Fracture: Type, Cause, Symptoms, Diagnosis, Treatment
Table of Contents
What is a Fracture?
A fracture is a break, usually in a bone. If the broken bone punctures the skin, it is called an open or compound, fracture. Fractures commonly happen because of car accidents, falls, or sports injuries. Other causes are low bone density and osteoporosis, which cause the weakening of the bones.
A bone fracture is a medical condition where the continuity of the bone is broken.
A significant percentage of bone fractures occur because of high-force impact or stress.
However, a fracture may also be the result of some medical conditions which weaken the bones, for example, osteoporosis, some cancers, or osteogenesis imperfecta (also known as brittle bone diseases).
A fracture caused by a medical condition is known as a pathological fracture.
Your risk of fracture depends, in part, on your age. Broken bones are very common in childhood, although children’s fractures are generally less complicated than fractures in adults. As you age, your bones become more brittle and you are more likely to suffer fractures from falls that would not occur when you were young.
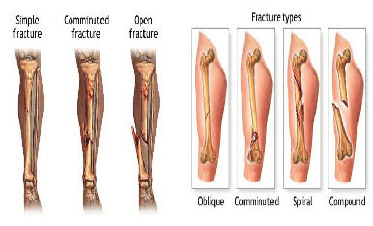
There are many types of fractures, but the main categories are displaced, non-displaced, open, and closed.
Displaced and non-displaced fractures refer to the alignment of the fractured bone.
In a displaced fracture, the bone snaps into two or more parts and moves so that the two ends are not lined up straight. If the bone is in many pieces, it is called a comminuted fracture. In a non-displaced fracture, the bone cracks either part or all of the way through, but does move and maintains its proper alignment.
A closed fracture is when the bone breaks but there is no puncture or open wound in the skin. An open fracture is one in which the bone breaks through the skin; it may then recede back into the wound and not be visible through the skin. This is an important difference from a closed fracture because with an open fracture, there is a risk of a deep bone infection.

Fast facts on fractures
Here are some key points about fractures. More detail and supporting information is in the main article.
Most bone fractures are caused by falls and accidents.
Bone fractures caused by the disease are referred to as pathological fractures.
A compound fracture is one that also causes injury to the overlying skin.
There are a number of different types of fractures, including avulsion, comminuted, and hairline fractures.
Bone healing is a natural process, treatment revolves around giving the bone optimum conditions to heal itself.

What is a bone fracture?
The word “break” is commonly used by lay (non-professional) people.
Among doctors, especially bone specialists, such as orthopedic surgeons, “break” is a much less common term when talking about bones.
A crack (not only a break) in the bone is also known as a fracture. Fractures can occur in any bone in the body.
There are several different ways in which a bone can fracture; for example, a break to the bone that does not damage surrounding tissue or tear through the skin is known as a closed fracture.
On the other hand, one that damages the surrounding skin and penetrates the skin is known as a compound fracture or an open fracture. Compound fractures are generally more serious than simple fractures, because, by definition, they are infected.
Most human bones are surprisingly strong and can generally stand up to fairly strong impacts or forces.
However, if that force is too powerful, or there is something wrong with the bone, it can fracture.
The older we get, the less force our bones can withstand. Because children’s bones are more elastic, when they do have fractures they tend to be different. Children also have growth plates at the end of their bones – areas of growing bone – which may sometimes be damaged.
Pathophysiology
The natural process of healing a fracture starts when the injured bone and surrounding tissues bleed, forming a
fracture hematoma. The blood coagulates to form a blood clot situated between the broken fragments. Within a few days, blood vessels grow into the jelly-like matrix of the blood clot. The new blood vessels bring phagocytes to the area, which gradually removes the non-viable material. The blood vessels also bring fibroblasts into the walls of the vessels and these multiply and produce collagen fibres. In this way, the blood clot is replaced by a matrix of collagen. Collagen’s rubbery consistency allows bone fragments to move only a small amount unless severe or persistent force is applied.
At this stage, some of the fibroblasts begin to lay down bone matrix in the form of collagen monomers. These monomers spontaneously assemble to form the bone matrix, for which bone crystals (calcium hydroxyapatite) are deposited in amongst, in the form of insoluble crystals. This mineralization of the collagen matrix stiffens it and transforms it into bone.
