Shoulder Instability
Table of Contents
What is Shoulder instability?
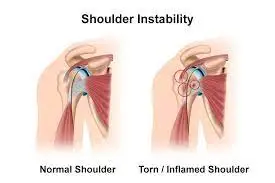
Shoulder instability mostly occurs when the head of the upper arm bone is displaced from the shoulder joint socket. This causes loss of shoulder movement with pain and other related symptoms.
What is the shoulder joint?
The shoulder is a ball-and-socket type of joint that allows a wide range of movement. Its bony structures include the upper arm bone (the humerus) and the shoulder blade’s shallow cavity (the glenoid).
The shoulder joint is formed up of three bones:
- Humerus: upper arm bone
- Scapula: shoulder blade
- Clavicle: collar bone
The humerus ball is indicated to stay near the socket, like a ball bearing in a holder. The humeral head is maintained into the socket by the lining of the joint (the capsule), thickenings of the capsule known as ligaments, and a cartilage rim (the labrum).
The bones in the shoulder are connected together by ligaments, and one of them is the coracoacromial ligament, which connects the acromion process and the coracoid process, bony projections off the scapula.
The acromion and the coracoacromial ligament develop a sort of bridge or roof over the top of the shoulder called the coracoacromial arch. The space below this arch is known as the subacromial space.
Each of the rotator cuff muscle tendons runs through the subacromial space and as the arm moves up and down, the rotator cuff tendons slide backward and forward through this space.
Between the subacromial space and the rotator cuff tendons are the subacromial bursa, which is a small fluid-filled sac that protects the tendons and prevents friction against the bone.
The space underneath the acromion is relatively small, and the gap gets narrower as you raise your arm up because of how the bones and tendons move.
Causes of Shoulder Instability
Shoulder instability often observes an injury that causes the shoulder to dislocate. This initial injury is usually fairly significant. It is critical that the shoulder be decreased, or put back in the socket. Sometimes people can achieve this on their own; however, often physician assistance is needed in the Emergency Department. Two damages happen with a dislocation that often shows recurrent dislocations.
- The labrum is often pulled out from the bone.
- The ligaments in the capsule are stretched (like a rubber band that has been overstretched- it becomes loose and floppy.) An unstable shoulder can result in repeated attacks of dislocation, even during normal activities.
In some cases, shoulder instability can occur without the last dislocation. People who do repeated shoulder movements may slowly stretch out the joint capsule. This is particularly common in athletes such as baseball pitchers, swimmers, and volleyball players. If the joint capsule gets stretched out and the shoulder muscles drain the ball of the humerus begins to drop around too much within the shoulder. Eventually, this can cause disturbance and pain in the shoulder.
A genetic problem with connective tissues of the body can show to ligaments that are too flexible. When ligaments pull too easily, they may not be able to maintain joints in place. All the joints in the body may be similarly flexible. Some joints, such as the shoulder, maybe smoothly dislocated. People with this type of problem are sometimes guided to double joints.
Classification:
It is classified into three types:
Anterior Instability
This occurs due to the translation of the humeral head in the anterior direction. It is the most common type of shoulder instability.
Posterior Instability
It accounts for 2-5 % of instability cases. Normally, the athletic population is influenced by this type of instability who participate in an overhead activity. Structural problems like posterior glenoid erosion and glenoid retroversion or deficiency of rotator interval can predispose patients to posterior instability.
Multidirectional instability (Atraumatic)
In this, there is a combination of anterior /posterior/inferior instability at the GH joint. In many of cases, this type of instability is because of generalized laxity throughout the body. Another cause is repetitive trauma during extremes of motion.
Mainly the pain is during the mid ranges of shoulder ROM which indicates the main role of altered muscle activation. The inappropriate position of the scapula can also be the reason for pain or any other symptoms.
Mechanism of Injury:
GH joint anterior dislocation
- Traumatic
The most common glenohumeral dislocation occurs anterior side, usually as a result of sporting accidents or falls, particularly when the upper extremity is placed in 90° abduction and external rotation.
