Hill Sachs Lesion
Table of Contents
What is a Hill Sachs Lesion?
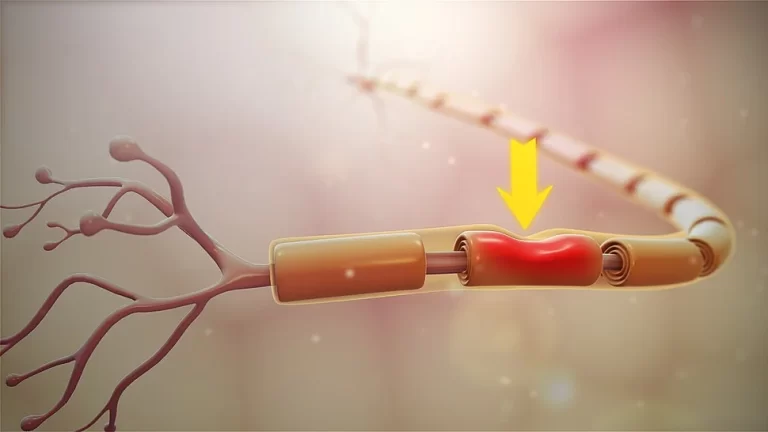
A Hill-Sachs lesion is a fracture or lesion in the long bone in the humerus (upper arm bone) that connects to the body at the shoulder. A doctor might have discovered this condition if a person has experienced a dislocated shoulder. In this case, the humerus bone slips out of the socket and is compressed against the glenoid rim. This makes a dent in the head of the humerus, causing debilitating pain and limited arm movement.
A Hill-Sachs lesion is an osseous defect or “dent” of the postero-lateral humeral head that occurs in association with anterior instability or dislocation of the glenohumeral joint. It is often connected with a Bankart lesion of the glenoid. This lesion is induced by an anterior shoulder dislocation which provokes a humeral head impression fracture. The posterolateral aspect of the humeral head impacts the anterior glenoid in the dislocated position, causing shoulder instability.
It results from violent impaction of the humeral head against the anteroinferior glenoid rim when the shoulder is dislocated anteriorly.
The depth of the lesion in the joint reflects the portion of damage to the opposite side of the joint—the anterior capsule and the labrum. Therefore larger Hill-Sachs lesions are associated with increased risks of recurrent dislocations.
If a person has dislocated shoulder and the humerus is pressed against the lip of its socket in the scapula (shoulder blade) the ball at the top of it can be damaged.
Most people recover from a dislocated shoulder that may cause a Hill-Sachs lesion in a month or two with a few months of physical therapy.
If a person has been diagnosed with a Hill-Sachs lesion or has pain in the shoulder that just won’t go away, a physiotherapist can help you. Our highly-skilled physicians comprehensively evaluate injuries and can develop the most effective approach to relieve the pain and get a person back on track. Our team of surgeons, nurses, and therapists offers both surgical and non-surgical options, including physical therapy to help heal and strengthen the shoulder.
Causes and Risk factors of Hill Sachs Lesion:
Dislocated shoulders lead to Hill-Sachs lesions.
The shoulder is a ball-and-socket joint. The humerus head is shaped like a ball that fits into the socket in the scapula. The shoulder joint is a very flexible joint. It can move in the multi directions and has many parts that can be injured.
The upper portion of the humerus bone is called the humeral head. It is larger than the socket that holds the humerus bone. To keep the head stable, tendons, muscles, and ligaments hold it in place.
If the shoulder is dislocated forward (away from the front of the body), the rounded head at the top of the humerus can get pressed into the edge of the socket it’s usually in. This pressure can damage the head of the humerus enough to dent the ball.
The Hill Sachs lesion is associated with anterior shoulder dislocation. When the humerus head is driven from the glenoid cavity, its relatively soft head impacts against the anterior edge of the glenoid. The result is a divot or flattening in the posterolateral aspect of the humeral head, usually opposite the coracoid process of the scapula. The mechanism which leads to shoulder dislocation is usually traumatic but can vary, especially if there is a history of previous shoulder dislocations. Sports falls, seizures, assaults, throwing, reaching, pulling on the arm, or turning over in bed may all be causes of anterior dislocation.
Common causes for a dislocated shoulder include:
- Falls, such as from a ladder or downstairs
- Sports activities, especially contact sports
- Trauma, such as a car accident
People with shoulder dislocations found that 58.8 percent of dislocations resulted from a fall. Of these cases, 47.7 percent occurred at home. And 34.5 percent of dislocations occurred while playing sports or participating in some other type of recreation. Overall, 48.3 percent of all dislocations occurred in sports or recreation.