In fact, bone is a mineralized collagen matrix; if the mineral is dissolved out of bone, it becomes rubbery. Healing bone callus on average is sufficiently mineralized to show up on X-ray within 6 weeks in adults and less in children. This initial “woven” bone does not have the strong mechanical properties of mature bone. By a process of remodelling, the woven bone is replaced by mature “lamellar” bone. The whole process may take up to 18 months, but in adults, the strength of the healing bone is usually 80% of normal by 3 months after the injury.
Several factors may help or hinder the bone healing process. For example, tobacco smoking hinders the process of bone healing,[8] and adequate nutrition (including calcium intake) will help the bone healing process. Weight-bearing stress on bone, after the bone has healed sufficiently to bear the weight, also builds bone strength.
Although there are theoretical concerns about NSAIDs slowing the rate of healing, there is not enough evidence to warrant withholding the use of this type analgesic in simple fractures.
Types of Fractures:
There is a range of fracture types, including:
Avulsion fracture – a muscle or ligament pulls on the bone, fracturing it.
Comminuted fracture – the bone is shattered into many pieces.
Compression (crush) fracture – generally occurs in the spongy bone in the spine. For example, the front portion of a vertebra in the spine may collapse due to osteoporosis.
Fracture dislocation – a joint becomes dislocated, and one of the bones of the joint has a fracture.
Greenstick fracture – the bone partly fractures on one side, but does not break completely because the rest of the bone can bend. This is more common among children, whose bones are softer and more elastic.
Hairline fracture – a partial fracture of the bone. Sometimes this type of fracture is harder to detect with routine xrays.
Impacted fracture – when the bone is fractured, one fragment of bone goes into another.
Intraarticular fracture – where the break extends into the surface of a joint
Longitudinal fracture – the break is along the length of the bone.
Oblique fracture – a fracture that is diagonal to a bone’s long axis.
Pathological fracture – when an underlying disease or condition has already weakened the bone, resulting in a fracture (bone fracture caused by an underlying disease/condition that weakened the bone).
Spiral fracture – a fracture where at least one part of the bone has been twisted.
Stress fracture – more common among athletes. A bone breaks because of repeated stresses and strains.
Torus (buckle) fracture – bone deforms but does not crack. More common in children. It is painful but stable.
Transverse fracture – a straight break right across a bone.
What is a broken bone (fracture)?
Bones make up the skeleton of the body. They allow us the ability to interact with our environment and lift out body up against gravity. Bones are attachment points for muscles which allows us to run, jump, sit, kneel, grasp, and lift. Bones also protect organs from potential damage, and the bone marrow (tissue inside of bones) is responsible for blood cell production.
Bones are the body’s storage area for calcium. On a cellular level, calcium is always entering and exiting bone under the influence of the body’s hormones. Parathyroid hormone increases calcium levels in the bloodstream, meaning, that it regulates it’s release by bone and decreasing bone density. Calcitonin decreases blood calcium levels and helps restore calcium to bone. Calcium is needed in the blood stream to help muscle cells including the heart to function. Hormone levels will sacrifice calcium in bone to maintain blood calcium levels in a normal range. For that reason, calcium and Vitamin D are important to maintain calcium stores in the body.

What causes a broken bone?
When a bone has an outside force exerted upon it, like a blow or a fall, there is a potential that it cannot withstand the amount of force and it breaks. That loss of integrity results in a fracture. It is important to remember that a fracture, break, or crack all describe the same situation, an injury to the bone where it has been damaged. One term is not more serious than another. Fracture, break, and crack all mean the same thing.
Depending upon the situation, the amount of force required may not be very great. For people with osteoporosis, the bones lack calcium and are brittle, a minor injury or even gravity may create enough of a force to cause a vertebral compression fracture of the back or a hip fracture
What are the most common types of broken bones?
Fractures are usually described by their location, how the bones are aligned, whether there are associated complications with blood and nerve function, and whether the skin is intact at the injury site.
The terms and definitions used in medicine to describe fractures allow healthcare professionals to describe exactly where in the bone the fracture is located. For a reference point, the heart is considered the center of the body, and the anatomic descriptions are based on their location in reference to the heart. When describing a location on or in the body, imagine standing straight up, looking forward with the arms slightly away from your side, and the palms turned forward.
Common anatomic terms used to describe fractures include the following:
Proximal (closer to the center of the body) and Distal (further from the center): the elbow is proximal to the wrist and the wrist is distal to the elbow.
Anterior (toward the front of the body) and Posterior (toward the back): The chest is anterior to the back and the back is posterior to the chest.