Posterior dislocations most typically result from seizures, shock, and falls.
- Atraumatic
Chronic Recurrent
Abducted, extended shoulder – Tennis serve
Chronic recurrent caused by repetitive extreme external rotation with the humerus in abducted and an extended position(i.e.pitching motion). Instability may be caused by the gradual weakening of the anterior and inferior static restraints. The head o the humerus will tend to move away from shortened structures. For example, posterior shoulder capsular tightness will induce the humeral head to shift anteriorly, resulting in a loss of integrity of all anterior structures. Generally, it is associated with participation in sports such as Gymnastics, Baseball, Softball, Tennis, Swimming, and Weight training.
Common accompanying features or causes are :
- Bankart lesion
- HillSachs lesion
- SLAP lesion (Superior Labrum Anterior Posterior)
- HAGL lesion (Humeral Avulsion of Glenohumeral Ligaments)
- ALPSA lesion (Anterior Labroligamentous Periosteal Sleeve Avulsion)
- Laxity of the joint capsule
Pain in the Right shoulder after repetitive shoulder posterior dislocation.
Congenital Instability
Congenital instability may be the result of:
- Glenoid hypoplasia is also called glenoid dysplasia. It is an uncommon congenital condition that occurs due to the underdevelopment of the inferior glenoid ossification center.
- Lessen anterior-posterior diameter of the glenoid
- Increased retroversion of glenoid part
- Increased quantity and composition of collagen and elastin
- Bony abnormalities
Signs and Symptoms of shoulder instability:
The most common signs of shoulder instability are:
- Repeat instances of a dislocated shoulder
- Shoulder pain due to injury
- A loose or hanging feeling in the shoulder joint
- The sensation of your arm bone slipping out of joint
Risk Factors for Shoulder Dislocation
Apart from participation in reference marks, there are three factors that can make the shoulder joint weak to dislocations:
1. Repetitive overhead exercise
A repetitive shoulder sign can cause the ligaments wrapping the shoulder’s socket to stretch. Strained and lengthened shoulder tissue from redundant motion can leave the shoulder mutually slightly stabilized, which may show shoulder instability.
Shoulder instability due to repetitive use is sometimes referred to as a micro-traumatic dislocation. Those at risk for a micro traumatic dislocation include participants in sports with a lot of overhead motion, including swimming, volleyball, and baseball.
2. Previous dislocation
Behind the first dislocation, the shoulder is much weaker to a recurring dislocation—especially for younger patients. In fact, some assessments show that patients younger than 20 have a reproduction rate of up to 90%. 1 The first dislocation can pull the tissues covering the shoulder joint, pushing the shoulder to be unstable and resulting in another dislocation. The medical term for recounted shoulder dislocations is chronic shoulder instability.
3. Genetics
Some people unaffectedly have more flexible, malleable connective tissues in the body, including those who may be directed to as “double-jointed.” They may participate in a shoulder dislocation without substantial injury or pain. These people may also be more possible to experience subluxations (partial dislocations) in which the joint slips back into place by itself. Many individuals with this illness or generalized laxity learn how to push the shoulder back in place themselves
Complications:
Complications of a dislocated shoulder might include:
- Tearing of the muscles, ligaments, and tendons that reinforce the shoulder joint
- Nerve or blood vessel injury in or near the shoulder joint
- Becoming more prone to repeat dislocations, especially if the injury is severe
- Pulled or torn ligaments or tendons in the shoulder or harmed nerves or blood vessels around the shoulder strength need surgery for rehabilitation
Diagnosing:
Diagnosing shoulder instability often begins with a material exam by a doctor. A doctor will check for disadvantages, range of signs, and looseness. They will also ask you about damages and shoulder instability history.
For a more detailed look at the shoulder, a physician may operate further testing:
- Magnetic resonance imaging (MRI) or calculated tomography scan (CT scan)
- MRI or CT scan can be performed after the dye is injected into the shoulder joint (arthro-MRI or arthro-CT)
- Examination under anesthesia followed by arthroscopy
Special tests are used to evaluate for shoulder instability including the sulcus sign, anterior apprehension, and relocation. Classically, these tests are positive for shoulder instability:.