Specific activity risks include:
- Contact sports include football, hockey, and soccer
- Sports where falls can be possible, such as skiing, volleyball, and gymnastics
- Sports with throwing activities, such as tennis and baseball
- Sports involving overhead motion, such as swimming and weight-lifting
- Occupations where a person does heavy lifting or pushing or pulling above shoulder height or does repetitive work
Approximately 47% of the lesions are associated with beginning shoulder instability according to research studies
Bankart lesion is 2.5 times more likely for someone with either of those lesions to have the other as well as Anterior glenoid bone loss (in cases of recurrent instability).
A dislocated shoulder has a higher risk of recurrence after the first injury. Studies showed that if a person has a Hill-Sachs lesion, then it is 1.55 times more likely to have a recurrence.
Classification of Hill Sachs Lesion:
Classification systems are used to interpret the quantity of destruction to the anterior capsule and the labrum, reflected by the depth of the lesion. Higher-grade lesions are associated with a higher risk of recurrent dislocation.
Grade 1: Defect in the articular surface down to the subchondral bone
Grade 2: Lesion contains the subchondral bone
Grade 3: Lesion leads to a large defect in the subchondral bone.
Further classification can be done by knowing the percentage of the defect of humeral head involvement in the compression fracture. The size of the lesion is associated in most cases with the number of previous dislocations.
- Minor: <20%
- Moderate: 20%-45%
- Severe: >45%
Another classification depends on: ON track or OFF track
- If the Hill-Sachs lesion engages, it is termed as an “off-track”
- If the Hill-Sachs lesion does not engage, it is termed an “on-track” lesion.
Signs and symptoms of Hill Sachs Lesion:
Shoulder dislocation infrequently occurs isolated. It leads to the devastation of other tissues surrounding the glenohumeral joint, such as Ligaments, Rotator cuff tendons, Joint capsule as well as the bone and cartilage of the humeral head. This happens when the round humeral head is forcibly deep-seated on the edge of the glenoid, which causes compression fractures in the humeral head. This makes a dimple structure on the articular surface of the humerus which is known as a Hill-Sachs lesion. This is always acquired by dislocation, not only subluxation.
The following indicates an acute Anterior Glenohumeral Dislocation:
- Arm is placed in the abduction and external rotation
- Absence of normal shape of the deltoid and acromion prominent posteriorly and laterally
- Humeral head palpable anteriorly
- All movements are limited and painful also
- Coracoid process: Palpable fullness at the process and positioned towards the axilla
Hill-Sachs lesions usually have the exact symptoms as the dislocated shoulder that causes them, including:
- Severe pain.
- Weakness in limb
- Inability to move the arm.
- The shoulder is visibly out of place.
- Swelling may present
- Bruising or discoloration in the skin
- Muscle spasms present
- Numbness, tingling, or weakness in the arm, hand, or fingers.
If a person has a Hill-Sachs lesion, they might experience more severe versions of these symptoms.
The most common sign of the Hill-Sachs lesion is severe pain in the shoulder, especially during movement. Other symptoms a person may observe include:
- Nausea, lightheadedness, and weakness
- Recurring shoulder dislocations
- Squared off the appearance of the shoulder, sometimes the presence of a bulge in the front of the joint.
Diagnosis:
Physical examination:
- Bony apprehension test:
Positive test: Pain/reflex muscle contraction (in case of subluxation) may present - Jobe relocation test:
Positive test: Apprehension
Crepitus and catching may be sensed during active and passive abduction and external rotation
Possible lesion indicated by audible/palpable clunk in active/passive abduction and external rotation or an unstable feeling during mid-range
Special investigations:
X-ray:
Grashey view (AP) in internal and external rotation; transcapular view (X-ray beam caudally from standard AP view); axillary views with exaggerated external rotation and West Pont views (if pain allows) can be done.
The essential first step at effectively evaluate the glenohumeral relationship as well as the osseous pathology of the humerus and the glenoid.
A doctor can detect bony lesions related to shoulder instability in the acute phase
It is difficult to see Hill-Sachs lesions in X-ray
Ultrasound:
Ultrasound detects and localizes a compression fracture
Cost-effective, minimal exposure to extreme radiation, comfortable for the patient
Hill-Sachs lesions: Apparent triangular depression in the shape of the humerus
CT scan: CT scan reliably assesses the location and depth of the humeral lesion
MRI: MRI detects pathology of the soft tissue; determines the amount of humeral and glenoid bone loss.
Treatment of Hill Sachs Lesion:
There are many methods for treating a dislocated shoulder. Some may be done in the doctor’s office by giving a local anesthetic. Other treatments may require either open surgery or arthroscopic surgery. If the dislocation also involves damage to the humerus bone or surrounding area, the doctor may include additional treatment.
