Non-union Bone Fracture
Table of Contents
What is a Non-union?
A non-union fracture is a type of fracture that does not heal or fails to heal within a normal timeframe. In most cases, fractures will heal within six to eight weeks if the bone is immobilized properly and receives proper nutrition. However, if the fractured ends of the bone fail to unite, the result is a non-union fracture.
Non-union fractures can be caused by a variety of factors, including poor blood supply to the bone, infection, instability at the fracture site, and inadequate immobilization of the affected limb. Treatment options for non-union fractures may include surgery, such as bone grafting or the use of specialized implants to stabilize the bone, as well as physical therapy and other supportive measures to promote healing.
With modern treatment methods, most broken bones (fractures) recover without any problems. After a broken bone is treated, new bone tissue starts to form and joins the broken pieces.
Some broken bones do not recover even when they get the best surgical or nonsurgical treatment. Certain risk factors can sometimes increase the likelihood that a bone won’t heal. A “nonunion” is a damaged bone that doesn’t heal properly. A “delayed union” happens when a fracture heals more slowly than expected.
Nonunion is a chronic failure of the bone to heal after a fracture unless treatment (such as surgery) is performed. The terms “false joint” and “pseudoarthrosis” (from the Greek pseudo-, meaning false, and arthrosis, meaning joint) are frequently used to describe fractures that do not heal because they frequently take on the structural characteristics of a fibrous joint. The diagnosis is typically made when there is no healing between two sets of medical imaging, such as an X-ray or CT scan. This is generally after 6–8 months.
Nonunion, a significant challenge with fractures, can happen when the fracture moves excessively, has an insufficient blood supply, or develops an infection. Smokers are more likely to suffer from nonunion. The usual process of bone repair is halted or slowed down.
A nonunion may, in extremely rare circumstances, continue to heal without treatment since the bone-healing process is quite unstable. Normally speaking, if a nonunion is still present six months after the damage, it won’t heal without certain care, usually orthopedic surgery. A delayed union is a non-union that eventually heals.
Healing of the bone often takes a few months after a bone breaks or fractures (both terms signify the same thing). A bone is considered healed or “united” when it is strong and adequate to allow normal activities. Depending on many factors, this can take as short as 4 weeks or as long as 6 months. When a fractured bone is not healed and there is a possibility it will heal without surgery, the fracture is then counted to be a “nonunion”. A “Delayed Union” is not the same as a nonunion. A delayed union suggests that the bone’s healing took longer than anticipated or is still proceeding longer than anticipated, but that the bone will eventually mend without the need for extra surgery.
How do Bones heal?
When a bone cracks, the body instantly goes to work trying to heal it. Fractures healing process occurs in three stages:
- Inflammatory phase
- Repair phase
- Remodeling phase
Inflammatory stage: Blood and immune system cells rush to the location during the inflammatory stage to begin the healing process. Immune cells eliminate tainted blood, broken bones, and other damage indicators. The area around the broken bone is filled with blood, fluid, and immune cells, which results in inflammation. This phase, which peaks a few days after the accident and can extend for weeks, is what causes the majority of the discomfort and swelling following a fractured bone.
Repair stage: The repair stage overlaps with the inflammatory stage. In order to stabilize the broken ends of bones, the body creates a callus from the immature bone. This callus lacks calcium at first and is initially soft and stretchy. This explains why an X-ray doesn’t detect the initial phases of fracture healing.
Remodeling stage: Eventually, the body started the remodeling stage. That’s when calcium starts to enter the callus, and the callus evolves into more mature bone tissue. When the fracture has entirely healed, this remodeling stage, which can last months, may make the fracture virtually unnoticeable.
Bone Repair
The bone must have sufficient stability and blood flow for bone repair to occur. Bone repair is aided by a nutritious diet.
Stability: All methods of treating shattered bones adhere to the same fundamental principle: the fragments must be repositioned and restrained from shifting while they are healing. Some fractures can be stabilized by a cast. Surgical fixing of some fractures is necessary using tools including screws, plates, rods, and frames.
Blood flow: The elements necessary for healing are carried to the fracture site by blood. These include the body’s own chemicals required for healing (growth factors), oxygen, and healing cells. During the healing process, the blood flow to the broken bone normally returns on its own. A broken bone was fixed with a plate and screws.