- Sulcus sign: The patient sitting in an upright position with the arm resting at their side. The clinician stabilizes the shoulder proximally and applies pressure inferiorly directed at the elbow. A positive test is documented based on the inferior displacement of the humeral head.
- Anterior apprehension test: The patient lying in the supine position, this test is performed by positioning the patient’s shoulder in 90 degrees of abduction and 90 degrees of external rotation. While holding the proximal shoulder, the clinician applies greater gentle external rotation movement. The test is considered positive if the patient reports a subjective feeling of impending subluxation or near dislocation.
- Relocation test: The relocation test is for shoulder instability and it requires a positive anterior apprehension test. After the patient complains of the prodrome of dislocation or subluxation described above. The clinician applies a force in the posterior direction on the anterior humeral head, which relieves the patient’s symptoms.
Treatment for Shoulder Instability
Non-surgical Rehabilitation :
Even nonsurgical treatment for shoulder instability usually needs a medical treatment and rehabilitation program which includes physical therapy. The purpose of Physical Therapy is to support the rotator cuff and shoulder edge muscles to make the shoulder more long-lasting.
Treatment of instability can range from simple home treatment such as aspirin and rest to surgery, relying on how severe the instability is.
Conservative treatments are efficacious for many people to relieve pain. Many cases respond sufficiently to conservative treatment within a year. Negligible cases may settle more quickly.
Conservative treatment for shoulder impingement:
- Rest
- Medication including nonsteroidal anti-inflammatory drugs (NSAIDs)
- Heat
- Physical therapy
Physical therapy comprises gentle exercises to increase the strength of the muscles in the shoulder and restore the range of motion in the shoulder
Home treatment:
Use of RICE Principle:
REST: Rest is very compulsory when it comes to treating shoulder impingement. Bypass any laborious exercise or any movements that make the pain worsen. This is especially important if a person is an athlete or sport.
While it is good to not move the shoulder too much, avoid using a sling to immobilize the arm fully. Immobilization can direct to more weakness and stiffness in the shoulder.
Ice Therapy: Using an ice pack regularly for 10-15 minutes at a time can help relieve pain and inflammation. Ice packs should be covered in a towel and placed over the shoulder for 10 minutes, 3-4 times daily. To relieve pain and any swelling around the shoulder a patient might have.
Compression: To reduce swelling and pain
Elevation: To reduce swelling in the shoulder.
Medical Treatment:
The doctor will recommend nonsteroidal anti-inflammatory drugs, such as ibuprofen. These medicines can help lessen swelling and shoulder pain. If these medications taken along with ice and rest, don’t lessen the pain, a doctor might prescribe steroid injections to reduce swelling and pain.
Injections: Corticosteroid injections may help to lower inflammation in the tendons or bursa. A mixture of steroids and local anesthetic is injected or infiltrated into the pain area. Care is needed after taking the injection. Initially, the injection temporarily weakens the tendon rising the risk of rupture.
Injections should not be used as a stand-alone treatment, they should be obeyed by a course of physical therapy to ensure the problem does not return.
Physical Therapy:
After conservative treatment physical therapy is usually prescribed, which involves strengthening the rotator cuff muscles and strong scapular muscles to help regain strength and stability in the shoulder joint. This will ultimately help the patient regain full motion, reduce the sensation that the shoulder is unstable, and hopefully allow a return to a normal activity level. Therapy is usually less effective for the younger and more athletic population.
A physiotherapist will first help the patient to control her pain and rash. The initial treatment that we suggest to manage pain usually leaves an anti-inflammatory prescription, such as aspirin or ibuprofen. Ensure that you confer with your doctor or pharmacist regarding the use of pain comfort or anti-inflammatory medication.
To reduce swelling, inflammation, and pain, physiotherapists give treatment with modalities followed by exercises.
Modalities include:
Interferential therapy
Ultrasound: Ultrasound is typically an in-clinic option only that can be used for the first several weeks to kickstart the healing procedure. Ultrasound is an excellent option for a localized and very specific source of pain, such as rotator cuff tendinitis or bursitis condition in the shoulder.
