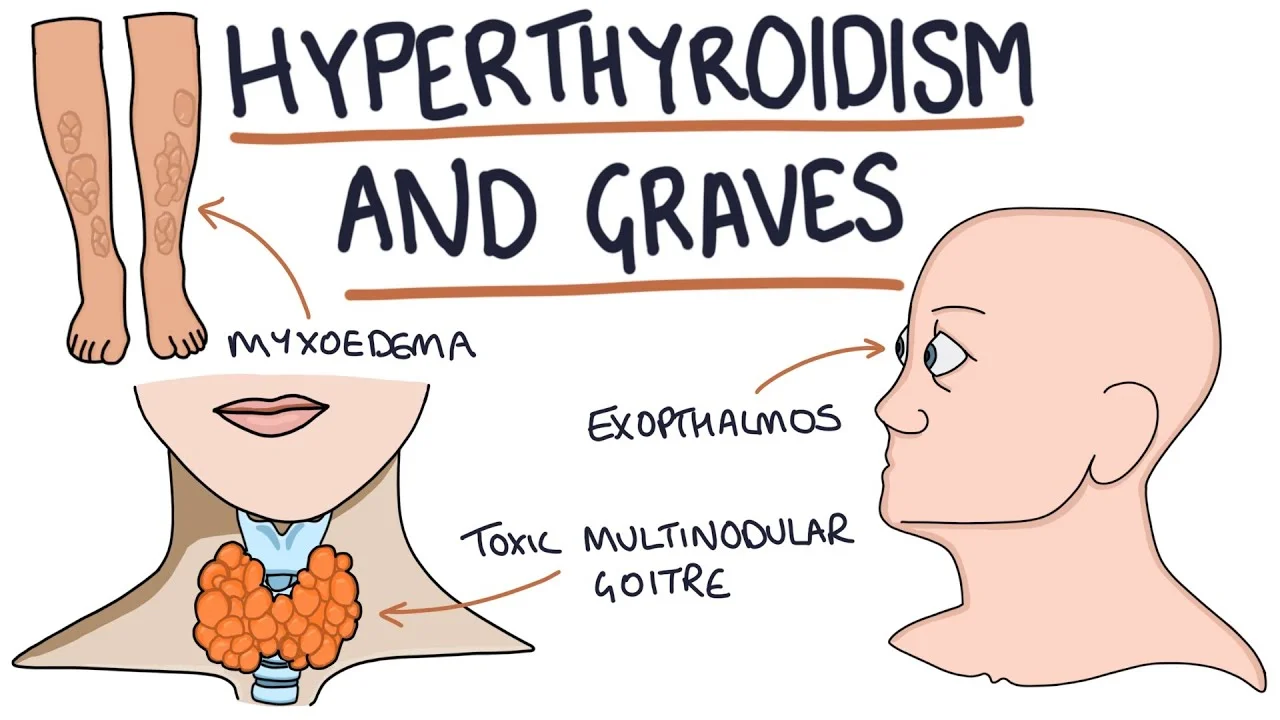
Hyperthyroidism
- Hyperthyroidism, known as overactive thyroid, is a condition where your thyroid creates and releases high levels of thyroid hormone. This condition can create your metabolism to speed up. Symptoms of hyperthyroidism involve a rapid heartbeat, weight loss, increased appetite, and anxiety. Hyperthyroidism treatment is antithyroid drugs, beta-blockers & surgery.
Table of Contents
What is hyperthyroidism?
- Hyperthyroidism is a condition in which your thyroid makes and releases more hormones than you need. This is known as an overactive thyroid. The main hormones your thyroid makes involve triiodothyronine (T3) and thyroxine (T4).
- Hyperthyroidism can affect your whole body and is a condition that needs to be treated by a healthcare provider.
What does my thyroid do?
- Located at the forward of your neck, the thyroid is a butterfly-shaped gland. Glands are organs that can be found whole over your body. Some of your glands make and release hormones — substances that assist your body’s function and growth.
The thyroid gland plays a big part in many of your body’s important functions, involving:
- Controlling your body temperature,
- Controlling your heart rate (HR),
- Controlling your metabolism (the process that transforms the food you put in your body into energy that assists your body function).
