edge of the pedicular boundary.
Infrequently, in cases of severe compression fractures or at advanced levels of the thoracic spine where pedicles are frequently more vertical in configuration to the vertebral body, a para-vertebral or extra-pedicular approach may be required. The authors prefer a transpedicular approach & use a para-vertebral or extra-pedicular technique only if the transpedicular approach is not technically possible. Although beyond the range of this article, treatment of cervical VFs may need an indispensable anterolateral, transoral, or trans-facial approach and more advanced image guidance. Care must be taken to prevent the carotid jugular complex. Treatment of these fractures should be allocated to the most educated practitioners.
What happens after the Vertebroplasty procedure?
You are allowed to lie on your back for 1 to 2 hours until the cement hardens. You’ll probably remain in an observation room for another 1 to 2 hours. Following vertebroplasty, bedrest or resting at home is typically advised for the first 24 hours. The majority of routine prescriptions can be resumed, and activity levels can be gradually increased.
You may witness pain relief somewhere instantly after the procedure, but it might take up to 72 hours. Your doctor can give you untoward pain relievers for temporary discomfort.
The doctor will assess your pain & check for any possible complications.
utmost patients who have vertebroplasty go home on the same day. You will need to arrange in advance for someone other to drive you.
The place on your back where the needles were fitted might be sore for many days. An ice pack can assist relieve this pain. cover your skin from the ice with a cloth. give ice pack for about 15 minutes.
You may need to continue wearing a back brace, but it’s generally gratuitous. A follow-up appointment with the doctor is generally listed a couple of weeks after surgery to assure that the recovery is going well. You should avoid heavy weight lifting and strenuous conditioning for at least six weeks.
What are the complications of Vertebroplasty procedures?
All surgeries that are done inside the body and involve medicine include some serious risks, including infection, allergic reaction, & excessive bleeding. Other potential complications of vertebroplasty include:
Cement leakage. This problem can occur when the bone cement leaks outside of the intended vertebral compression fracture’s cracks. Fortunately, there are unfrequent complications associated with bone cement leaking outside of the fracture, especially if it is a little amount. Nevertheless, it is possible for bone cement to come out onto a nerve root or the spinal cord, which could increase pain, tingling, numbness, & weakness, as well as possibly cause problems with function & mobility. Additionally, instances of bone cement entering a vertebral vein and producing issues, such as pulmonary embolisms (lung artery obstructions), have been documented.
Paralysis. The spinal cord and other vital nerves are close by when vertebroplasty is performed, therefore a mistake in the needle’s placement could potentially cause injury that results in weakening and/or paralysis of one or more limbs.
Pain is not lessened. Vertebroplasty occasionally fails to alleviate symptoms, even when there were no mistakes made or difficulties encountered.
This is not a whole list of possible vertebroplasty complications. A patient who suffers an osteoporotic fracture is already at risk for further fractures, but it is not yet known whether vertebroplasty or kyphoplasty increases the risk of another fracture in the spine or ribs.
Physiotherapy treatment
Physical therapy is indicated both pre and post-op. Prior to vertebroplasty, the focus is on pain management and avoiding secondary problems such as advancing weakening and immobility. The following interventions are recommended for pain relief previous to the procedure
- Analgesic medicine
- Heat
- Massage
- Gentle exercises and advice on the conditioning of day-to-day living
- Rest
Physiotherapists should also give advice to avert further injury, especially when recommending exercises. Patients should be advised to avoid flexion exercises same as crunches and situps. nevertheless, Axial back extension strengthening exercises should be added to the program, in accordance with the patient’s pain tolerance. Weight-bearing exercises should be included to minimize the effects of osteoporosis, still, submarine exercises and balance training are also salutary.
Patients diagnosed with osteopenia or osteoporosis should be on anti-osteoporotic medicines, including alternate-generation bisphosphonates, as well as( daily) with 1500 mg of essential calcium and 400 IU of vitamin D.
Most vertebroplasty procedures are performed demanding a short inpatient stay.
Post-op treatment should be geared towards home safety training if the patient is at high threat for falls( Berg Balance Scale> 40), pain care, and transfer training. Rehabilitation at this stage should concentrate not only on recovery but must also averting. The following modalities should be included in the program with a gradational increase in intensity depending on the patient’s tolerance.
- Strengthening Exercises- particularly of the back extensors can help not only with pain care and with perfecting posture
- Weight-bearing Exercises- should be included in the program as mechanical loading will stimulate osteogenesis( Wolff’s law), perfecting bone quality and reducing the threat of( or worsening) osteoporosis.
- Stretching- Care requires to be taken not to overstretch, especially spinal flexion, as this might alter the defensive mechanisms against back pain.
- Pain Management- advice on the usage of heat & ice
- Advice and transfer practice- educating the customer on how to move from one position to another may help to minimize unessential load on the spine
- Homemade handling training and conditioning of day-to-day living-correct methods on lifting and diurnal tasks can help reduce the load on the spine and other joints
- Balance and Proprioception Training- This is specially salutary for guests who are at threat of falling
- Posture Re-education- embracing correct posture at rest and when active can help to reduce the stress on the spine, muscles, and ligaments.
At each step of the program, the patient should be treated like an individual and their position of pain, function, and lifestyle should be taken into account. Close monitoring is necessary to assure that the program is progressing in agreement with the patient’s status and needs.
Conclusion
A compression fracture is a result of weakened bones. Patients who have one compression fracture have a higher risk of more fractures in the future. That’s why it’s important to also diagnose and treat the cause of bone weakness.
Percutaneous vertebroplasty is widely accepted as a safe and effective therapeutic option for the treatment of painful osteoporotic and malignant VFs that fail to respond to optimal medical therapy. Appropriate patient selection, pre-procedure evaluation, and meticulous attention to the proper procedure are paramount to achieving the best outcomes & minimizing complications. As existing research has shown conflicting outcomes, additional research will likely be needed to conclusively establish the efficacy of vertebroplasty. Until then, patients should be treated in the context of a collaborative and multidisciplinary approach, and in the setting of appropriate informed consent. They most frequently need fewer pain medicines and can move better than before.
Patients who have this procedure frequently have less pain & better quality of life after the surgery.
FAQs
Percutaneous Vertebroplasty: New Treatment for Vertebral compression fracture
The success rate for this approach in treating osteoporotic fractures is 73 to 90 %.
Significantly, the Vertebroplasty procedure cost in India might range from INR 2,55,000 to INR 4,00,000.
This technique is usually completed within one hour. It might take longer if more than one vertebral body level is being treated.
Vertebroplasty is an image-guided, minimally invasive technique and is most frequently performed by a specially trained interventional radiologist or neuroradiologist in an interventional radiology or neuroradiology suite, or sometimes in an operating room.
The Vertebroplasty approach is done near the spinal cord and other important nerves, so a mistake in the needle’s placement could potentially outcome in damage that causes weakness & paralysis of one or more limbs.
Generally, diagnostic evaluation of this recurrent pain demonstrates a new compression fracture at a different vertebral level, & most of these patients have benefited from a repeated approach performed at the newly fractured level.