TENS unit
A TENS unit can be used in the physiotherapy clinic to help ease pain and improve tolerance for the rest of the treatment session. A Physiotherapist will demonstrate to you where to put the pads for maximal comfort. If a person is getting satisfactory results, they can then recommend what options are best for the patient.
Short wave diathermy: It is a deep heating modality that helps to reduce pain.
Ice and heat
A physical therapist will suggest you determine how long, the exact placement, and how often you should apply ice and/or heat to the shoulder.
-Hot pack to reduce pain
-Cold pack to reduce swelling and pain.
The physical therapist will show the patient ways to avoid positions and activities that put the shoulder in further danger of injury or dislocation. We may allocate overhand athletes a special shoulder belt or sleeve to stop the shoulder from moving in ways that test it.
Exercises:
We use hands-on treatments and various types of exercises to enhance the range of motion in your shoulder and nearby joints and strengths. Later, you will do maintaining exercises to improve the strength and power of the rotator cuff and shoulder blade muscles. A Physical Therapist will help you retrain these muscles to maintain the ball of the humerus in the socket. This will improve the strength of the shoulder and help your shoulder joint move smoothly.
Although the time needed for recovery goes, as a guideline, you may need Physical Therapy treatments for six to eight weeks. Most patients are capable to get back to their activities with full use of their arms within this amount of time.
Exercises:
Exercise includes Strengthening of shoulder muscle, stretching of muscle surrounding the shoulder, and stability exercises for the shoulder are the best place to start. With the help of exercises, there is an expansion in the subacromial space which takes the pressure and friction off the irritated tendons.
- ROM exercises: Shoulder joint movement
- Shoulder flexion
- shoulder extension
- Shoulder abduction
- Shoulder adduction
- Shoulder external and internal rotation
Begin exercise actively in the available range. Later on, followed by passive movement in full range slowly. For achieving full range, stretching exercises are necessary. As the full range is achieved, strengthening can be achieved.
2. Stretching exercises:
Pendulum exercises:
Cross arm stretch
- Relax both shoulders and slowly pull one arm across the chest as far as possible, holding at the upper arm.
- Hold the stretch position for 30 seconds and then relax for 30 seconds.
- Repeat with the other arm.

Passive Internal Rotation
Repetitions: 4 on each side
Days per week: 5 to 6 times
The patient may feel the stretch at the front of the shoulder
Equipment needed for exercise is a Light stick, such as a yardstick
Step-by-step directions:
- Hold a stick behind the back with one hand, and lightly grasp the other end with the other hand.
- Pull the stick horizontally as shown in the picture so that the shoulder is passively stretched to the point of feeling a pull without pain.
- Hold the position for 30 seconds and then relax for 30 seconds.
- Repeat on the other side.
Advice: Do not lean over or twist to the side while pulling the stick or doing exercise.
Passive External Rotation
Repetitions: 4 on each side
Days per week: 5 to 6 times
The patient should feel the stretch in the back of the shoulder
Equipment needed for exercise is a Light stick, such as a yardstick
Step-by-step directions:
- Grab the stick with one hand and cup the other end with the other hand.
- Keep the elbow of the shoulder that you are stretching against the side of the body and move the stick horizontally as shown to the point of feeling a pull without pain.
- Hold the position for 30 seconds and then relax for 30 seconds.
- Repeat the exercise on the other side.
3. Strengthening:
Strengthening exercises of the shoulder can be done with objects that provide resistance while doing exercises. Various weights, Dumbbells, Elastic bands, Theraband, and manual resistance can be done.
Strengthening of Rotator Cuff & Scapular for the Shoulder:
This is a home schedule designed to strengthen the muscles of the rotator cuff and scapula. Therabands are rubber bands that may be received from the physical therapist or purchased at a sporting goods store (e.g. Dick’s, Sports Authority, etc). Light-free weights such as 2-3 lb. dumbbells will be helpful, but if these are not readily known simple household items such as a can of soup may be used rather. Complete all exercises 3-4 times per week to keep the shoulder healthy and strong. Note: Each exercise should be completed for both shoulders.