Nutrition: A broken bone also requires adequate nutrition to heal. Eating a healthy and well-balanced diet that contains protein, calcium, vitamin C, and vitamin D is the best way to provide adequate nutrition; dietary supplements that go above the daily requirements are not effective. (The rare exception is the hardly malnourished patient with many injured organs. In this case, the doctor will discuss dietary guidelines and make suggestions for adding dietary supplements.)
Types of nonunions:
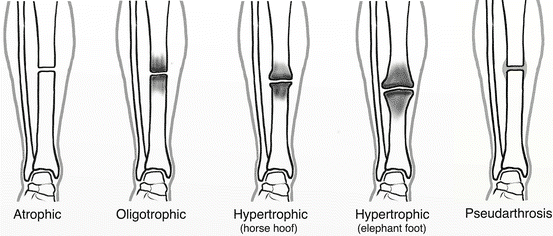
- Hypervascular or hypertrophic: (horse hoof)
- Resulting from insufficient stability with a sufficient blood supply and biology
- Demonstrated by radiographically extensive callus development
- Importantly, the ends are not joined, and there is no bridging bone.
- This research suggests that biology and blood supply are enough (as evidenced by the development of calluses), but stability is insufficient.
- Septic nonunion:
- It is caused by an infection.
- The CRP test is the most accurate predictor of infection.
- reduces blood flow from organisms consuming nutrition to healthy bones
- Increases the new bone formation.
- Oligotrophic non-unions:
- These are not hypertrophic types, and callus is absent.
- Produced by fracture fragment displacement and insufficient reduction
- They typically occur after major displacement of fractures, the distraction of fragments, or internal fixation w/o accurate
- Apposition of fragments;
- Has an intact blood supply.
- Demonstrates radiotracer uptake on radionuclide scans
- Has an inadequate healing response
- Avascular or atrophic:
- Caused by the insufficient blood supply and immobilization
- The fragments’ ends become atrophic and osteoporotic;
- The non-union is inert and incapable of biological reaction;
- Will undergo a cold bone scan.
- The ends of the fragments have a weak blood supply;
- These are commonly seen in tibial fractures treated with a plate and screws;
- Typically, the final result is the absence of intermediate fragments and the presence of scar tissue devoid of osteogenic potential;
- The bone ends that are eburnated, osteopenic, or sclerotic may be visible on radiographs.
- Treatment: Open decortication and the addition of cancellous bone grafts are necessary;
- Comminuted Nonunions:
- These can be identified by the presence of one or more necrotic intermediate fragments;
- Typically, any plates used to stabilize the acute fracture break as a result of these nonunions;
- Defective non-unions:
- These are distinguished by the loss of a piece of a bone’s diaphysis;
- The fragments’ ends are viable, but they cannot be united across the defect;
- The ends of the pieces become atrophic as time goes on;
- These non-unions develop following open fractures, sequestration in osteomyelitis, and tumor removal;
- Infected tibial nonunion:
Causes of Non-union:
There are several other causes why a fracture may not heal correctly. A surgeon requires to consider these, as fixing this will be vital in choosing the proper treatment. Causes for non-healing or nonunion fracture contain:
- Infection at the site of the fracture
- Inadequate blood supply to the fractured bone
- Separation of the bone ends during or following surgery
- Inadequate surgical stabilization of the bone
- Avascular necrosis (the fracture cut off the blood supply)
- There is no opposition between the two ends, i.e., they are not next to one another.
- Infection (particularly osteomyelitis)
- The fracture is not stable(that is, the two ends of the bone are still mobile)
- Soft-tissue imposition (covering the shattered ends with muscle or ligament to keep them from contacting one another)
Multifactorial causes are there:
- Most commonly, insufficient fracture stabilization and inadequate blood supply lead to nonunion
- Infection
- Eradication must occur along with the achieving fracture union
- Smoking
- Location:
- Due to the blood flow in these regions being low, the scapholunate, distal tibia, and base of the fifth metatarsal are more susceptible to nonunion.
- Pattern
- Seen in Segmental fractures and those with butterfly fragments
- Due to the intercalary segment’s compromised blood supply, there is an increased likelihood of nonunion.