Treatment for a Hill-Sachs lesion relies on the size of the lesion, its placement, the involvement of the glenoid socket bone, and how it affects arm mobility. If the lesion is little, involving less than 20 percent of the head of the humerus, it’s likely that the doctor will leave it alone and suggest physical therapy to strengthen the shoulder.
If the lesion is medium-sized, involving 20 to 40 percent of the head of the humerus, the treatment option will rely on whether the doctor determines the shoulder will be unstable if it is not treated.
Medical Treatment
The bony defect usually does not need treatment, though the connected glenohumeral instability and possible anterior labral injuries often require surgical repair.
- Minimum glenoid bone loss and without any considerable involvement of the humeral head (<20%), surgical management is not indicated as treatment. This instability can be operated conservatively in a master sling for immobilization for 2-6 weeks, before starting with rehabilitation.
- Large Defects: Management of the bony defect (as in Hill-Sachs lesion) can be treated with bone grafting or placement of soft tissue within the defect
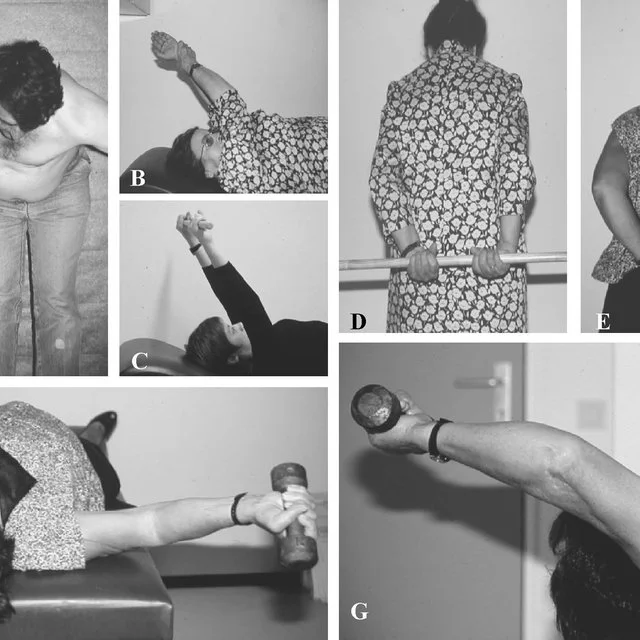
Physiotherapy Treatment:
The aim of physical therapy is to prevent the reoccurrence of dislocations.
The non-operative rehabilitation of the unstable shoulder consists of about seven key factors. It is important to consider this in the rehabilitation program for the shoulder after a Hill-Sachs lesion.
- The onset of pathology
- The degree of instability
- The frequency of dislocation
- The direction of instability
- Concomitant pathologies
- Neuromuscular control
- Activity level
Physiotherapy interventions include:
2-6 weeks of immobilization in a mastering:
- Scapula stabilization exercises
- Hand, wrist, and elbow exercises
- Teach the patient about functional adaptions (e.g. personal hygiene, dressing, and undressing)
- No driving while still in a sling
When the use of a sling is discontinued (on the recommendation of the orthopedic surgeon):
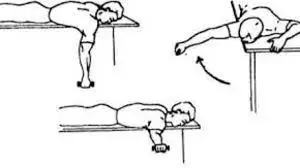
- Pendulum exercises
- Passive, active-assisted, and active range of motion exercises (progressions)
- Abduction and external rotation is restricted during the initial phase of the rehabilitation
- Ligaments healing needs to take place to prevent dislocation
- Strengthening of the deltoid, rotator cuff, and periscapular (e.g. pectoralis major) muscles
Post-surgical rehabilitation should be guided by the orthopedic surgeon and depends on the procedure that was done.
Surgical Treatment:
In orthopedic hospitals, doctors offer a full range of innovative and traditional surgical techniques to treat Hills-Sachs lesions. These may include:
- Capsular Shift: In these, it shifts the shoulder capsule to tighten tissue and avoid exaggerated shoulder rotation.
- Bone Grafting/Tissue Filling: A doctor uses either bone (often from the pelvis) or soft tissue to fill the defects in the humeral head.
- Bone augmentation: This can be directly done on the humerus head, or onto the glenoid bone in order to stop its contact with the humerus when you move the shoulder.
- Disimpaction: A doctor lifts the compressed bone to restore the shape of the humeral head. This concerns bone graft under the lesion to lift the humerus up to the pre-injury position. It’s a fairly new procedure best suited for lesions that are less than three weeks old and have under 40 percent of humerus bone involvement.