Exercises:

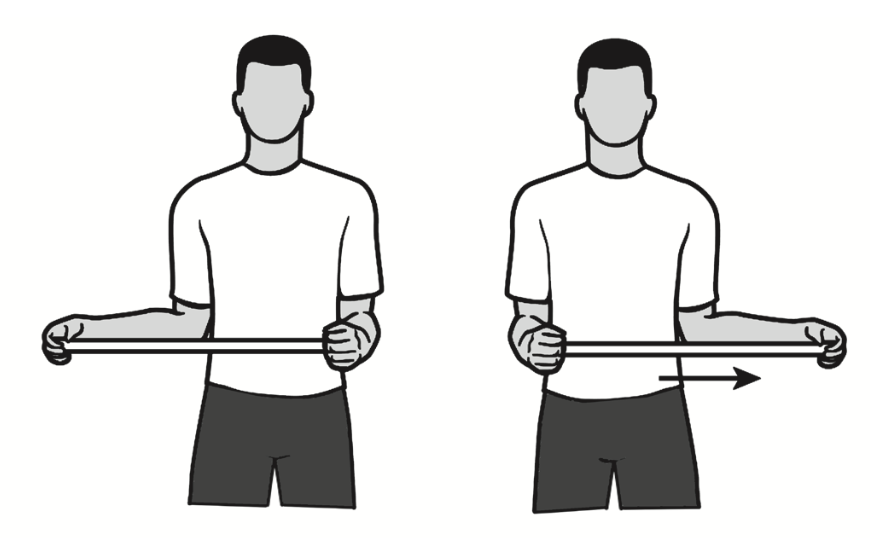
External Rotation
Attach the theraband at a core level to a doorknob. While standing sideways to the door and facing straight forward, grasp one end of the band and pull the band all the way through until it is tight. The elbow is placed next to the side with the hand as close to the chest as possible (think of this elbow as being a hinge on a gate). Take the cord in the hand ‘set’ the scapula and move the hand away from the body as far as it feels comfortable. Return to the start position. Perform 2 sets of 20 repetitions.
Internal Rotation
Connect the theraband at waist level in a doorknob. While standing sideways to the door and looking straight forward, grasp one end of the handle and pull the cord all the way through until it is tight. The elbow is placed next to the side and is relaxed at 90 degrees (think of this elbow as being a hinge on a gate). Taking the cord in the hand, ‘set’ the shoulder blade and move the hand toward the belly as far as it feels comfy, or to where the endpoint of pain limits it. Return to the start position. Perform 2 sets of 20 repetitions.
Lateral Raises
The person stands with the arm at the side with the elbow straight and the hands rotated so that the thumbs face forward. Raise the arm straight outside, palm down, until the hands reach shoulder level. Do not raise the hands more increased than the shoulder. Stay and slowly lower the arm. Perform 2 sets of 12 repetitions.
Standing forward flexion (‘full-can) exercise
Stand facing a mirror with the hands rotated so that the thumbs face in the forward direction. While keeping the shoulder blade ‘set’ and keeping the elbows straightforward, raise the arms forward and upward to shoulder level with a slight outward angle (30°). Stay for one second and slowly lower and repeat. Perform 2 sets of 12 repetitions.
Sidelying external rotation
Lying on your side, bend your elbow to a 90-degree angle and keep the arm firmly against the side with the hand resting on the abdomen. By rotation at the shoulder, raise the hand upward, toward the ceiling through a comfortable range of motion. Hold this position for 1 to 2 seconds, and then slowly bring the hand down. Perform 2 sets of 10 repetitions.
Prone rowing exercise
The starting position for this exercise is to lie face down on the bed with the arm hanging freely off of the side. While keeping the shoulder blade ‘set’, raise the arm up toward the direction of the ceiling while bending at the elbow. The elbow should be drawn along the body side until the hands feel the lower ribs. Always back slowly to the start position. Perform these 2 sets of 15 repetitions.