Risk factors:
Related to the person:
- Age: Most Common in old age
- Nutritional status: Poor
- Habits: Nicotine and alcohol consumption
- Metabolic disturbance: Hyperparathyroidism
- Can be found in those with NF1
- Genetic predisposition
Related to the fracture site:
- Soft tissue interposition
- Bone loss at the fracture
- Infection
- Loss of blood supply
- Damage to surrounding muscles
Related to treatment:
- Inadequate reduction
- Insufficient immobilization
- Improperly applied fixation devices.
Several other factors increase the risk of nonunion.
- Smoking, chewing tobacco, using nicotine patches, or using nicotine gum all slow down bone healing and increase the likelihood of a nonunion.
- Seen in Older age
- Severe anemia
- Diabetes
- Due to low vitamin D level
- Hypothyroidism
- Poor nutrition
- Medications, such as aspirin, ibuprofen, and prednisone, as well as anti-inflammatory drugs. The dangers and advantages of utilizing these drugs during fracture healing should always be discussed between the doctor and the patient.
- Infection
- An open or complex break that is difficult.
The risk factors in detail:
- Smoking, vaping, and nicotine-containing products: Nicotine usage of any kind slows the healing process and increases the likelihood of nonunion fractures.
- Energy-intensive injuries: Compared to other traumatic events, high-energy fracture-causing injuries—car accidents are the most frequent, although falls from a height would also qualify—are more likely to result in nonunion fractures because they are more likely to cause damage to blood vessels and surrounding tissue and alter blood flow.
- Open Fractures: Due to the disruption of the blood supply, open fractures—those in which at least one end of the broken bone pierces the skin—might be more prone to result in nonunions.
- Lower Vitamin D Level: Vitamin D is vital for the development of bones. It gives calcium absorption a vital boost. Less vitamin D reduces calcium absorption from food or supplements, which may obstruct the formation of calluses and bones (osteogenesis).
- Diabetes: Type 2 diabetes has a variety of effects on how bones recover. People with diabetes make fewer bone cells, develop new blood vessels in the bone more slowly, and experience higher amounts of harmful inflammation.
- Osteoporosis: Throughout the course of a person’s life, bone tissue is continuously renewed. Osteoporosis occurs when bone tissue is lost more quickly than it can regenerate. Osteoporosis raises the risk of fractures and also increases the likelihood of nonunions following a fracture.
- Infection: If an infection develops at the site of a fracture, the body may divert its energies away from healing the fracture to combat the infection, which could lead to nonunion or a delayed union.
Symptoms of Non-union:
A history of a broken bone is usually clear. Long after the acute pain from the fracture goes away, patients with nonunions typically continue to have discomfort at the site of the break. This pain may stay for months or even years. It may be constant, or it may appear only when the broken arm or leg is used
There is a whole list of symptoms that patients with non-union fractures will typically present with. The main ones include:
- Swelling
- Persistent Pain
- The patient may notice an Abnormal clicking sound at the fracture site
- Tenderness
- Joint Instability
- Limb or joint Deformity
- Difficulty in bearing weight
- Bone tenderness
- Bone instability
- Limb deformity
- Joint deformity
- Stiffness in the affected area
- Immobility
- Restricted use of the affected area
- Unable to fully flex the affected joint
Diagnosis:
Doctor Examination:
The doctor uses imaging studies, which give clear images of the bone and surrounding soft tissues, to identify a nonunion. Relying on which bone is involved, these tests may contain X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI). Imaging tests enable the clinician to visualize the damaged bone and monitor the healing process.
A nonunion may be analyzed if the doctor finds one or more of the following:
- Persistent pain at the fracture site
- A persistent gap that is not spanned by bone at the fracture site
- When compared over several months, repeated imaging examinations show no progress in bone repair.
- Insufficient healing in a time period that is usually enough for normal healing
- If the doctor diagnoses a nonunion, they may advise blood tests to investigate the cause. These tests could identify an infection or another illness that could hinder bone regeneration, such as diabetes or anemia.
Physical exam:
- Complete a thorough neurovascular examination that considers the soft tissue envelope, among other things.
- Evaluate the mobility of the nonunion
- Evaluate extremities for the presence of deformity
IMAGING
- Radiographs:
Four views should be included on plain radiographs, which are the cornerstone for evaluating fracture healing.
Full-length weight-bearing films should be acquired if a limb length discrepancy is present
- Consider 45 deg oblique views and stress views for the maximal diagnostic prospect
- Bridging trabeculae, or the absence of bone crossing the fracture location
- Sclerotic fracture edges
- Persistent fracture lines (On the AP and Lateral views, the real union can be seen as 4 healed cortices)
- Lack of proof of progressive change toward union on serial x-ray.
