Osteoporosis : Physiotherapy Treatment:
Table of Contents
Introduction:

Osteoporosis is defined as low bone mineral density caused by altered bone micro-structure ultimately predisposing patients to low-impact, fragility fractures.
Normal bone is composed of protein, collagen, and calcium, all of which give bone its strength. Bones that are affected by osteoporosis can break (fracture) with relatively minor injuries that normally would not cause a bone to fracture. The fracture can be either in the form of cracking (as in a hip fracture) or collapsing (as in a compression fracture of the vertebrae of the spine). The spine, hips, ribs, and wrists are common areas of bone fractures from osteoporosis although osteoporosis-related fractures can occur in almost any skeletal bone.
Osteoporotic fractures lead to a significant decrease in quality of life, with increased morbidity, mortality, and disability. Over 50% of postmenopausal white women will have an osteoporotic-related fracture. Only 33% of senior women who have a hip fracture will be able to return to independence.
Classification of Osteoporosis :
Primary Osteoporosis:
- Affects mainly in adults
- Idiopathic

Type 1 ( postmenopausal) Osteoporosis:
- Usually affects females ages 51 to 75
- Related to the loss of estrogens protective effect on bone
- Results in trabecular bone loss and some cortical bone loss
- vertebral and wrist fractures are common.
Type 2 (senile) Osteoporosis:

- Occurs most commonly between ages70 to 85
- Trabecular and cortical bone loss
- Fractures of the proximal humerus,proximal tibia,femoral neck,and pelvis.
Secondary Osteoporosis:
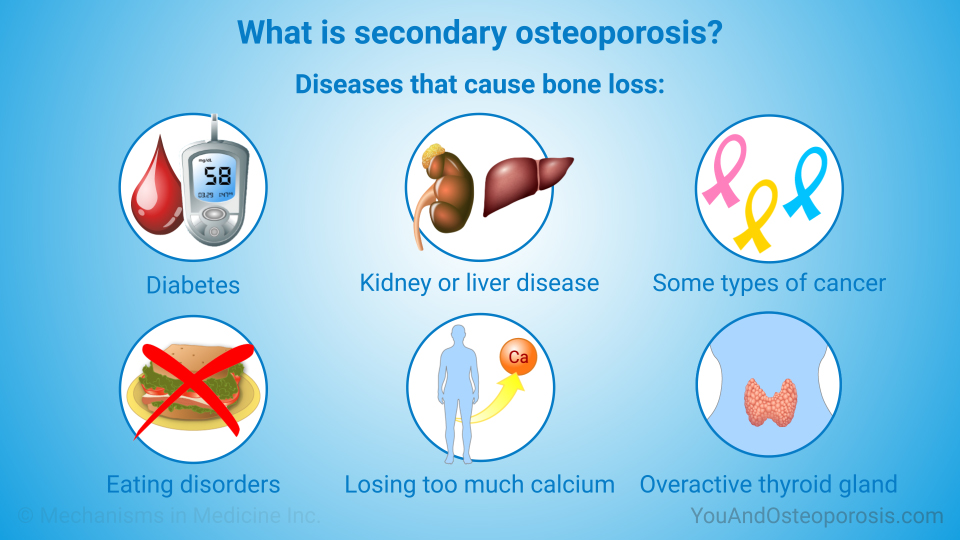
Secondary Osteoporosis is caused by prolonged use of medications or secondary to another disease or condition which inhibits the absorption of calcium or impedes the body’s ability to produce bone.
Low calcium intake or absorption can greatly increase one’s risk of developing osteoporosis. Life-long calcium intake is crucial in building up bone stock prior to peak levels of bone mass, as well as to maintain bone mass after the age of 20. Excessive alcohol consumption can decrease the body’s ability to absorb calcium.
Bone responds to the load applied to it. Physically active individuals typically have higher bone density, than those who have a sedentary lifestyle.
Hormone levels, either too little or too much, can impede the body’s ability to produce and maintain adequate bone mass. Dysfunction with sex glands, thyroid, parathyroid, or adrenal glands is often associated with osteoporosis.
Types of secondary osteoporosis:
- Endocrine origin
- Hypogonadism
- Hypercortisolism
- Hyperthyroidism
- Hyperparathyroidism
- Hyperprolactinemia
- Diabetes mellitus
- Gastrointestinal diseases
- Chronic inflammatory bowel disease
- Mal absorption
- Malnutrition
- Primary biliary cirrhosis
- Lactose intolerance
- Rheumatological and connective tissue diseases
- Immobilization
- Chronic alcoholism
- Organ Transplantation
Which are the Causes of Osteoporosis ?
There are some causes that will increase the risk of developing osteoporosis:
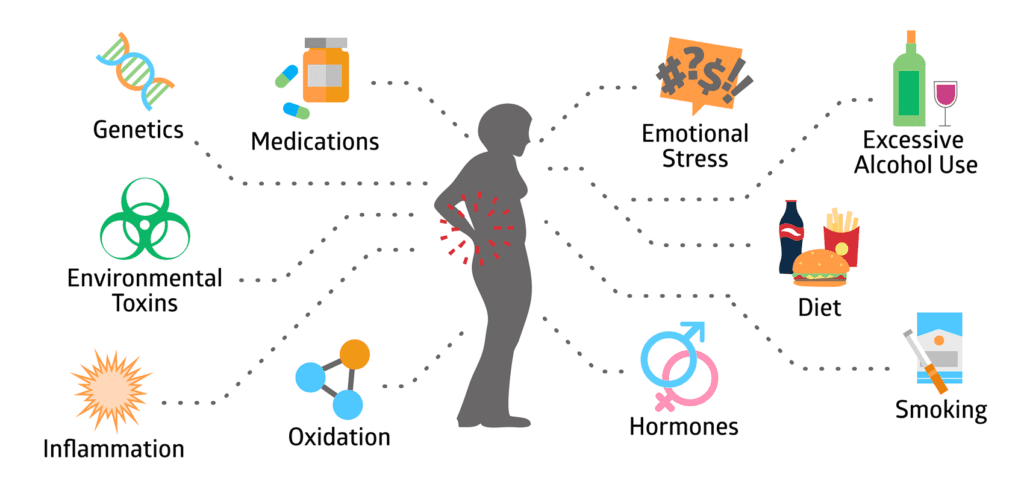
- Most common in females
- Caucasian or Asian race
- Thin and small body frame
- Family history of osteoporosis .for example, having a mother with an osteoporotic hip fracture doubles your risk of hip fracture.
- Personal history of fracture as an adult
- Cigarette smoking
- Excessive alcohol consumption
- Lack of exercise
- Diet low in calcium
- Poor nutrition and poor general health, especially associated with chronic inflammation or bowel disease
- Mal-absorption (nutrients are not properly absorbed from the gastrointestinal system) from bowel diseases, such as celiac spure that can be associated with skin diseases, such as dermatitis herpetiformis
- Low estrogen levels in women (which may occur in menopause or with early surgical removal of both ovaries)
- Low testosterone levels in men (hypogonadism)
- Chemotherapy that can cause early menopause due to its toxic effects on the ovaries
- Amenorrhea
- Chronic inflammation, due to chronic inflammatory arthritis or diseases, such as rheumatoid arthritis or liver diseases
- Immobility
- Hyperthyroidism,
- Hyperparathyroidism
- vitamin D Deficiency
- Certain medications can cause osteoporosis such as phenytoin (Dilation) and phenobarbital, and long-term use of oral corticosteroids (such as prednisone).
- Inherited disorders of connective tissue, including osteogenesis imperfect, homocystinuria, osteoporosis-pseudoglioma syndrome, and skin diseases, such as Mar-fan syndrome and Ehlers-Danlos syndrome (These causes of hereditary secondary osteoporosis each are treated differently.)
Symptoms:
There typically are no symptoms in the early stages of bone loss.That is why it is sometimes called a silent disease. However, you should watch out for the following things:

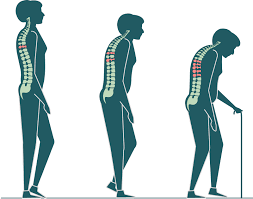
- Back pain, caused by a fractured or collapsed vertebra
- Loss of height over time
- A stooped or Bending forward posture
- A bone that breaks much more easily than expected
- Shortness of breath (smaller lung capacity due to compressed disks).
- Symptoms of severe osteoporosis can include a fracture from a fall or even from a strong sneeze or cough.
Diagnosis:

- A doctor will consider family history and any risk factors. If they suspect osteoporosis, they will request a bone mineral density scan (BMD).
- Bone density scanning uses a type of X-ray known as dual-energy X-ray absorptiometry (DEXA).
- DEXA can indicate the risk of osteoporotic fractures. It can also help monitor a person’s response to treatment.
Two types of devices can carry out a DEXA scan:
A central device:
This is a hospital-based scan that measures hip and spine bone mineral density while the individual lies on a table.
A peripheral device:
This is a mobile machine that tests bone in the wrist, heel, or finger.
DEXA test results
Doctors give the results of the test as a DEXA T score or a Z score.
The T score compares an individual’s bone mass with the peak bone mass of a younger person.
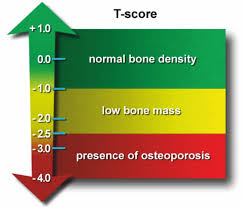
- -1.0 or above shows good bone strength
- from -1.1 to -2.4 suggests mild bone loss (osteopenia)
- -2.5 or below indicates osteoporosis
- The Z score compares the bone mass with that of other people of a similar build and age.
- A doctor will typically repeat the test every 2 years as this allows them to compare results.
Other tests:
- An ultrasound scan of the heel bone Trusted Source is another method that doctors use for assessing osteoporosis, and they can carry it out in the primary care setting. It is less common than DEXA, and the doctors cannot compare the measurements against DEXA T scores.
Osteoporosis Treatment:
Aim of treatment:
- slow or prevent the development of osteoporosis .
- maintain healthy bone mineral density and bone mass.
- prevent fractures .
- reduce pain .
- maximize the person’s ability to continue with their daily life .
- People at risk of osteoporosis and fractures can use preventive lifestyle measures, supplements, and certain medications to achieve these goals.
Medical Management:

A number of different medicines are used to treat osteoporosis:
- Bisphosphonates
- Parathyroid hormone
- Calcium and vitamin D supplements
- HRT (hormone replacement therapy)
- Diet and Nutrition
- In men, testosterone treatment can be useful when osteoporosis is caused by low levels of male sex hormones.
Physiotherapy Management:

Physical therapy intervention for individuals with osteoporosis, or even osteopenia, should include:
- Follow a healthy diet that includes enough calcium and Vitamin D
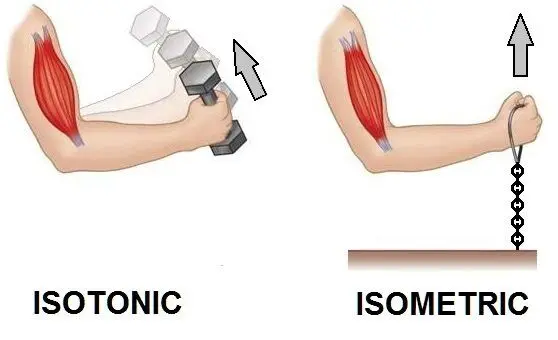
- Weight-bearing exercises
- Exercises such as walking or hopping, has been shown to maintain or improve bone density
- Strengthening exercises, using weights or resistance bands, have also been used to maintain or improve bone density
- Flexibility and strengthening exercise to improve the individual’s overall physical function and postural control. eg Tai chi, Yoga .
- Improving Balance exercises are important to prevent the risk of falls
- Postural exercise to prevent structural changes that often accompany osteoporosis, such as thoracic kyphosis
- Every osteoporosis program should include extension exercises such as chin tucks, scapular retractions, thoracic extensions, and hip extensions
- Wear sensible, well-fitting shoes to avoid falls
- Avoid rugs and sloppy slippers
- Have good lighting on stairs
- Try to avoid heavy lifting
- Physiotherapists may treat patients with osteoporosis for back pain
- Agility training, resistance training, and stretching have all been shown to decrease back pain and related disabilities
- High-intensity training – Research highly supports high-intensity training in the prevention of bone loss for women in menopausal years and the early post-menopausal period
- Dynamic weight-bearing, low force exercise has moderate positive effects on the spine
- Non-weight-bearing, high force exercises were shown to have moderate effects on the femoral neck
In progression exercises should be suggested such as :

- walking
- Jogging
- Going on a short, easy hike
- Climbing stairs
- Yoga
- Pilates
Prevention:

- have a healthy and varied diet with plenty of fresh fruit, vegetables and whole grains.
- eat calcium-rich foods.
- absorb enough vitamin D.
- Avoid smoking As Smoking increases rates of bone loss and the chance of fracture.
- Avoid excessive alcohol. Consumption of alcohol decrease bone formation and also increase the risk of falling.
- To prevent falls Wear low-heeled shoes with nonslip soles . Keep rooms brightly lighten, install grab bars just inside and outside of shower door.
- do regular weight-bearing and strength-training activities.


37 Comments