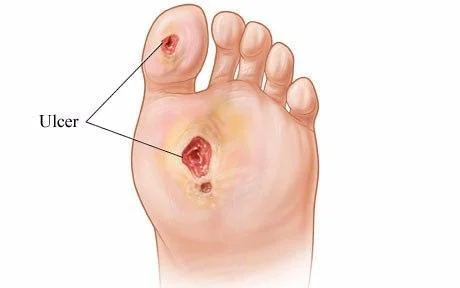
Diabetic Foot Ulcer
Table of Contents
What Is a Diabetic Foot Ulcer?
- A Diabetic foot ulcer is an open sore or wound that often develops on the bottom of the foot and affects 15% of people with diabetes. Six percent of people who get a foot ulcer end up in the hospital because of an infection or other ulcer-related issues.
- One of the most prevalent consequences for those with poorly managed diabetes mellitus is diabetic foot ulcers. Poor foot care, peripheral vascular disease, underlying neuropathy, and poor glycemic management are the typical causes. It is also one of the common causes of foot osteomyelitis and lower extremity amputation. These ulcers generally develop in areas of the foot that are constantly under pressure. Staphylococcus is a widespread infectious agent. It is very helpful when primary care doctors, vascular surgeons, endocrinologists, infectious disease experts, and podiatrists all work together. It is a circumstance that is frequently seen in both inpatient and outpatient settings.
- Compared to other diabetes complications, diabetic foot ulcers cause the most hospitalizations. Diabetes is presently the major cause of non-traumatic amputations in the US. In general, 5% of diabetes mellitus patients get foot ulcers, and 1% require an amputation.
- The danger of problems will be lower, and there will be better compliance if the patient is informed about the problem and the requirement for appropriate medical care.
Types of Diabetic Ulcers
Diabetes can cause a variety of foot ulcers.
- Where there is peripheral diabetic neuropathy but no ischemia from peripheral artery disease, neuropathic ulcers develop.
- When peripheral artery disease is evident but diabetic peripheral neuropathy is not apparent, ischemic ulcers can develop.
- When a person has peripheral neuropathy as well as ischemia brought on by peripheral artery disease, neuro ischemic ulcers can develop.
- Since the treatment strategy is influenced by the diagnosis, it is crucial to establish the etiology of a diabetic ulcer.
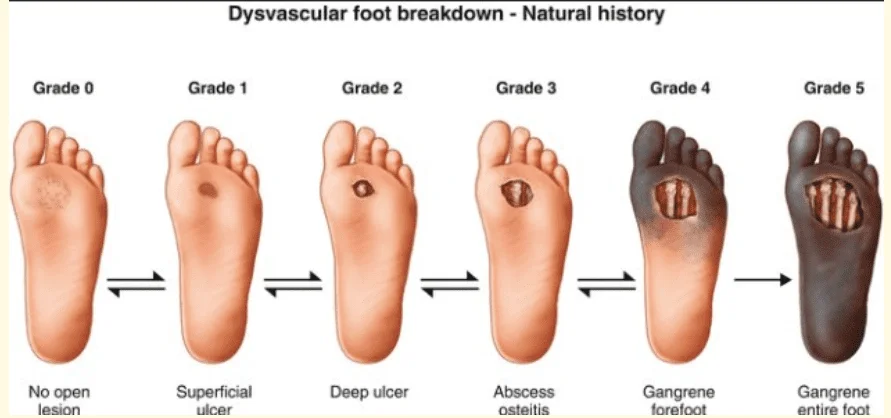
The Wagner Ulcer Classification System will be used by your doctor to rate the severity of your ulcer on a scale of 0 to 5:
- 0: no exposed sores; a healed sore may be present.
- 1: an ulcer that is only superficial and doesn’t reach deeper levels
- 2: a deeper ulcer that has spread to a tendon, bone, or joint capsule
- 3: involvement of deeper tissues, abscess, osteomyelitis, or tendonitis
- 4: gangrene affecting the forefoot or heel in any way
- 5: a foot with significant gangrenous involvement
Epidemiology
- Every year, there are between 9.1 and 26.1 million diabetic foot ulcers worldwide. A diabetic foot ulcer will occur in 15 to 25% of persons with diabetes mellitus throughout the course of their lives. The frequency of diabetic foot ulcers is certain to rise as the number of people newly diagnosed with diabetes rises each year.
- Diabetes mellitus individuals aged 45 and older are most likely to develop diabetic foot ulcers than patients of any age. In the US, foot ulcers are most common in Latinos, African Americans, and Native Americans.
