Talus Fracture
Table of Contents
What is a Talus Fracture?
A talus fracture refers to a break or crack in the talus bone, which is located in the ankle joint between the lower leg bones (tibia and fibula) and the foot bones. The talus is a small, cube-shaped bone that plays a crucial role in weight-bearing and transmitting forces between the leg and foot.
Due to this, the talus is essential for movement in the ankle, a fracture usually causes in significant lack of movement and performance. A talus fracture that does not recover adequately can result in complications, comprising a limp, arthritis, and constant pain. For this cause, most talus fractures demand operative intervention.
The talus rates as the second most considerable tarsal bone with distinctive anatomic characteristics and performs an essential function in the mobility of the foot and ankle as it is the osseous connection between the leg and the foot. The anatomy of the talus is relatively complex with three distinct articulations with particular characteristics comprising the subtalar joint with its three faces. The talus splits into the head, neck, and body Unsurprisingly, articular cartilage covers around two-thirds of the surface, and there are a few muscle or tendon attachments as well. Hyaline cartilage covers the convex talar head, which articulates with the navicular at the anterior lower aspect to secure the ankle and midfoot. The talar head also articulates with the calcaneus through the anterior facet at its inferior margin (anterior part of the subtalar joint )
The center or anteromedial & posterior or posterolateral aspects of the talar body are used to articulate it inferiorly with the calcaneus. The posterior facet is the biggest of the two making up the posterior subtalar joint while the middle facet articulates with the sustentaculum tali (medial process from the calcaneus). By the way, it is the middle facets of the subtalar joint which are most usually participating in the talocalcaneal coalition accounting for forty-five percent of the tarsal alliance. At the tibiotalar joint, the body’s superior side, the talar dome or trochlea, articulates with the tibia. The neck is the portion of the talus that connects the head to the body and is devoid of cartilage or an articular surface. The sinus tarsi and tarsal canal lie on the inferior border of the neck.
The posterior process of the body is combined of the medial and lateral tubercles. The flexor hallucis longus tendon passes between these two tubercles. A Stieda process is an anatomic variant characterized as an extension of the lateral tubercle. The os trigonum is some other normal variable because of the non-fusion of the lateral tubercle ossification center. Both of these normal variables may be involved in pathology varying from fracture to os trigonum syndrome.
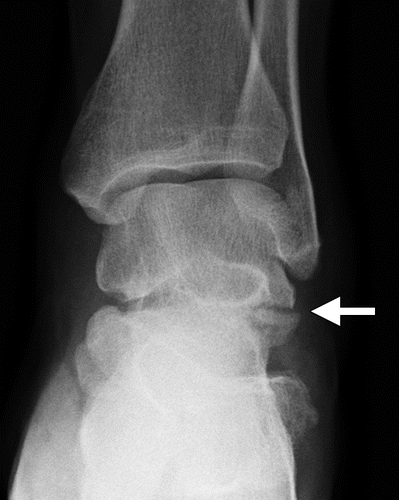
The lateral process extends from the outer side of the body of the talus. This process articulates with the fibula superiorly and forms the anterolateral part of the posterior facet of the posterior subtalar joint. Fracture of the lateral process has been described as a “snowboarder’s fracture” and is ordinarily incomprehensible on first radiographs. Judgment of the lateral process of the talus is excellent on AP radiographs of the ankle.
Three arteries feed blood to the talus: the perforating peroneal, dorsalis pedis, and posterior tibial arteries. The blood circulation is predominately extraosseous due to the extended articular cartilage coverage and is hence easily discontinuous in the setting of displaced fractures or dislocation resulting in avascular necrosis or osteonecrosis.
Anatomy
The talus is the bone that creates the distal portion of the ankle joint (the tibia and fibula create the upper portion). The ankle joint permits your foot to move up and down. The talus also lies above the heel bone (calcaneus). Jointly, the talus and calcaneus compose the subtalar joint. This joint permits your foot to move inward and outward, which is necessary for walking on irregular ground.
The talus connects the foot and leg, allowing it to take load and stress forces across the ankle joint. It is mostly surrounded by articular cartilage, the white greasy material that covers all joint surfaces. This cartilage permits the talus to move smoothly in front of its neighboring bones.