- When your thyroid gland is working correctly, your body is in balance, and the whole of your system functions properly. If your thyroid stops working the way it is meant to — creating too much or too little thyroid hormones — it can impact your entire body.
What is the difference between hyperthyroidism and hypothyroidism?
- Hyperthyroidism and hypothyroidism are medical conditions that both have to do with the amount of thyroid hormone your thyroid creates and releases — the difference is how much.
- Picture something connected to the word “hyper.” Most such as you just thought of something fast or full of a lot of energy. When you have hyperthyroidism, your thyroid is overactive and creates and releases very much thyroid hormone.
- In the medical world, the title “hypo-” means “low” or “not enough.” When you have hypothyroidism, your thyroid is underactive and does not make and release enough thyroid hormone that your body needs.
Who gets hyperthyroidism?
- Anyone can have hyperthyroidism, but it is more common in females.
How common is hyperthyroidism?
- Hyperthyroidism is relatively infrequent. Around 1% of people in the United States (US) have hyperthyroidism.
What are the symptoms of hyperthyroidism?
- There are so many symptoms of hyperthyroidism, and they can affect your whole body. You may experience certain of these symptoms and not others or many of them at the same time.
Symptoms of hyperthyroidism can involve:
- Rapid heartbeat (palpitations),
- Feeling shaky and/or nervous,
- Weight loss,
- Increased appetite,
- Diarrhea & more frequent bowel movements,
- Vision changes,
- Thin, warm & moist skin,
- Menstrual changes,
- Intolerance to heat & excessive sweating,
- Sleep issues,
- Swelling & enlargement of the neck from the enlarged thyroid gland (goiter),
- Hair loss & change in hair texture,
- Bulging of the eyes (looked with Graves’ disease),
- Muscle weakness.
What causes hyperthyroidism?
Medical conditions and situations that can cause hyperthyroidism to involve:
- Graves’ disease: In this disorder, your immune system harms your thyroid. This creates your thyroid creates too much thyroid hormone. Graves’ disease is a hereditary condition (passed down across a family). If a member of your family has Graves’ disease, there is a chance others in the family could have it, too. It is more common in people assigned females at birth than people assigned males at birth. Graves’ disease is the most usual cause of hyperthyroidism, making up about 85% of cases.
- Thyroid nodules: A thyroid nodule is a hunk or growth of cells in your thyroid gland. They can create more hormones than your body needs. Thyroid nodules are infrequently cancerous.
- Thyroiditis: Thyroiditis is swelling of your thyroid gland, which may be painful or painless (silent). It may occur within a year of delivering a baby (postpartum thyroiditis). Later you experience thyroiditis, and your thyroid may be unable to recover, which would lead to hypothyroidism.
- Consuming excess iodine: If you are at risk for hyperthyroidism and consume too much iodine (through your diet or medications), it can cause your thyroid to create more thyroid hormones. Iodine is a mineral that your thyroid utilizes to create thyroid hormones. Receiving intravenous iodinated contrast (iodine “dye”) may cause hyperthyroidism. Amiodarone, a medication that contains a high amount of iodine, may cause hyperthyroidism.
How is hyperthyroidism diagnosed?
Your healthcare provider can diagnose hyperthyroidism in several ways, involving:
- A physical exam of your neck to look if your thyroid is larger than normal.
- Blood tests to see for high levels of thyroid hormone in your body.
- Imaging tests to see your thyroid.
Physical exam for diagnosing hyperthyroidism
If you are experiencing symptoms of hyperthyroidism, your healthcare provider may check the following during a physical exam in their office:
- Your thyroid: Your provider may gently feel your thyroid through the outside of your neck to check if it is enlarged, bumpy, or tender.
- Your eyes: Your provider (doctor) may check your eyes for swelling, redness, bulging and other signs of Graves’ eye disease.
- Your heart: Your provider may utilize a stethoscope to listen to your heart for a rapid and/or irregular heartbeat.
- Your hands: Your provider may have you outstretch your hands to look if you have a tremor. They may also see for changes in your fingernails.
- Your skin: Your provider may feel your skin to see if it is warm and moist.
Blood tests for diagnosing hyperthyroidism
- Your healthcare provider may take a blood sample to see for high levels of thyroid hormone. This is known as thyroid function testing. When you have hyperthyroidism, levels of the thyroid hormones T3 and T4 are above normal and thyroid-stimulating hormone (TSH) is decreased than normal.
