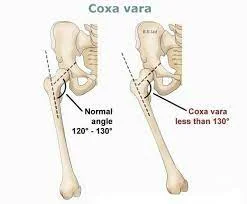
Coxa vara
Table of Contents
What is a Coxa Vara?
- Coxa vara is an abnormality of the hip, in which the angle joining the head and the shaft of the femur is decreased to less than 120 (one-twenty) degrees. This outcome in the leg being shortened and the evaluation of a limp.
- It is commonly caused by injury, like a fracture. It can occur when the bone tissue in the neck of the femur is smoother than normal, causing it to bend under the weight of the body. This may either be congenital or the outcome of a bone disorder.
- The most usual cause of coxa vara is either congenital or evaluated. Other usual causes include metabolic bone diseases (e.g. Paget’s disorder of bone), post-Perthes abnormality, and post-traumatic (because of inappropriate healing of a fracture joining the greater and lesser trochanter). Shepherd’s Crook deformity is a serious form of coxa vara here the proximal femur is severely deformed with a reduction in the neck shaft angle beyond 90 (ninety) degrees.
- It is most usually the sequela of osteogenesis imperfecta, Paget’s disease, osteomyelitis, tumor, and tumor-like states (e.g. fibrous dysplasia).
- Coxa vara can occur in cleidocranial dysostosis.
Anatomy and coxa vara
- In early skeletal development, a usual physis serves the greater trochanter and the capital femoral epiphysis. This physis splits as extends and continues in a stable that is acceptable to the capital epiphysis and creates a typical neck-shaft angle (angle joining the femoral shaft and the neck).
- The equal angle at ability is 135 ± 7 degrees. Another angle utilized for the measurement of coxa vara is the cervicofemoral angle which is approximately 35 degrees at infancy and improves to 45 degrees after maturity.
Type Of Coxa Vara
- Developmental,
- congenital (e.g. congenital short femur, PFFD),
- acquired (e.g. SCFE, infection, Perthes),
- dysplasia (e.g OI, Jansen, Schmid, SED),
- cretinism.
Developmental Stages
- More usual cause: primary defect in endochondral ossification of the medial area of the femoral neck.
- Excessive intrauterine pressure on the evolving fetal hip.
- vascular insult.
- Faulty maturation of the cartilage or metaphyseal bone of the femoral neck.
Clinical feature in Congenital Coxa Vara
- presents later the child has begun walking but before six years of age. Commonly associated with a painless hip because of mild abductor weakness and mild limb length discrepancy.
- If there is the bilateral involvement the child might have the waddling gait or Trendelenburg gait with an increased lumbar lordosis. The greater trochanter is commonly prominent on palpation and is more proximal. Restricted abduction or internal rotation.
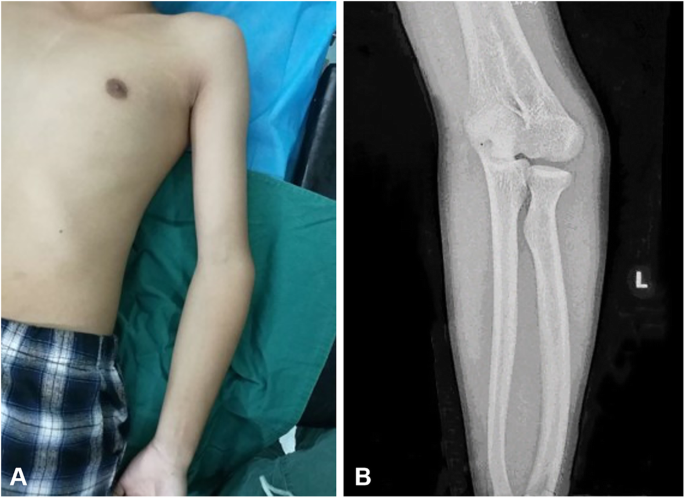
X-ray
- Decreased neck shaft angle, improved cervicofemoral angle, vertical physis, shortened femoral neck decrease in femoral anteversion. HE angle (hilgenriener epiphyseal angle- angle subtended joins a horizontal line connecting the triradiate cartilage and the epiphysis normal angle is <30 degrees.