Pathophysiology
The talar vascular supply and its absence of muscular attachments predispose it to a marked injury in the setting of trauma. Since a large ratio of the surface of the bone has a cartilage covering, the surface region convenient to vascular supply is restricted. Besides, since talar fractures connect with high-impact injuries, correlated musculoskeletal and vascular injuries can be correlated. Not surprisingly, displaced fractures and dislocations have a greater incidence of subsequent osteonecrosis. Because of these respects, talar fractures can be correlated with marked morbidity and long-term disability if not properly treated.
Epidemiology
In general, talar fractures are not common, including lower than one percent of all fractures in the human body and between three percent and six percent of fractures of the foot. There is probably no age preference for these fractures, although the correlation with MVC would indicate advanced incidence in more youthful patients. Likewise, there is a significant men preference, with up to seventy-three percent of talar fractures happening in males. While the incidence of these fractures is probably not rising, these kinds of injuries (and, in special, the more extreme fracture types) are increasingly being noticed because of increased survival from severe trauma. Some reports indicate that there can be an enhanced incidence of lateral process fractures because of snowboarding.
Talar head fractures are a slightly not uncommon kind of talar fracture, compromising five to ten percent among talar fractures. Talar neck fractures were standardly thought the most familiar kind of fracture, first defined in WW1 pilots, though current proof recommends that they are likely less common compared to body fractures, possessing around five percent of talar fractures. Dissimilarities can be connected to contrasts in the description of anatomic borders between the neck and body (discussed down). It is worth mentioning that talar neck and body fractures connect with calcaneal and spine fractures. There is also considerable variation in the documented incidence of body fractures, thirteen to sixty-one percent.
What are the different types of Talus Fracture?
Your talus bone can fracture in various places and in various ways. Talus bone fractures contain:
- Neck. The most expected kind of talar fracture appears in the mid-aspect of your talus. This is known as the neck. The neck is located between the “head” of your talus, which is far below your foot, and the “body” of your talus, which is under your tibia by your ankle joint.
- Lateral process. The exterior of your talus bone is known as the lateral process. These kinds of fractures happen when your ankle is moved externally to the side. Lateral process talus fractures are generally noticed in snowboarders and are occasionally understood as “snowboarder fractures.”
- Avulsion fractures. A talar avulsion fracture happens when a slight portion of your talus bone rips out from the insertion of the bone where it’s connected to a ligament or tendon.
- Stress fractures. Also known as the special fracture defined as a talar stress fracture is a little break in your talus bone. This kind of fracture occurs due to the overuse or repeated stress put on your talus bone.
Classification of Talus Fracture
Fractures can happen in all components of the talus bone. Most generally, the talus fracture in its mid-portion is known as the “neck.” The most expected kind of talar fracture appears in the mid-aspect of your talus. This is known as the neck. The neck is located between the “head” of your talus, which is far below your foot, and the “body” of your talus, which is under your tibia by your ankle joint.
The talus may even fracture through an eminence on the exterior of the bone known as the lateral process. These kinds of fractures happen when your ankle is moved externally to the side. Lateral process talus fractures are generally noticed in snowboarders and are occasionally understood as “snowboarder fractures.”
Talus fractures can be typed by how much the broken fragment of bone has pushed out of its original position.
- Minimally displaced or regular fractures: This kind of fracture is slightly out of place. The cracked ends of the bones line up perfectly or nearly accurately. In a minimally displaced fracture, the bones commonly remain in position during recovery. operative to fix the bones is not needed.
- Displaced fracture. A displaced fracture happens when the bone fracture and the elements move out of their original position. The quantity of displacement correlates to the force of the trauma. Greatly displaced fractures are more potential to be unstable. They usually need an operative to fix the alignment and give the best option for a return to the normal function of the foot and ankle.
- Open fracture: When cracked bones crack through the skin and are exposed to the environment, the trauma is known as an open or compound fracture. Open fractures usually involve more significant injury to the nearby muscles, tendons, and ligaments. In addition, open fractures reveal the fracture area to the environment, permitting debris from the exterior to infiltrate the wound. For this cause, they have a greater risk of infection and frequently take a more extended time to recover.
Cause of Talus Fracture
Most talus fractures are the result of high-impact trauma for example a road traffic accident or a drop from height. Injuries from sports, particularly snowboarding, is another, though less common, cause of talus injuries.