Prone horizontal abduction (‘T’s)
The starting position for this exercise is to lie face down on the bed with the arm hanging freely off of the side. Rotate the hand so that the thumb faces forward. While keeping the shoulder blade ‘set and keeping the elbows straightforward, slowly raise the arm away from the body to shoulder height, through a pain-free range of motion. Hold the position for 1 to 2 seconds and slowly bring it lower. Limit the height at which the person raises the arm horizontally to the floor. Perform 2 sets of 10 repetitions.
Prone scaption (‘Y’s)
The starting position for this exercise is to lie face down on the bed with the arms hanging freely off of the side. Keep the shoulder blade ‘set’ and keep the elbows straightforward. Slowly raise the arm away from the body and slightly forward through a pain-free range of motion (so that the hand now has the thumb facing up, and is aligned with the forehead). Hold the position for 1 to 2 seconds and slow down. Limit the height that the patient raises the arm to 90 degrees, or in other words, horizontally to the floor. Perform 2 sets of 10 repetitions.
Prone external rotation at 90º abduction (‘U’s)
Lie face down on a table or bed with the arm hanging over the side. Raise the arm to shoulder height 90º angle to the body. While holding the upper extremity in this position, rotate the hand in an upward direction, until the hand is even with the elbow. Hold the position for one second and slowly allow the hand to rotate to the starting position and repeat. Perform these exercises in 2 sets per 10 repetitions.
Press-ups
A person sits on a chair or table, placing both hands firmly on the sides of the chair, palm down and fingers pointed outside. Hands should be placed under the shoulders. Slowly push down through the hands to raise the body. Hold in these positions for 1-2 seconds and slowly lower the body back to the chair. Perform 2 sets of 10 repetitions
4. Improve Posture: Thinking about posture.
Surgical Treatment
Shoulder instability surgery may be recommended if a patient:
- Have recurrent shoulder dislocation
- Have a Shoulder Dislocation and are at more risk of it repeating again and again — For example if the person participates in a sport that raises the risk.
If nonsurgical treatments and physical therapy have not helped, surgery may be the next option to decrease the risk of recurrent dislocations and return a person to her daily activities.
There are several kinds of shoulder operations that stabilize the shoulder joint. The surgery may be done using an arthroscope or through an incision made in the skin depending on the type of injury a person has and the type of surgery needed. Shoulder arthroscopy is a minimally invasive surgical approach that allows the surgeon to evaluate the shoulder and in some cases treat the cause of instability. During the procedure, the surgeon will make small incisions in the shoulder called portals. A small camera is then placed in the portals and the internal space of the shoulder can be envisioned. The following are the more commonly performed surgeries.
Bankart Repair:- Also known as arthroscopic labral repair, this common procedure repairs tears to the glenoid labrum, which is the ring of cartilage around the edge of the shoulder socket. It restores the stability of the shoulders that don’t have any extensive damage from repeated dislocations in the shoulder. In small tears in the labrum, it is sometimes not required to repair the tear, but rather to débride it. A debridement is simply removing the frayed edges and any loose parts that get caught when the shoulder is moved. A more considerable tear is repaired using suture anchors and heavy suture to reattach the labrum to the socket. An open procedure may be required if the bone of the socket is involved in the injury. The surgeon would make the repair through a longer incision on the front side of the shoulder. And then incision would be closed with suture and sterile strips. Arthroscopic repairs can be executed at both the front side and back side of the shoulder depending on which direction the shoulder was dislocated. If there is an extensive injury to the front of the glenoid labrum or the bone of the socket joint or a person is at high risk for recurrence, the doctor may recommend an open Bankart repair.
Capsular shift:- This procedure is conducted to tighten the joint capsule. A capsular shift is normally performed using an arthroscope. In this procedure, the surgeon tightens the capsule, including the ligaments that stabilize the shoulder. This is equivalent to when a tailor tucks loose fabric by overlapping and sewing the two parts. By tightening the ligaments in the joint, they are then able to perform their stabilizing function.