Imaging Tests for diagnosing hyperthyroidism
- Taking a closer look at your thyroid can assist your provider to diagnose hyperthyroidism and its possible cause of it.
Imaging tests your provider could use to examine your thyroid involve:
- Radioactive iodine uptake (RAIU) test: For this test, you will take a small, safe dose of radioactive iodine (also called a radiotracer) by mouth to see how much of it your thyroid absorbs. Later a certain amount of time — usually six and 24 hours later — your healthcare provider will scan your neck with a device known as a gamma probe to look at how much of the radioactive iodine your thyroid has absorbed. If your thyroid has absorbed a lot of the radioactive iodine, it means that your thyroid gland is creating too much thyroxine (T4). If this is the case, you most such as have Graves’ disease or thyroid nodules.
- Thyroid scan: This procedure is an extension of the RAIU, where in addition to measuring the absorbed amount of radioactivity by your thyroid, you will lie on a table with your head tilted back while a special camera (gamma camera) gets several images of your thyroid. The radioactive material makes all or certain areas of your thyroid appear “bright” on the screen. Your provider may utilize a thyroid scan to look for lumps or nodules on your thyroid, inflammation, swelling, goiter, or thyroid cancer.
- Thyroid ultrasound: An ultrasound utilizes high-frequency sound waves to create images of your thyroid. It is a non-invasive procedure that allows your provider to look at your thyroid on a screen. Your provider may utilize this test to look for nodules on your thyroid.
How is hyperthyroidism treated?
- There are so many treatment options for hyperthyroidism. Depending on the cause of your hyperthyroidism, certain options may be better for you. Your healthcare provider will discuss each option with you and assist you to determine the best treatment plan.
Treatment options for hyperthyroidism involve:
- Antithyroid drugs methimazole (Tapazole) or propylthiouracil (PTU): These drugs choke the ability of your thyroid to create hormones. They offer quick control of your thyroid.
- Radioactive iodine: Radioactive iodine is an oral medication that your extractive thyroid cells absorb. The radioactive iodine harms these cells and causes your thyroid to shrink and thyroid hormone levels to go down over a few weeks. This commonly leads to permanent destruction of the thyroid, which will cure hyperthyroidism. The amount of radiation delivered by this medication varies from the amount used for the radioactive iodine uptake (RAIU) test and scan for diagnosis. This treatment has to take thyroid hormone drugs for the rest of their lives to maintain normal hormone levels.
- Surgery: Your healthcare provider (doctor) may remove your thyroid gland through surgery (thyroidectomy). This will correct your hyperthyroidism, yet it will usually cause hypothyroidism (an underactive thyroid), which requires lifelong thyroid supplements to keep hormone levels normal.
- Beta-blockers: These drugs choke the action of thyroid hormones in the body. They do not change the level of hormones in your blood, yet they can help manage symptoms such as rapid heartbeat, nervousness, and shakiness that are caused by hyperthyroidism. This treatment is not used alone and is commonly paired with another option to treat hyperthyroidism over the long term.
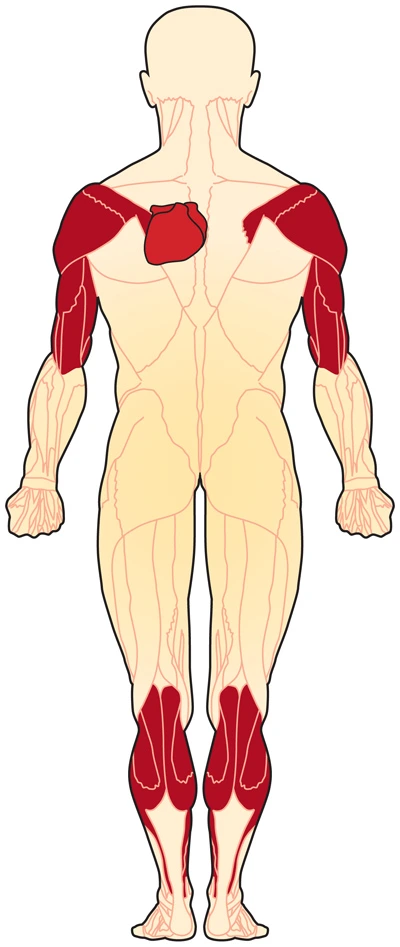
Physiotherapy treatment
- Hyperthyroidism has key elements that will cause a reduced tolerance to physical activity. Therapists should be sensitive to patient complaints and symptoms to note an exacerbation if the patient is already diagnosed or be able to acknowledge symptoms in order to refer to a physician.