Pathophysiology
- Typically, a diabetic ulcer develops in three phases. The callus-forming phase is the beginning step. The callus results from neuropathy. Sensory neuropathy produces a sensory loss, which results in continual damage, whereas motor neuropathy physically deforms the foot. Another cause is autonomic neuropathy, which causes the skin to dry out. Finally, repeated stress to the callus causes subcutaneous bleeding, and over time, it erodes and develops into an ulcer.
- In addition to having significant atherosclerosis of the tiny blood arteries in their legs and feet, people with diabetes mellitus also have vascular compromise, which contributes to diabetic foot infections. The healing process is slow mainly due to blood cannot get to the wound, which finally causes necrosis and gangrene.
Causes of Diabetic Foot Ulcer
The leading causes of ulcers in diabetes are:
- weak blood flow
- hyperglycemia, or high blood sugar
- nerve injury
- Angry or injured feet
- A kind of vascular illness called poor blood circulation causes inefficient blood flow to your feet. Additionally, poor circulation might make it more Ulcers are challenging to heal. The regulation of blood sugar is essential because high glucose levels might hinder the healing of an infected foot ulcer. Many times, ulcer infections are more difficult to treat in people with type 2 diabetes and other illnesses.
Loss of feeling in your feet might result from nerve injury, which has a long-term effect. Nerve damage can be uncomfortable and stinging. Nerve damage causes ulcer-causing sores that are painless and lowers the sensitivity to foot pain. Drainage from the afflicted region and occasionally a pronounced, non-painful lump are signs of ulcers.
History and Physical Examination
In order to properly treat individuals with diabetic ulcers, a thorough history must be obtained. The history should cover the onset and duration of diabetes, glycemic control, and other antecedent problems of diabetes, such as sensory neuropathy, history of peripheral vascular disease, callus, previous ulcer, past therapy, and the result. Information about the shoes and feet should be included in the whole history as well.
Anatomical abnormalities, calluses, and symptoms of vascular insufficiency, which can suggest hair loss, muscle atrophy, and the site of the ulcer, should all be looked for during the clinical examination of the foot. Examine with a monofilament to check for the presence of purulence, scabs, and signs of neuropathy.
Characteristics of neuropathy include:
- Paresthesia
- both hypo- and hyperesthesia
- Dysesthesia
- Anhydrosis
- The plantar metatarsal head, heel, tips of hammertoes, and other visible regions are where ulcers are most likely to occur.
Hammertoes, calluses, fissures, and brittle nails are further physical characteristics.
Evaluation
- Fasting blood sugar, glycated hemoglobin levels, a full metabolic panel, a complete blood count, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) are the most often laboratory tests performed during the examination of the ulcer. Recent recommendations and research indicate that in patients with diabetic foot ulcers, the results of culture specimens obtained by superficial swabbing do not correlate well with those obtained by deep tissue sampling; this implies that deep tissue samples may be more reliable for directing antimicrobial therapy than surface swab samples.
- The use of plain X-rays in radiological studies includes checking for the presence of a foreign substance, the air in the subcutaneous tissue, any indications of underlying fractures, and any underlying osteomyelitis. MRI is the test of choice when osteomyelitis is thought to be present.
- Diagnoses of underlying osteomyelitis can also be made with a technetium bone scan. To rule out underlying peripheral vascular disease, employ arterial Doppler in conjunction with the ankle-brachial index (ABI). A bedside test called the probe-to-bone test (PTB), which is carried out by probing the ulcer with a sterile metal probe, can aid in the identification of underlying osteomyelitis. It is a positive test if the probe touches the bone.[4] Results from the probe-to-bone test that are positive are particularly useful for people who have diabetes mellitus.
Treatment of Diabetic Foot Ulcer
- For the best results, diabetic foot ulcer treatment should be methodical. The most crucial thing is to determine whether there is any indication of an ongoing infection by getting a history of chills and fever and searching for purulence or at least two indicators of inflammation, such as discomfort, warmth, erythema, or induration of the ulcer. It is important to highlight that there may not always be significant systemic symptoms of infection, even in cases of severe diabetic foot infection.
- The next stage is to determine if the patient’s ulcer can be treated either inpatient or as an outpatient. Considerations for hospitalization include the need for parenteral antibiotics, worry about noncompliance, incapacity to care for the wound, and the capacity to relieve pressure. Antibiotics should be used to treat both types of patients.
- Staphylococcus aureus, Streptococcus, Pseudomonas aeruginosa, and E. coli are frequently found in diabetic foot ulcers. Staphylococcus aureus is more commonly carried by the nares and skin of diabetic individuals, which increases the likelihood that the ulcer will become infected.[8]The only time antibiotics are required is when there is a risk of infection. The kind, dose, and duration of the antibiotic are determined by how serious the illness is.