Medial (toward the middle of the body) and Lateral (to the outer edge of the body): The ears are lateral to the nose and the nose is medial to the ears.
By thinking of the body in the anatomic position, fractures can be described by their location in the bone and how the parts are aligned and related to each other. Fractures are either displaced or non-displaced, meaning that they are adequately aligned or not. Some physicians suggest that all fractures have some displacement and prefer the term “minimally displaced.”
The description of the fracture also includes the direction it takes within the bones.
Transverse: the fracture travels across the bone
Oblique: the fracture occurs at an angle
Spiral: –the fracture spirals or extends down the length of the bone
Comminuted: the fracture has more than two parts, and multiple fragments are present.
Special terms:Greenstick: In young children, the bones are not yet solid and when force is applied, it tends to bow and not break completely through. The term comes from a similar situation when trying to break a young branch off a tree.
Torus: In children, when only one part of a bone buckles it is called a torus or incomplete fracture.
Open fracture: An open fracture describes the situation where the bone penetrates through the skin.
The skin is very important in protecting the inside of the body from infection. If the skin overlying a broken bone is damaged, whether it is cut, torn or scraped, there is potential for bacteria from the outside world to invade the broken bone and cause an infection.
Fractures are classified as open (if the skin is damaged) or closed (if the skin is intact). An open fracture may require an orthopedic surgeon to wash out the fracture site to prevent osteomyelitis (bone infection). Depending upon circumstances, the type of fracture, the amount of contamination to the skin and wound, and the person’s condition, this procedure may take place in the operating room.
Compression fracture
The spine is comprised of 7 cervical, 12 thoracics, and 5 lumbar vertebrae. The spine holds the body erect against gravity and protects the spinal cord. Compression fractures can be caused by osteoporosis, injury, or trauma.
People with osteoporosis lose calcium from the bones, and the vertebrae may become weak and unable to hold up against the forces of gravity, so they gradually compress over time.
A compression fracture due to an injury may or may not have spinal cord or nerve root irritation because of the fracture.
A compression fracture due to trauma most likely occurs from a motor vehicle crash or fall from height.
Skull fracture
The purpose of the skull is to protect the brain. It is a flat bone and it takes a significant direct blow to cause a fracture. Because the main concern is an injury to the brain and not the skull injury, plain X-rays are not routinely performed to look for a skull fracture. Instead, a CT scan of the brain is recommended if there is concern about a brain injury. Skull fractures are often associated with localized swelling and bleeding at the site of injury.
Basilar skull fractures describe damage to bone at the base of the brain. Physical findings may include bloody drainage from the ear or nose, bruising behind the ear (Battle’s sign), and bruising around the eyes (Raccoon eyes).
With a depressed skull fracture, the bone is broken and fragments are pushed inward. Depending upon the depth of the bony depression and whether there is brain tissue involvement, surgery may be required. With an open skull fracture, the scalp is lacerated and the wound may connect with the fibrous coverings of the brain (meninges). Surgery is often performed to help prevent infection.
Stress fracture
Stress fractures are the result of multiple microtraumas where the bone cannot tolerate and absorb repeated stresses placed upon it. It is an overuse injury and is often seen in the lower leg, especially with runners and other athletes. If untreated, and if the person continues to participate in an offending activity, the stress fracture may progress to a completed fracture. These are most often seen in athletes who participate in running, tennis, basketball, and other sports that involve running and jumping on hard surfaces.
March fracture is the name given to a stress fracture of the metatarsal bone of the foot. They are described as soldiers who are forced to walk or “march” for prolonged distances.
What are the most common bones that are broken?
The most common fractures involve the clavicle (collarbone), the forearm (radius and ulna), the wrist, the ankle, and the hip. Closed fractures are more common than open fractures (the skin overlying the injury is intact and not damaged).
In children, a fracture of the distal radius is most common. The break occurs in the radius near the wrist but usually does not involve the joint itself.
Broken hand or fingers
Injuries to the hands and fingers are very common because they are exposed in daily activities. In addition to the bones, the health care professional will be interested in making certain there are no tendon or nerve injuries associated with any broken bone(s). Because the anatomy of the hand is so complex, complicated fractures may be referred to an orthopedic or plastic hand specialist. Many of them will only require splinting or casting, but occasionally surgery will be necessary.