- Failing or broken implants
- Progressive deformity
- Lack of callus (most unreliable finding)
- Callus formation is desired in IM nail
- Callus formation is not desired with plate fixation;
2. CT scan
- A CT scan should be accepted; hardware artifacts may restrict the utility of the CT scan.
Treatment:
Nonoperative method:
- Fracture brace immobilization
- Bone stimulators
- Bone stimulation
Bone stimulation with either electromagnetic or ultrasound waves has been recommended to decrease the healing time for non-union fractures. The suggested mechanism of action is by stimulating osteoblasts and other proteins that form bones using these modalities. The proof supporting the use of ultrasound and shockwave therapy for improving unions is very weak and it is possible that these approaches do not make a clinically significant difference for a delayed union or non-union.
- Bone stimulation
Contraindications:
-Synovial pseudoarthroses
-Mobile nonunions
-Greater than 1 cm between fracture ends
Operative methods in several types:
Infected nonunion
- Often associated with pseudoarthrosis
- The chance of fracture healing is less if the infection is not eradicated
- The staged approach is often essential
- Modalities
- Need to remove all infected/devitalized soft tissue
- Use antibiotic beads, and VAC dressings to control the wound
- With significant bone loss, bone transport may be another option
- Muscle flaps can be essential for wound management with soft tissue loss
Pseudoarthrosis
- It may be found in association with infection
- Modalities
- Removal of atrophic, non-viable bone ends
- Internal fixation with mechanical stability
- Maintenance of viable soft tissue envelope
Hypertrophic nonunions
- Often have biologically viable bone ends
- The issue with fixation, not the biology
- Modalities
- Internal fixation with the application of appropriate mechanical stability
Oligotrophic nonunions
- Often have biologically viable bone ends
- May need biological stimulation
- Modalities
- Internal fixation
Atrophic nonunions
- Often have dysvascular bone ends
- Modalities
- Require to confirm biologically viable bony ends are apposed Fixation needs to be mechanically stable
- Bone grafting
- Autologous iliac crest (osteoinductive) is the gold standard
- BMPs
- Osteoconductive agents (ie. crushed cancellous chips, DBM)
- Establishment of healthy soft tissue flap/envelope
Orthopedic surgeries:
Currently, there are different strategies to augment the bone-regeneration process, however, there is no standardized clinical treatment approach yet. Surgical treatment options contain:
- Debridement: Radical surgical removal of necrotic or infected soft tissue and bone tissue is considered essential for the healing process.
- Immobilization of the fracture with internal or external fixation: Metal plates, pins, screws, and rods, that are fixed or driven into a bone, are operated to stabilize the broken bone segments.
- Bone grafting: Filling of the bone defect resulting from debridement must be achieved. Autologous bone graft is the “gold standard” method and possesses osteogenic, osteoinductive, and osteoconductive properties, although only a limited sample can be accepted and there is an increased risk of side effects.
- Bone graft substitutes: Inorganic bone replacements can be used to supplement or take the place of autologous bone grafting. The benefit is that there is no morbidity associated with sampling and that the availability of them is not restricted. S53P4 bioactive glass has shown good outcomes as a promising bone graft replacement in the treatment of nonunions, due to its osteostimulative, osteoconductive, and antimicrobial properties.
In simple cases, healing may be noticeable within 3 months. Signs of a union typically appear after 3 months, but the course of treatment may extend well beyond that.
- For Managing infection in the setting of nonunion:
- Intraoperative culture is the gold standard for the diagnosis of infection
- Treated with culture-specific antibiotics.
When the diagnosis of infection is confirmed before treatment in the setting of nonunion, a staged treatment method is suggested. Debridement, removal of any loose or persistently infected hardware, revision fixation, stabilization of the nonunion, and the management of infection with culture-specific local and systemic antibiotics should all be included in the initial step.
Local antibiotic treatment can be achieved by a variety of methods including antibiotic nails, antibiotic cement beads, bioresorbable antibiotic pellets, or antibiotic cement spacers. In addition to aiding in the eradication of infection, antibiotic cement spacers (Masquelet technique) can encourage the creation of an osteogenic-induced membrane. There are also a number of options for revision fixation including both temporary (external fixation and antibiotic nails) and definitive (intramedullary nails and plates) forms of fixation. At this time, soft tissue coverage may also be necessary in the form of a flap or rotational coverage.