What Should I Monitor During Treatment Session?
- Vital Signs: This is especially important if the patient is an older adult, has coronary artery disease (CAD) or previous hx of heart disease, or presents with signs of dyspnea, fatigue, tachycardia, and/or arrhythmia.
- Watch for signs of hypoparathyroidism like muscular twitching, tetany, numbness, and tingling around mouth, fingertips, or toes if the patient is post thyroidectomy. Hypoparathyroidism may result in 1-7 days after thyroidectomy if there are complications during the surgery resulting in unintentional removal of part of the parathyroid glands.
Safety Precautions for Therapists
- When working with patients who have been given RAI, be aware their saliva is radioactive for 24 (twenty-four) hours following their treatment. When working with these patients it is main to take the necessary precautions if the patient is coughing or expectorating.
- Monitor for heat stress,
- Hyperthyroidism and Exercise.
- Some patients with Graves’ disease suffer from heat intolerance, creating exercising in a hot pool a contraindication to therapy. This patient would until be able to participate in aquatic therapy in a warm pool; given the patient’s body temperature is being monitored. Typically heat intolerance is associated with thyroid storm, and will normally not happen in clients attending therapy in outpatient settings.
- Hyperthyroidism is associated with exercise intolerance and decreased exercise capacity.
- Many patients with hyperthyroidism suffer from cardiopulmonary complications often leading to atrial fibrillation, CHF, and an improved risk of a MI.
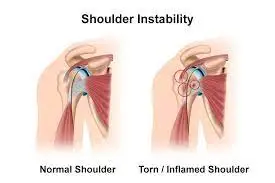
- 70% of people with hyperthyroidism develop proximal muscle weakness as an outcome of treatment, most often affecting the pelvis and thigh muscles
- Graves’ disease is associated with a decrease in bone mineral density (BMD) and has also been shown to be a risk factor for hip fractures.
How long does it take to treat hyperthyroidism?
- The amount of time it takes to treat hyperthyroidism can change turning on what caused it. If your healthcare provider (doctor) treats your condition with antithyroid medications (methimazole or propylthiouracil) your hormone levels should drop to a healthy level in about 6 to 12 weeks.
- Your healthcare provider (doctor) may decide to give you great doses of iodine drops (not radioactive), which would normalize thyroid levels in 7 to 10 days. However, this is a short-term solution, and you will most likely need a more lifelong solution such as surgery. Though you may require to wait to be scheduled for thyroid surgery (thyroidectomy), this is a very powerful and definitive way to treat hyperthyroidism. It is considered a permanent solution for hyperthyroidism.
Are there any risks to hyperthyroidism treatments?
- With most treatments, there are risks of side effects. It is important to tell your healthcare provider (doctor) & weigh all of the advantages and disadvantages previous choosing a treatment plan.
Some of these risks involve:
- Medication side effects: The 2 medications that can treat hyperthyroidism are methimazole and propylthiouracil (PTU). These drugs can cause too many side effects. One infrequent side effect that affects decrease than 1% of people is potential liver damage, which may be permanent in the case of PTU. Another rare (less than 1%) yet serious side effect is agranulocytosis (severe drop in white blood cell count). These side effects can occur to people of any age. In pregnant people, this medication can towards from the parent to the fetus through the placenta. This could cause hypothyroidism or the growth of a goiter in the fetus. Pregnant people are nearly monitored because of this side effect. There is also a possibility of an allergic reaction to these medications, which occurs in about 5% of people.
- Radioactive materials: Whenever radiation is involved, there is a possible side effect of cancer. Currently, there is no link between using radioactive iodine to treat hyperthyroidism and developing cancer. This is considered decrease-risk and unlikely. One risk that is well known is between a pregnant or breastfeeding person and their baby. You should not take radioactive iodine while pregnant or breastfeeding because it can affect your baby’s thyroid gland. Sometimes, you can lose sensation in your mouth later radioactive iodine (RAI) therapy. This is usual. But do not worry — even though it can last for up to a few months, the sensation does come back to your mouth over time.