- Treatment: HE angle (hilgenriener epiphyseal angle) of 45–60 degrees observation and periodic follow-up.
- Indication for surgery: HE angle (hilgenriener epiphyseal angle) more than 60 degrees, progressive deformity, neck-shaft angle <90 degrees, development of Trendelenburg gait.
- Surgery: subtrochanteric valgus osteotomy with adequate internal rotation of distal fragment to correct anteversion usual complication is recurrence. If the HE angle (hilgenriener epiphyseal angle) is reduced to 38 degrees less evidence of recurrence post-operative spica cast is used for a period of 6–8 weeks.
- Coxa vara is seen in Niemann–Pick disease.
Congenital coxa vara
- Presence at birth is extremely infrequent and associated with other congenital anomalies such as proximal femoral focal deficiency, fibular hemimelia, or anomalies in another area of the body such as cleidocranial dysostosis. The femoral deformity is present in the subtrochanteric part where the bone is bent. The cortices are thickened and may be related to overlying skin dimples.
- External rotation of the femur with a valgus abnormality of the knee may be noted. This condition does not resolve and needs surgical management. Surgical management involves valgus osteotomy to improve hip biomechanics and length and rotational osteotomy to right retroversion and length.
Treatment
Non-operative Treatment
Indications OF Treatment
- Hilgenreiner-ephyseal (HE) angle (normal <25 degrees),
- <45 degrees – unlikely to progress,
- 45-60 – may progress,
- will require close follow-up if non-symptomatic.
Operative Treatment (Surgical)
Corrective valgus derotation osteotomy (VDRO)
Indications For surgery :
- Hilgenreiner’s physeal angle > 60°,
- Hilgenreiner’s physeal angle between 45-60° if symptomatic (e.g. limp & progression of varus),
- progressive decrease in neck-shaft angle < 110 °,
- aftercare,
- hip-spica or abduction pillow x 4-6 weeks depending on fixation and healing.
Indications for surgical intervention are :
- Neck–shaft angle < 90 degrees, Progressive deformity, Vertical physis, and a significant limb length discrepancy, HE angle> 60 degrees.
Physiotherapy treatment
- Literature is lacking, yet surgical management ss to seems the accepted treatment protocol for this condition.
Summary
- Due to the decreased incidence of coxa vara and even lower for the coxa valga, there is little literature latest available. There are three types of Coxa Vara, acquired, congenital, and developmental, usually displaying greater acetabular dysplasia or the abnormal acetabulum. Surgery is the most essential treatment protocol. In the case of acquiring this abnormality from a fracture, the proximal femur and femoral neck require accurate reduction and rigid fixation to avoid potentially serious complications.
FAQs
Coxa vara is a hip abnormality in which the femoral neck-shaft angle decreases under its normal value. The standard surgical treatment for this condition is a curative valgus osteotomy.
Coxa vara commonly attendings with a limp, a leg length difference (LLD), or a limited ability to bring the thigh out to the side. X-rays are utilized to diagnose coxa vara. Depending on what causes the condition or how serious the abnormality is, reconstructive surgery may be needed to improve the hip alignment or biomechanics.
Individuals may present with small limbs and/or small trunks. Radiographic features involve enlargement and corner fracture-such as lesions of the metaphyses, developmental coxa vara, shortened long bones, scoliosis, and vertebral anomalies. Limited joint mobility and chronic pain are usual.
Coxa vara deformity is well cured by anatomic reduction and rigid internal fixation followed by external immobilization in most cases. To lessen the risk of premature epiphyseal closure and subsequent abnormality, internal fixation devices should avoid the growth plate as long as a good screw purchase can be achieved.
The condition is sometimes not apparent until a child is 2 or 3 years old. It is infrequent for coxa vara to be present at birth and in these cases, it is commonly associated with other conditions, such as proximal focal femoral deficiency (PFFD), fibular hemimelia, or other congenital problems.
Patients who have congenital coxa vara (CCV) commonly present with gait abnormalities. Affected children are commonly present between the time they begin ambulation and the age of six years. In most patients, the gait deformity is progressive and, notably, pain-free.