Following are the few common causes are:
- Falls: Falls from a height or on uneven surfaces are a frequent cause of talus fractures. Landing on the foot with significant force can lead to a fracture of the talus bone.
- Motor vehicle accidents: Car accidents, motorcycle accidents, or other high-impact collisions can exert immense force on the ankle and foot, potentially causing talus fractures.
- Sports injuries: Participating in sports that involve running, jumping, or sudden changes in direction can increase the risk of talus fractures. Activities such as basketball, soccer, skiing, or gymnastics may involve high-velocity movements or awkward landings that can lead to fractures.
- Twisting injuries: Twisting or rotating the ankle forcefully, especially when the foot is fixed or caught on an object, can cause talus fractures. This type of injury often occurs during activities like hiking, stepping on uneven ground, or getting the foot trapped in a crevice.
- Crushing injuries: When the foot or ankle is crushed between heavy objects or trapped in a confined space, it can result in severe fractures, including talus fractures.
- Occupational accidents: Certain occupations or work environments that involve heavy machinery, construction sites, or manual labor can increase the risk of traumatic injuries to the foot and ankle, potentially leading to talus fractures.
Symptoms of Talus Fracture
Patients with talus fractures usually experience:
- Acute pain
- Ankle swelling
- Incapacity to walk or bear the load on the feet
- Considerable swelling, bruising, and tenderness
- Inability to move the ankle joint
- Ankle Deformity
- Tingling or numbness if an associated injury
It is important to note that talus fractures can sometimes be associated with additional injuries, such as ligament damage, fractures of neighboring bones, or dislocations. These injuries can further contribute to pain, swelling, and functional limitations.
Differential Diagnosis
With the provided history of high-impact injury to the foot and ankle and the above clinical conclusions, the preliminary differential diagnoses are fractures of other bones of the foot and ankle with or in the absence of injuries to the soft tissues of the foot and ankle for example ligaments, tendons, and neurovascular structures.
Radiographic evaluation often narrows the differential diagnosis. Accessory ossicles are standard variants of the foot and ankle which need differentiation from traumatic injury. The os trigonum can imitate a fracture of the posterior process. A recent fracture will have radiographic results of irregular, irregular margins, while an os trigonum will have smooth, well-corticated margins.
Diagnosis
Examination
Many individuals with talus fractures will go to an immediate supervision center or emergency room for earlier management due to the severity of their symptoms.
Physical Examination
- After inspecting your symptoms and medical history, your physician will do a careful examination. During the examination test, he or she will:
- Inspect your foot and ankle carefully to notice if there are any scratches from the trauma.
- Review to visit if you can push your toes, and can feel things on the bottom of your foot. In some circumstances, nerves may be injured at the same time that the bone is broken.
- Inspect your pulse at critical points of the foot to be sure that there is adequate blood circulation to the foot and toes.
- inspect to see that stress from fluids is not constructing up in the muscles of the leg, a condition known as compartment syndrome. Compartment syndrome can cause in lack of sensation and function and needs emergency operation once it is diagnosed.
- Decide if you have any other trauma by investigating the rest of your traumatic foot, as well as your legs, pelvis, and spine.
Imaging Tests
Information from diagnostic imaging tests will support your physician to determine whether the operation is needed and will be required for operative planning.
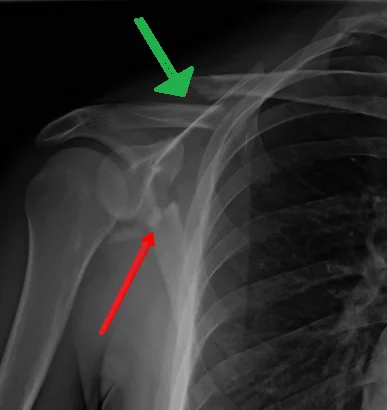
X-rays. X-rays are the most typical and largest general diagnostic imaging procedure. An X-ray can reveal if the bone is cracked and whether there is displacement (fragments are out of their original position ). It can even show how many broken pieces of bone there are.
Computerized tomography (CT) scan. If your physician still needs more details after considering your x-rays, a CT scan can also be ordered. A CT scan reveals a cross-sectional picture of your foot. It can give useful information about the severity of the fracture by allowing your physician to see the fracture lines more undoubtedly.