The second stage often moves forward when there are no longer any clinical or serological indicators of infection and after a period of systemic antibiotic therapy.
This reconstructive stage to address the nonunion may consist of definitive fixation, bone grafting, other biologic treatment, or bone transport, depending on the specific characteristics of the nonunion
- Bone grafting:
Autologous bone grafting is the cornerstone of surgical treatment for nonunions with compromised biology (atrophic nonunion). Three points are essential for successful grafting: osteogenesis, osteoinduction, and osteoconduction. Osteogenesis is described as a cell’s ability to differentiate into bone matrix-producing osteoblasts. Osteoinduction is defined as the ability of a growth factor to induce osteogenic differentiation of skeletal progenitor cells or induce osteoid deposition by osteoblasts. Osteoconduction describes the ability of a material to supply a scaffold for the attachment and subsequent bone matrix deposition of bone-forming cells.
All three are essential for successful healing in nonunion.
The 2 most ordinary options for autograft harvest enclose iliac crest bone graft (ICBG) and the Reamer-Irrigator-Aspirator (RIA).
Other treatments for nonunion:
1. Biological therapies
2. Cell-based therapy
Physical Therapy Treatment:
Fractures often heal well, but they can also come with treatable difficulties such as joint stiffness, muscle weakness, issues with tendons, and damage to your nerves.
Treatment of the injured soft tissues must frequently take precedence over the fracture itself for physiotherapy to be effective. Unfortunately, the clinicians whose main priority is to manage your fracture may ignore these.
A thorough assessment by a musculoskeletal physiotherapist can spot and address a variety of issues, assisting in the quickest possible return to the normal range of motion, strength, and function.
Physiotherapists also use effective evidence-based modalities such as shockwave therapy and regenerative therapy which stimulate the body’s own healing mechanism to heal tendon problems.
The course of treatment may include a combination of the following, depending on the problems you uncovered during your initial assessment:
- Soft tissue manual therapy, particularly to manage edema, swelling, and trigger points
- Scar management if they had surgery to fix the fracture
- Stretching exercises to regain joint range of movement, and optimize muscle length and tone
- Manual therapy and mobilizations to the joints to assist you in regaining good movement at the joints around the break
- Structured and progressive strengthening regime
- Work on balance and control, as well as, where necessary, gait (walking) re-education
- Getting back to athletic preparation work and guidance as needed.
- A modern, well-stocked gym is available to our team members. With the use of this equipment, the staff can rehab you more quickly, but more importantly, effectively, minimizing any downtime.
We also offer an aquatic treatment pool for people who need to remain weightless for a while. This means you can continue exercising to increase muscle strength, balance, flexibility, and the cardiovascular system even in the presence of any weight-bearing restrictions.
Summary:
Non-union fracture has differed from the delayed union. It has symptoms such as pain, swelling, stiffness, tenderness, etc. Some people may have deformities. It is diagnosed by X-ray, CT scan-like imaging. Treatment may include medical and home treatment to decrease pain. But the permanent solution is Surgical treatment only. There are various surgeries that can treat nonunion fractures. After performing surgery, physical therapy is essential for getting recovery, so a person can get back to their work back.
FAQs:
What is the treatment for non-union?
Nonunion treatments are few but include:
Surgery to treat an infection or repair the bone.
Immobilization by casting or splinting.
Bone graft (using a cadaver bone or a piece of your own bone)What is an example of a non-union fracture?
Foot & Ankle Fractures Nonunion. Every fracture carries the chance of not healing properly and producing a nonunion. Nonunions can occur in any bone, however, they occur most frequently occurs in the tibia, humerus, talus, and fifth metatarsal bones.
Is a nonunion serious?
Nonunions usually lead to a continuance of the pain at the site of a break, even after the initial pain of the fracture has passed. The pain from a nonunion may last months or even years if treatment is not desired.
How long might it take for a nonunion to heal?
This could take as little as 4 weeks or as much as 6 months, depending on a number of variables.
Who is most at risk for nonunionization?
Numerous illnesses, such as osteoarthritis, rheumatoid arthritis, osteoporosis, and diabetes, are linked to a higher incidence of nonunion.







7 Comments