Broken wrist
Falling on an outstretched hand is the most common reason for a wrist fracture. It is often the distal radius (see illustration) that is damaged, and the fracture may involve more than one bone. Aside from the radius, wrist fractures may also include fractures of the carpal bones of the wrist (carpus), those that connect the radius to the long bones of the hand (metacarpals). Doctors often look for fractures of the scaphoid bone (the bone between the bottom of the thumb and the top of the radius), and dislocations of the lunate (the bone next to the scaphoid bone) that may be difficult to see on plain X-ray.
In some cases, the wrist is splinted even if X-rays are normal because upon physical examination the doctor may be concerned about a potential occult or hidden fracture (the fracture is so small that it does not show up on an X-ray).
Depending upon the bone that is injured and it’s alignment, surgery may or may not be required. Regardless of the treatment, the goal is to have a normally aligned wrist, especially if the fracture involves the joint surface.
Poor alignment may lead to arthritis in the future.
Broken hip
Hip fractures are perhaps the most common fracture seen in people 75 years of age or older. While falls and trauma may be the obvious cause, many times, people are more susceptible to hip fracture because of osteoporosis and sometimes the hip will break spontaneously.
The hip joint is made up of the interconnection of two bones in a ball and socket: 1) the socket in the pelvis (acetabulum), and 2) the ball (femoral head). Hip fractures refer to the femur fracture.
Almost all hip fractures require surgery and the type of surgery depends upon where in the femur the fracture is located.
Broken leg
Each of the many bones of the lower extremity is at risk for fracture. Leg fractures also may involve the knee joint, and treatment depends upon the type of fracture. Similarly, fractures of the lower leg (tibia and fibula) and talus (the most proximal bone in the foot) may involve the ankle joint.
Fractures and dislocations of the foot may be as complex as the hand. Because of the anatomy, they may also be more difficult to diagnose on plain X-rays.
Broken toe
Broken toes are a common fracture and may be diagnosed by history and physical examination. X-rays may or may not be needed depending on the clinical situation.
Broken shoulder
The clavicle (collarbone) fracture is one of the most commonly seen broken bones, fracture of the humeral head (the ball) is quite common an older person who falls.
Depending upon the amount of comminution (into how many pieces the humeral head breaks) surgery may or may not be required. Initial treatment usually begins with a sling.
The scapula or shoulder blade is a flat bone and very difficult to break. The mechanism is usually a direct blow.
Any scapula fracture needs to be evaluated for related injuries.
Symptoms
The signs and symptoms of a fracture vary according to which bone is affected, the patient’s age and general health, as well as the severity of the injury. However, they often include some of the following:
- pain
- swelling
- bruising
- discolored skin around the affected area
- angulation – the affected area may be bent at an unusual angle
- the patient is unable to put weight on the injured area
- the patient cannot move the affected area
- the affected bone or joint may have a grating sensation
- if it is an open fracture, there may be bleeding
When a large bone is affected, such as the pelvis or femur:
the sufferer may look pale and clammy there may be dizziness (feeling faint) feelings of sickness and nausea.If possible, do not move a person with a broken bone until a healthcare professional is present and can assess the situation and, if required, apply a splint. If the patient is in a dangerous place, such as in the middle of a busy road, one sometimes has to act before the emergency services arrive.
Causes of Fractures
Most fractures are caused by a bad fall or automobile accident. Healthy bones are extremely tough and resilient and can withstand surprisingly powerful impacts. As people age, two factors make their risk of fractures greater:
Weaker bones and a greater risk of falling.
Children, who tend to have more physically active lifestyles than adults, are also prone to fractures.
People with underlying illnesses and conditions that may weaken their bones have a higher risk of fractures.
Examples include osteoporosis, infection, or a tumor. As mentioned earlier, this type of fracture is known as a pathological fracture.
Stress fractures, which result from repeated stresses and strains, commonly found among professional sports people, are also common causes of fractures.
Complications
Some fractures may lead to serious complications including a condition known as compartment syndrome. If not treated, eventually, compartment syndrome may require amputation of the affected limb. Other complications may include non-union, where the fractured bone fails to heal, or malunion, where the fractured bone heals in a deformed manner. One form of malunion is the malrotation of a bone, which is especially common after femoral and tibial fractures.
Complications of fractures may be classified into three broad groups, depending upon their time of occurrence.
These are as follows –
- Immediate complications – occur at the time of the fracture.
- Early complications – occur in the initial few days after the fracture.
- Late complications – occur a long time after the fracture.