- Surgery: There are always certain risks linked to surgery, such as infection and bleeding. Surgery is commonly considered a very much effective treatment for hyperthyroidism. In rare situations, complications such as paralysis of the vocal cords (inability to speak) and damage to your parathyroid glands can happen, which results in low calcium in your blood.
- After treatment, you will most likely need to take replacement thyroid hormone for the rest of your life. This is because certain of these treatments — especially surgery — reduce your thyroid hormone levels to very low levels or eliminate this hormone by removing your thyroid. You will need to reintroduce the thyroid hormones back into your system by getting regular medication.
What happens if hyperthyroidism is left untreated?
- Hyperthyroidism can impact many parts of your body. Various systems, ranging from your vascular system (heart) to your skeletal system (bones) can all be affected if you have an overactive thyroid.
Complications from untreated or undertreated hyperthyroidism involve:
- Atrial fibrillation,
- Stroke
- Congestive heart failure
- Osteoporosis.
- If you are experiencing symptoms of hyperthyroidism, it is important to see your healthcare provider so they can determine a proper diagnosis and recommend treatment.
What are the risk factors for hyperthyroidism?
Some factors that could increase your risk of developing hyperthyroidism can involve:
- Having a family history of thyroid disease,
- Having a medical history that involves conditions such as pernicious anemia, Type 1 diabetes, and primary adrenal insufficiency (Addison’s disease),
- Having a lot of iodine (a mineral that your body utilizes to make thyroid hormones) in your diet,
- Being pregnant.
What is the outlook (prognosis) for hyperthyroidism?
- Hyperthyroidism is a manageable & treatable condition, & most people carry it powerfully with a cure. While some forms of treatment need you to take medication for the rest of your life, your thyroid hormone levels will be normal.
- Unfortunately, untreated hyperthyroidism caused by Graves’ disease may acquire worse over time and cause complications. If you have Graves’ disease, ask your healthcare provider (doctor) questions about how you can best manage your condition.
Can hyperthyroidism be cured?
- Yes, there is a permanent treatment for hyperthyroidism. Removing your thyroid through surgery or destroying your thyroid through medication will prevent hyperthyroidism. However, once your thyroid is removed or destroyed, you will need to get thyroid hormone replacement medications for the rest of your life. Your body still requires thyroid hormones, just not at such high levels as you have in hyperthyroidism. Though you will need to get the medication & detect it with your healthcare provider regularly, this is a manageable form of thyroid disease.
Are there complications of hyperthyroidism?
- A thyroid storm (thyroid crisis or thyrotoxic crisis) is a rare yet serious complication of hyperthyroidism. It happens when your thyroid creates and releases a large amount of thyroid hormone in a short amount of time. A thyroid storm is a life-threatening emergency that requires immediate medical attention.
Symptoms of thyroid storm include:
- High fever — a temperature between 104 degrees to 106 degrees Fahrenheit is usual,
- Quick heart rate (tachycardia) that can exceed 140 beats per minute,
- Feeling agitated, irritable, and/or anxious,
- Delirium,
- Congestive heart failure,
- Loss of consciousness.
- A complication of Graves’ disease, one of the causes of hyperthyroidism, is known as Graves’ eye disease (Graves’ ophthalmopathy). This condition can commonly not be prevented.
Graves eye disease can cause the ensuing complications:
- Bulging eyes,
- Vision loss,
- Double vision,
- Light sensitivity.
When should I see my healthcare provider?
- If you are experiencing signs and symptoms of hyperthyroidism, it is important to see your healthcare provider so they can assess your condition and recommend treatment.
- If you have already been diagnosed with hyperthyroidism, you will likely need to see your provider regularly to make sure your treatment is working.
- If you are experiencing signs of thyroid storm, or a complication of hyperthyroidism, such as a high fever and a very fast heart rate, get to the nearest hospital as soon as possible.
Can hyperthyroidism cause female infertility?
- One of the symptoms of hyperthyroidism can be irregular menstrual cycles (periods), which can make it hard to get pregnant. Some people certainly begin thrusting out to their healthcare provider (doctor) because of issues becoming pregnant & then learning about the thyroid condition.
Can I develop hyperthyroidism during pregnancy?