- Oral cephalosporins plus an amoxicillin-clavulanic acid mixture are typically used in outpatient antibiotic regimens (if MRSA is not a problem). Oral therapies include linezolid, clindamycin, cephalexin with doxycycline, or a trimethoprim-sulphamethoxazole combination if MRSA is suspected.
- The parenteral antibiotic regimens include piperacillin-tazobactam, ampicillin-sulbactam, and carbapenems like ertapenem or meropenem if the patient is penicillin allergic. Adding metronidazole for anaerobic coverage along with quinolones like ciprofloxacin or levofloxacin, or with cephalosporins like ceftriaxone, cefepime, or ceftazidime, are some of the additional combinations that are recommended. Among the intravenous medications that treat MRSA include vancomycin, linezolid, or daptomycin.
- The treatment of any underlying peripheral vascular disease is the next therapeutic step. Revascularization increases both and increases the ulcer’s probability of healing since inadequate blood flow restricts oxygen delivery and antibiotic distribution to the ulcer. The next action is to do local debridement or callus removal. For clean non-healing wounds, vacuum-assisted closure can be used. Hydrotherapy may help others get rid of disease-causing waste.
- The first therapy for Charcot’s foot is immobilization using braces or specially designed shoes, but the majority of patients will need surgical surgery like arthrodesis or an osteotomy.
- Last but not least, efforts should be taken to stop the development of new ulcers or the deterioration of existing ones, which happens when pressure is released from the location by utilizing walkers or therapeutic shoes. Hyperbaric oxygen treatment might be explored if the wound doesn’t heal in 30 days. There is frequently a delay in the wound healing process due to insufficient oxygen supply to the site. Both the pace of wound healing and the rate of complications are improved by hyperbaric oxygen therapy.
- A team of healthcare professionals, including a primary care doctor, a podiatrist, a vascular surgeon, an infectious disease expert, and wound care nursing personnel, is essential to get the greatest results.
- Staging The ulcer should be staged following a diagnosis. Wagner’s categorization system from 1981 is one of the most often used ones. It categorizes injuries.
depending on the depth, into six classes.
Grade / Features
- Initial superficial ulcer
- Deep ulcer affecting a tendon, bone, or joint
- Deep ulcer with an infection such as osteomyelitis
- Forefoot gangrene is described
- Gangrene affects the entire foot
However, this categorization has drawn criticism for just assessing the depth of the ulceration and leaving out other elements that are known to affect the result. The University of Texas Classification, among others, is one of the most widely used classifications in use today. It comprises an assessment of the depth of the wound as well as the kind of infection and ischemia depending on how the wound would ultimately turn out.
Prognosis
- If these ulcers are discovered quickly and the best therapy is started, the prognosis is favorable. Unfortunately, delays in treatment might have negative consequences and potentially necessitate the amputation of the foot. Patients with long-term hospitalization and readmission are at significant risk of having chronic diabetic ulcers.
Complications
- Amputation of the extremities is the complication that causes the most dread. The danger of infection, osteomyelitis, foot gangrene, and irreversible deformity are among the further consequences.
Postoperative and Rehabilitation Care
- Patients who require amputations require complete rehabilitation, which includes physical therapy, occupational therapy, and prosthetic limbs.
FAQs
Which five phases of a diabetic foot ulcer are there?
The natural history of the diabetic foot may be broken down into five stages: stage 1, a normal foot; stage 2, a high-risk foot; stage 3, an ulcerated foot; Stage 4 an infected foot, whereas stage 5 is a necrotic foot.
What is a typical reason for diabetic foot ulcers?
Poor glycemic control, calluses, deformed feet, incorrect foot care, uncomfortable footwear, peripheral neuropathy, poor circulation, dry skin, and other factors are frequent underlying causes. Neuropathy, which finally results in a foot ulcer, will appear in around 60% of diabetics.
What’s the most effective way to treat a diabetic foot ulcer?
Dressings and drugs used topically are part of proper wound treatment. These range from common solutions like saline to cutting-edge items like growth factors, bandages for ulcers, and skin replacements that have been proven to be incredibly successful in treating foot ulcers.
Which diabetic foot ulcer occurs most frequently?
An open sore or wound on a diabetic person’s foot, usually on the plantar area, or bottom of the foot, is known as a diabetic foot ulcer. 15% of people with diabetes get diabetic foot ulcers.
How are diabetic foot ulcers determined?
Your doctor could advise getting an X-ray to check for changes in the foot’s bone alignment, which can lead to ulcers. As a result of hormonal imbalances brought on by diabetes, X-rays may also show a reduction in bone mass.