Latarjet procedure:- This procedure is done when there is a loss of bone from the socket due to repeated dislocations in the joint. It is done by an open procedure. A small portion of bone is taken from another part of the shoulder and placed into the worn-away area of the shoulder socket. This is called a bone graft. It is attached using screws.
Remplissage Technique:-Sometimes, a dislocated shoulder can result in an indent in the ball part of the joint — which can cause the shoulder to dislocate again. This arthroscopic procedure fills in the dent in the back of the ball part of the humerus bone in the joint by advancing part of the attachment of the rotator cuff into that area, decreasing the risk of future dislocations. This may be connected with a Bankart repair.
Post-surgical Rehabilitation
Due to the number of factors that need to be considered when approaching post-traumatic anterior instability, clarity and consensus over the goals and cautions of the rehabilitation protocol are critically important.
PHASE I – IMMOBILIZATION
Goals:
The primary purpose of phase 1 includes protecting the healing capsulolabral tissue and decreasing post-operative pain and inflammation. Secondary objectives include protected glenohumeral (GH) joint range of motion (ROM) and strength, scapulothoracic stabilization, and addressing the kinetic chain. (i.e. adjacent joints, posture re-education).
Patients are alerted against doing any active or passive movement over the specified ROM, particularly external rotation, and patients are not allowed to carry any heavy object, push, pull, or use the affected arm beyond the ROM specified.
Specific Treatment Intervention:
Patients are immobilized in a sling and swath during the initial post-operative period, removing it for washing and exercises. Modalities such as Ice and Electrophysical agents such as IFT, SWD, TENS US, etc may be used for pain relief. Patient education on keeping to immobilization, managing pain, sleep, and rest positions are all important during this initial phase.
Protected GH joint ROM and scapulothoracic strength exercises can be completed with dosage dictated by pain and the ability to perform the exercise without any compensation. ROM is normally limited to 30 degrees of elevation (flexion and scaption) in neutral rotation and is performed in active-assist exercise. Strength exercises are conducted isometrically, with the shoulder in an adducted and slightly internally rotated placement. Scapulothoracic mobility and strength are highlighted during this phase along with the entire upper extremity kinetic chain. Cervical, thoracic, and lumbar spine mobility and stability are handled as indicated. Finally, patients are suggested to begin or continue cardiovascular exercise (e.g., stationary, recumbent cycling, or walking) that can be done with the shoulder supported in the sling.
Measures for Progression to Phase II:
The conclusion to progress a patient is made through consideration of time from surgery as well as fulfilling phase-specific criteria. In the Bankart repair procedure, progression to Phase II can occur when patients have indicated good adherence to shoulder immobilization with minimal pain at rest and correct scapular positioning with their arm at their side.
PHASE II – INITIAL MOBILIZATION AND STRENGTHENING
Goals:
Phase II aspires to increase GH joint ROM and improve shoulder girdle strength and control. Thinking of the healing capsulolabral tissue and pain is even more important. Secondary objectives include increased functional activities and integration of the kinetic chain.
Specific Treatment Intervention:
Immobilization is finished and ROM exercises progress from active-assisted to active when the patient is able to move through the range without pain and/or compensation. Isometric exercises may be moved to isotonic, avoiding long lever and abduction/external rotation positions. Scapular stabilization exercises improve to include both static and dynamic movements. All shoulder girdle strength exercises must be conducted with proper spine posture and a stable scapula and progress when the patient can maintain this position while performing the exercise. A mix of both open and closed-kinetic chain exercises should be utilized.
Measures for Progression:
Progression to Phase III occurs at about 12 weeks post-operatively, as long as the patient can be able to actively raise his/her shoulder to a minimum of 120 degrees of scaption with minimal pain and proper scapulohumeral rhythm. The patient should be able to perform the specified dosage of strength exercises, demonstrating proper technique and without reproducing pain and/or symptoms. Strength measures should be enhanced substantially at the end of Phase II. Finally, the patient should report an overall growth in the use of his/her affected arm in functional, daily activities.