- During early pregnancy, your body requires to produce more thyroid hormones than normal to help the developing fetus. These hormones are particularly main for the brain and nervous system. Having thyroid hormone levels that are a little higher than normal is all right, yet if your levels increase dramatically, your healthcare provider may need to form a treatment plan. High levels of thyroid hormones can impact not only you yet also the fetus.
- It can be hard to diagnose hyperthyroidism during pregnancy because your thyroid hormone levels naturally improve & the other symptoms of pregnancy mask signs of hyperthyroidism.
What foods should be avoided with hyperthyroidism?
- Eating very many iodine-rich or iodine-fortified foods in your diet may cause hyperthyroidism or create it worse in certain cases.
- If you have hyperthyroidism, your healthcare provider may recommend some changes to your diet. Always consult your provider or a registered dietician previous making drastic changes to your diet. If you take medication for your hyperthyroidism, always take the amount prescribed by your provider (doctor).
- According to the National Institutes of Health (NIH), the recommended everyday dose of iodine is about 150 micrograms (mcg). The daily dose is greater for pregnant people. A low-iodine diet requires an even decrease.
- Seafood has the most iodine. Just 1 gram of seaweed consists of 23.2 micrograms (mcg), or 0.02 milligrams (mg).
If your provider (doctor) or dietician has recommended a low-iodine diet, try to avoid the following seafood and seafood additives:
- Fish,
- Seaweed,
- Crab,
- Lobster,
- Sushi,
- Prawns,
- Algae,
- Alginate,
- Nori,
- Kelp.
Other foods have high amounts of iodine, involving:
- Milk and dairy products,
- Cheese,
- Egg yolks,
- Iodized salt.
Is hyperthyroidism the same thing as thyrotoxicosis?
- Hyperthyroidism is a type of thyrotoxicosis. Hyperthyroidism occurs specifically when your thyroid gland both produces and releases excess thyroid hormone. Thyrotoxicosis occurs when you have very much thyroid hormone in your body in general. You could have very much thyroid hormone by taking too much thyroid medication, for example. This would be thyrotoxicosis, not hyperthyroidism.
NOTE
- Getting the latest diagnosis can be stressful. The best news is that hyperthyroidism is a manageable and treatable condition. If you are experiencing symptoms of hyperthyroidism or have certain risk factors, such as a family history of Graves’ disease, be sure to contact your healthcare provider. They can have you undergo certain simple tests to see if your thyroid is making too much thyroid hormone.
FAQs
Graves disease (a most common cause of hyperthyroidism) Inflammation (thyroiditis) of the thyroid due to viral infections, some medicines, or later pregnancy (common) Taking too much thyroid hormone (common) Noncancerous developments of the thyroid gland or pituitary gland (rare).
About overactive thyroids
Extreme levels of thyroid hormones can then speed up the body’s metabolism, triggering a range of symptoms, such as nervousness and anxiety. hyperactivity – where a person can not stay still and is full of nervous energy. unexplained/unplanned weight loss.
Yes, there is a lifelong treatment for hyperthyroidism. Removing your thyroid through surgery or destroying your thyroid through medication will prevent hyperthyroidism. However, once your thyroid is removed or destroyed, you will need to get thyroid hormone replacement medications for the rest of your life.
Treatment may include:
Anti-thyroid medicine. These medications steadily ease symptoms of hyperthyroidism by preventing the thyroid gland from creating very many hormones.
Beta-blockers. These medicines do not affect thyroid hormone levels.
Radioiodine therapy. The thyroid gland takes up radioiodine.
Thyroidectomy.
Hyperthyroidism can occur at any age, yet it is more common in people aged 60 and older. Graves disease (one cause of hyperthyroidism) is more likely to happen between ages 40-60 years old.
Hyperthyroidism is sometimes treated with antithyroid drugs, which end the overproduction of thyroid hormone. If antithyroid drugs do not improve the state of the thyroid gland, hyperthyroidism could be cured with radioactive iodine. In certain cases, the thyroid gland might be surgically removed.
Hyperthyroidism caused by the overproduction of thyroid hormones can be treated with antithyroid medications (methimazole and propylthiouracil), radioactive iodine ablation of the thyroid gland, or surgical thyroidectomy. Radioactive iodine ablation is the most widely utilized treatment in the United States.





4 Comments