Prognosis
The nonoperative intervention of nondisplaced talar head fractures and proper operative management of displaced talar head fractures correlate with excellent results. The adequate vascular circulation of the talar head, as compared to the neck and body, is at least partially responsible for its generally positive prognosis.
Concerning talar neck fractures, there is a strong positive link between the modified Hawkins-Canale fracture kind and the threat of avascular necrosis. Also, investigations have revealed that the degree of fracture displacement, degree of comminution, size of soft-tissue trauma, and success of operative reduction correlate with the development of osteonecrosis and other consequences, for example, post-traumatic osteoarthrosis with rates of osteonecrosis in Type I, II, III, and IV fractures declared at 0 to 15%, 20 to 50%, 100%, and 100%, respectively. The Hawkins sign is a radiographic finding of a thin linear subcortical radiolucency appreciated in post-treatment pictures which shows preserved blood circulation to the talar body in the setting of talar neck fractures. Talar dome osteochondral defects which are stable and nondisplaced frequently heal well, while displaced unstable fragments may undergo osteonecrosis if not surgically repaired The worst result for talar body fractures is crushed comminuted fractures.
Treatment of Talus Fracture
As with any painful ankle injury, a talus fracture requires immediate first aid treatment that involves immobilizing and covering the injured extremity with a well-supported splint close to the rear of the foot and leg. The splint must extend from the toe to the upper leg. Raising the foot beyond the level of the heart allows to minimize swelling and pain. Characteristic treatment is based on the severity and the kind of fracture, so it is necessary to pursue immediate medical attention.
Nonoperative Treatment
Many talus fractures require surgery due to the high-impact trauma that causes the injury. Stable, well-aligned fractures, regardless, can usually be managed in the absence of the operation. This is commonly performed with a mixture of immobilization and followed by rehabilitation.
- Casting. A cast will keep the bones in your foot in position while they recover. For six to eight weeks you have to wear the cast. During this time, you will be requested to restrict the quantity of stress you place on your foot. The purpose is for the bone to heal sufficiently for you to take the load on it without the threat that it will move out of position.
- Rehabilitation. When the cast is removed, your physician will give you exercises to help restore your range of movement and strengthen your foot and ankle.
Surgical Treatment of Talus Fracture
If the bones have moved out of position(displaced), the operative internally assesses and stabilizes the broken pieces consequences in the best outcome and lowers the threat of prospective complications.
Open reduction and internal fixation. The bone fragments are first moved (reduced) into their original anatomical alignment before this procedure. They are then held together with individual screws or metal plates and screws.
Recovery
Bones have a special capacity to recover. The more extreme your injury, yet, the extended your healing time can be. After the operation, your feet will be in a sling or cast for two to eight weeks. This is based on the type and pattern of the injury and how well the recovery progresses. Your physician will take X-rays to confirm that the bones remain in position and are recovering properly.
Pain Management
After the operation, you will feel some pain. This is a natural component of the healing procedure. Your physician and nurses will work to ease your pain, which can assist you to recover from the operation faster.
Pharmaceuticals are usually prescribed for temporary pain comfort next to the operation.
Numerous medications, including opioids, non-steroidal anti-inflammatory medicines (NSAIDs), and local anesthetics, are known to help manage pain. Your physician can use a combination of these medicines to enhance pain comfort, as well as reduce the demand for opioids.
Be conscious that although opioids help reduce pain after the operation, they are a narcotic and can be addictive. Opioid dependency and overdose have become urgent public health issues in the U.S. It is necessary to use opioids just as directed by your physician. As soon as your pain starts to improve, prevent taking opioids. Talk to your physician if your discomfort has not started to improve within a few days of your operation.
What does fracture Physiotherapy include?
Physiotherapy must begin immediately after the fracture has been immobilized. Physical therapy during fracture recovery will focus on:
- Facilitating recovery
- Encouraging weight loading
- Maintaining the strength of weakened muscles
- Maintaining the range of movement of the involved and nearby joints
- Decreasing pain
- Decreasing swelling
After your fracture has recovered or your cast has been removed physical therapy is resumed for three to twelve months or until you have recovered your complete level of function.
The goal of physical therapy is:
- Advancement in weight-loading activities
- Return to complete function
- Return strength and a complete range of movement to muscles or joints
- Concentrate on sport-specific rehabilitation
- Optimize the range of movement at the involved joint
Exercises
An ankle fracture exercise protocol must be the major component of your ankle rehabilitation next to a fracture. Be certain to follow your physical therapist’s directions closely and ask queries if you have any.