PHASE III – STRENGTHENING AND RETURN TO ACTIVITY BACK
Goals:
The main objectives of the final phase are to enhance and normalize shoulder girdle neuromuscular strength, endurance, and proprioception as well as restore full, functional GH joint ROM and the entire upper extremity kinetic chain. Secondary objectives include returning to all daily activities, work, and recreation. Cautions remain regarding stretching the shoulder into abducted/externally-rotated positions and using the arm for lifting heavy objects, pushing, and pulling, especially in these same GH joint positions.
Specific Treatment Intervention:
Strengthening should contain all the shoulder girdle musculature, especially Scapular stabilizers, and Rotator cuff muscles. Progressions towards conducting strength exercises at increasing shoulder heights, in combined, functional movement patterns with dosage considerations that reflect both strength and endurance goals should occur. Both open and closed-chain exercises should be highlighted with progression features like speed, reaction time, and proprioception. ROM objectives should be achieved through joint mobility and soft tissue stretching as indicated. If stretching into external rotation, particularly overhead, is required, it must be done carefully to shield the surgically repaired tissue. Activity and patient-specific exercises are significant to address functional goals required for a full return to daily activities, work, and recreation.
Standards for Progression to RTA or Home Program:
Patients are regarded as appropriate for discharge if their shoulder girdle musculature’s strength and endurance are equal to or better than the unaffected side. A patient should show proper, symmetrical scapular control statically and dynamically through full, functional GH joint ROM. Patients should be committed to all activities of daily life and have returned to work. Most patients are able to return to their recreational and sport activity unless restricted by the surgeon.
Summary of post-rehab of surgery:
Immobilization:
- Sling for 3-4 weeks
- if required sling with flexion 20-degree flexion and 30-degree abduction
Restriction:
- External Rotation is limited to 45° until Day–45 OR No External Rotation + horizontal abduction x 3 wks
Mobility:
Start mobility exercises including:
- Pendulum exercise day 1
- Passive ROM from day 3rd
- Active assisted ROM in 3rd week, Be Carefully
- Active ROM by 6 weeks in all movement
- Stretching and mobilization in 6 weeks
Strengthening:
- Start by 6 weeks
- Sub-maximal Isometric shoulder in a week after surgery
- Isotonic External rotation, internal rotation after 6-9 weeks
- Diagonal movements
- Scapular exercises
- Rotator cuff muscle
- Adance strengthening at 12 weeks
Return to activity:
- Return to sports activity after 3-4 months. Overhead athlete
Outcome:
Shoulder instability is a condition in which the muscle in the shoulder joint is not stable and due to this, there may be a chance of subluxation. It is treated by medicine, surgery, and physiotherapy. Firstly it is treated conservatively, if not treated then surgical treatment is necessary. After surgical treatment, physiotherapy is required. Physiotherapy must be done very seriously to return back to activity. It takes a long time after surgery.
FAQs:
Why Shoulder Stability Is Important?
The muscles and tendons of the rotator cuff work concurrently to compress and stabilize the glenohumeral ball-and-socket joint of the shoulder. Lack of stability can lead to a laundry list of problems like shoulder pain with overhead activities
What muscles are used for shoulder stability?
The muscles of the shoulder play an integral role in providing stability to the shoulder joint. The primary muscle group that helps the shoulder joint is the rotator cuff muscles. The 4 rotator cuff muscles are the Supraspinatus, Infraspinatus, Teres minor, and Subscapularis.
Can you fix shoulder instability?
To correct painful instability, open surgery is often required. An incision is made over the shoulder and the muscles are pushed to gain access to the joint capsule, ligaments, and labrum
Is shoulder instability serious?
If it is left untreated, chronic shoulder instability can lead to more severe injury, shoulder joint pain, or arthritis of the shoulder joint.
How do I stop shoulder instability?
Rotator cuff and shoulder blade/scapular exercises are the best way to go for prevention and rehab. Push-ups and exercises that challenge the stability of the joint are effective in re-training the joint to try to minimize the risk of injury or re-injury.




One Comment