Diagnosis
A doctor will carry out a physiotherapy examination, identify signs and symptoms, and make a diagnosis.
The patient will be interviewed – or friends, relatives, and witnesses if the patient cannot communicate properly – and asked about circumstances that caused the injury or may have caused it.
Doctors will often order an X-ray. In some cases, an MRI or CT scan may also be ordered.
Bone healing is a natural process that, in most cases, will occur automatically. Fracture treatment is usually aimed at making sure there is the best possible function of the injured part after healing.
Treatment also focuses on providing the injured bone with the best circumstances for optimum healing (immobilization).
For the natural healing process to begin, the ends of the broken bone need to be lined up – this is known as reducing the fracture.
The patient is usually asleep under a general anesthetic when fracture reduction is done. Fracture reduction may be done by manipulation, closed reduction (pulling the bone fragments), or surgery.
Immobilization – as soon as the bones are aligned they must stay aligned while they heal. This may include:
Plaster casts or plastic functional braces – hold the bone in position until it has healed.
Metal plates and screws – current procedures may use minimally invasive techniques.
Intra-medullary nails – internal metal rods are placed down the center of long bones. Flexible wires may be used in children.
External fixators – these may be made of metal or carbon fiber; they have steel pins that go into the bone directly through the skin. They are a type of scaffolding outside the body.
Usually, the fractured bone area is immobilized for 2-8 weeks. The duration depends on which bone is affected and whether there are any complications, such as a blood supply problem or an infection.
Healing – if a broken bone has been aligned properly and kept immobile, the healing process is usually straightforward.

Osteoclasts (bone cells) absorb old and damaged bone while osteoblasts (other bone cells) are used to create new bone.
A callus is a new bone that forms around a fracture. It forms on either side of the fracture and grows toward each end until the fracture gap is filled. Eventually, the excess bone smooths off and the bone is as it was before.
The patient’s age, which bone is affected, the type of fracture, as well as the patient’s general health, are all factors that influence how rapidly the bone heals. If the patient smokes regularly, the healing process will take longer.
Physiotherapy treatment
Physiotherapy is an effective treatment for fractures and dislocations. Fractures are a result of excessive force applied to a bone resulting in complete or incomplete breaks.
- Relieve pain
- Reduce muscle weakness, and atrophy
- Improve range of motion and mobility
- Strengthen surrounding tissue and muscle
after the bone has healed, it may be necessary to restore muscle strength as well as mobility to the affected area. If the fracture occurred near or through a joint, there is a risk of permanent stiffness or arthritis – the individual may not be able to bend that joint as well as before. Surgery – if there was damage to the skin and soft tissue around the affected bone or joint, plastic surgery may be required.
Delayed unions and non-unions
Non-unions are fractures that fail to heal, while delayed unions are those that take longer to heal.
Ultrasound therapy – low-intensity ultrasound is applied to the affected area daily. This has been found to help the fracture heal. Studies in this area are still ongoing.
Bone graft – if the fracture does not heal, a natural or synthetic bone is transplanted to stimulate the broken bone.
Stem cell therapy – studies are currently underway to see whether stem cells can be used to treat fractures that do not heal.
The physiotherapist’s role is to identify the cause of the problem and select the appropriate procedure to alleviate or eliminate the cause of the loss of movement.
Doing an assessment for the patient is necessary also doing The problem-oriented medical record (POMR) system ( is based on a data collection system that incorporates the acronym SOAP:
• Subjective – any information is given to you by the patient: allergies, past medical history, past surgical history, family history, social history (living arrangements, social conditions, employment, medication), review of systems
• Objective – all information obtained through observation or testing, e.g. range of joint movement, muscle strength.
• Analysis – a listing of problems based on what you know from a review of subjective and objective data.
• Plan – this refers to the plan of treatment ).
Also By Using specific exercises, the aim is to reduce any swelling, regain full muscle power and joint movement, and to bring back full function.
The treatment will depend very much on the problems identified during your initial assessment, but may include a mixture of the following:
• Soft tissue massage, particularly to manage Edema and swelling
• Scar management if the patient had surgery to fix the fracture
• Ice therapy
• Stretching exercises to regain joint range of movement
• Joint manual therapy and mobilizations to assist in regaining joint mobility
• Structured and progressive strengthening regime
• Balance and control work and gait (walking) re-education where appropriate
• Taping to support the injured area/help with swelling management
• Return to sport preparatory work and advice where required




6 Comments