- Exercises for ankle fracture rehabilitation may contain:
- Exercises for ankle range of movement
- Ankle strengthening exercises
- Hip and knee exercises (to assist enhance walking ability)
- Balance and proprioception conditioning
- Exercise to enhance functional mobility and walking ability
You’ll most probably need to achieve a home exercise protocol for your fracture ankle. This protocol may continue for many months later to physical therapy has stopped, and the protocol may be a significant part of your long-term rehabilitation success.
Complications After Talus Fracture
Failure to reduce a displaced head or neck fracture can result in secondary osteoarthrosis or necrosis. As noted above, even with proper operative intervention, Type III and IV talar neck fractures are correlated with up to complete danger of osteonecrosis. Osteonecrosis and secondary osteoarthrosis are typical complications of talar body fractures. Associated fractures of the head or neck raise the possibility of complications in body fractures. An increased likelihood of avascular necrosis results from the greater prevalence of bone loss and nonanatomic decrease in crush comminuted talar body fractures.
Avascular Necrosis (AVN)
An increased likelihood of avascular necrosis results from the greater prevalence of bone loss and nonanatomic decrease in crush comminuted talar body fractures. Occasionally, the blood circulation just returns to the bone and regular healing begins. On the other hand, regardless, the bone cells die without a blood supply, causing a slight continuous and very painful collapse of the bone. This condition is called avascular necrosis (AVN) of the Talus.
When the bone collapses, the articular cartilage surrounding the bone is also injured. Without this smooth cartilage, bone rubs in the form of bone, causing increased pain, arthritis, and lack of movement and performance. The more intense the talus fracture, the more probable it is that AVN will happen. Even fractures that are treated properly, possessing those that are managed operatively, may result in AVN.
Post-traumatic Arthritis
Posttraumatic arthritis is a kind of arthritis that results after a trauma. Even when your bones naturally heal, the cartilage protecting them can suffer damage, which gradually will cause pain and stiffness. Almost all talus fractures cause some degree of posttraumatic arthritis. In conditions of extreme arthritis or avascular necrosis that limit activity, additional operation, for example, a joint fusion or ankle replacement, is perhaps the most satisfactory alternative to relieve symptoms.
Malunion
A malunion represents a fractured bone healed in an inadequate position. A malunion can result in long-term problems like difficulty in gait.
Nonunion
A nonunion represents a fractured bone that didn’t recover after an extended period of time.
FAQ
The recovery from a talus fracture can be lengthy due to until the bone is recovered, you cannot put a load on your feet. Hence, almost all talus fractures demand a minimum of six to twelve weeks of protection from weight-loading.
Nondisplaced talar head fractures accept conservative management. Displaced talar head fractures need an operation to reduce the malalignment of the talonavicular joint to minimize the chance of osteoarthrosis and osteonecrosis. Type I neck fractures can be not indicated for conservative management.
Recovery can be extended. No load or walking on the limb will be permitted for eight to twelve weeks. Once the bone is recovered, exercise and physical therapy are begun to maximize the role of the ankle. The patient must expect some foot swelling for many months after the procedure.
Most of the time fractures possess the talus demand operation. All the same, if the fracture is in an adequate alignment and appears stable, you might be managed in the absence of operation using a splint or cast. If the bones are shifted out of place, the operation is normally needed to fix the bones.
The Talar Tilt Test is the most common orthopedic test to be performed after an inversion trauma in command to measure the lateral ankle ligaments. It assesses the lateral ligaments of the ankle in three various positions.
Talar torsion (sometimes called subtalar version) outcome when there is a ten-degree or higher change in the final position of the talar head. This can result in an adducted position of the forefoot, frequently mistakenly known as “forefoot adducts, which really only applies to the metatarsals, and not at all to the talus.
Talus fractures are frequently resulted from a high-impact injury or direct trauma, possessing slip from a height, ladder, or stair, and car or road traffic accidents. In sports like snowboarding or when bending an ankle, talus fractures can also occur, which can lead to little shards of bone coming away.
Talus fractures are particularly painful injuries and can result in long-term difficulties with the foot and ankle. There are before and late complications. Before complications most usually are associated with the considerable swelling that can happen after these injuries, which can result in wound problems and infection.