- Remplissage: This is an arthroscopic technique in which the rotator cuff and capsule are sewn into the bony defect to reduce the risk of recurrent dislocation. This technique surgically adds tissue to the injured area. The procedure is usually done on Hill-Sachs lesions that are medium in size and also have some amount of glenoid defect.
- Shoulder Replacement: This surgery is reserved as the last resort and is typically used for large defects in older patients.
- Resurfacing: Resurfacing can be done with a metal implant or a complete replacement of the humeral head. The complete replacement is named a hemiarthroplasty. It’s done on people who have recurrent problems and contain involvement of more than 40 percent of the humerus bone. It is not recommended for younger people.
Open technique
- Laterjet procedure: This procedure is most frequently done.
Most commonly, a bone from the coracoid process is used as an augment to the anteroinferior glenoid bone loss. By reforming the concavity and width of the glenoid, a Hill-Sachs lesion does not influence the anterior glenoid rim of unstable shoulders.
Successful in preventing instability over time
Negative consequences associated with the Laterjet are shoulder arthrosis and loss of function in the shoulder
- Autologous bone plugs: Size-matched osteoarticular allografts
- Rotational humeral osteotomy:
Osteotomy of the surgical neck to rotate the humeral head for 25°
Currently, it is not the method of choice, given the related risks and the success rates of more recent procedures.
The osseous humeral allograft bone plug technique:
A size-matched humeral bone plug of a donor is used to treat
Approach: Delto-pectoral or deltoid-splitting
Advantages: Minimal exposure; humeral head remains in the capsule.
Disadvantage: Limited to small and moderate lesions; risks of using cadaveric tissue
How to Prevent Hill Sachs Lesion?
Because accidents such as falls or sports injuries commonly cause dislocated shoulders, there is not usually anything a person can do to prevent a Hill-Sachs lesion.
Follow these general safety tips to decrease the risk of an injury:
- Always wear a seatbelt.
- Wear the right protective equipment while doing activities or playing sports.
- Make sure the home and workspace are free from the chaos that could interrupt or may increase the falls
- Always use the proper tools or equipment at home to reach things overhead. Never stand on chairs, tables, or countertops in absence of any person or helper.
- Use a cane or walker if having difficulty in walking or have a higher risk of falls.
Conclusion:
A Hill-Sachs lesion is an injury that emerges secondary to an anterior shoulder dislocation. The humeral head ‘collides’ with the anterior part of the glenoid, generating a lesion, bone loss, defect, and deformity of the humeral head. This may induce a change in the loss of range of motion, feelings of instability, and pain. A grading system is used depending on the amount of bone loss or severity of the humeral head deformity. The incidence of Hill-Sachs lesions in patients with anterior shoulder instability can be as high as 100%. Another pathology secondary to an anterior shoulder dislocation is a Bankart lesion. This is an injury of the anterior glenoid labrum of the shoulder and is often accompanied by a Hill-Sachs lesion.
Conservative treatment is only recommended in cases of small bony defects (<20% Hill-Sachs lesion), in other cases (larger and more significant lesions), surgical treatment is needed. The conservative treatment should be based on strengthening the deltoid, the rotator cuff muscles, and scapular stabilizers.
FAQs:
What Causes a Hill-Sachs Lesion?
Hill-Sachs lesion is most often induced by a shoulder dislocation. The shoulder consists of a ball-and-socket joint. When the humerus ball slips out of the socket, it pushes against the socket’s rim, leaving an indentation in the humeral head.
Does Hill-Sachs need surgery?
For smaller-sized Hills-Sachs lesions, in which there is less than 20% of the humeral head has been affected, physical therapy or careful observation may be an efficacious option. For more severe cases and larger lesions, surgery is likely the best option for healing.
What is the treatment for Hill-Sachs lesion?
There are numerous techniques that can be used in combination with a Bankart repair or as a primary technique that includes fixing or filling in the bony defect using remplissage, reduction of the lesion, humeral head allograft, partial or full humeral head resurfacing, or rotational osteotomy.
Is a Hill-Sachs lesion a fracture?
A Hill-Sachs lesion, or Hill-Sachs impaction fracture, is an injury to the back part of the rounded top of the upper arm bone (humerus). This injury occurs when there is a dislocation in the shoulder.
Is a Hill-Sachs lesion bad?
A Hill-Sachs lesion is an injury that arises secondary to an anterior shoulder dislocation. The humeral head ‘hits’ with the anterior part of the glenoid, causing a lesion, bone loss, defect, and deformity of the humeral head. This may induce a change in the loss of range of motion, feelings of instability, and pain.