Peroneal Nerve Palsy:
The common peroneal nerve is a major nerve that supplies the lower limb. The common peroneal nerve is the smaller and terminal branch of the sciatic nerve which is composed of the posterior divisions of L4, L5, S1, and S2. Peroneal nerve palsy is a paralysis of a common fibular nerve that decrease the patient’s ability to lift the foot at the ankle. The common peroneal nerve gives the sensation to the front and sides of the legs and the top of the feet. Nerve also controls the muscles that lift the ankle and toes upward.
Common peroneal nerve dysfunction leads to loss of movement, decreased sensation, pain, and tingling in the foot and leg. This condition is also known as fibular nerve dysfunction. Due to the injury of the nerve, the gait pattern is changed so that time foot drop is developed.
There are traumatic and non-traumatic causes of peroneal nerve injuries, including knee dislocation, direct impact or cut on the fibular neck, fracture of the proximal fibula, compression by use of a tight plaster cast, or compression wrapping, bed rest for a long period, and regular crossing of the legs. It is typically managed conservatively with orthotics or physical therapy—the surgical options in more severe cases. In most cases, 30% of peroneal nerve palsy occurs due to knee dislocations.
Table of Contents
Anatomy of common peroneal nerve:
The common peroneal nerve referred to as the common fibular nerve also is a major nerve that supplies the lower extremity. It starts from the L4 to S2 nerve roots of the spinal cord and is a major branch of the sciatic nerve. the common peroneal nerve leave from the sciatic nerve in the distal posterior thigh near the popliteal fossa.
After that, it continues down the thigh, running posteroinferior to the biceps femoris muscle, then cross laterally to the head of the lateral gastrocnemius muscle through the posterior intermuscular septum. The nerve is palpated behind the head of the fibula and it round around the neck of the fibula. The common peroneal nerve gives articular branches to the knee and superior tibiofibular joint.
The lateral cutaneous nerve of the calf supplies the posterolateral side of the proximal two-thirds of the leg. The communicating branch of the nerve joins the sural nerve in the middle third of the leg.
The two branches are the superficial peroneal nerve (SPN) and the deep peroneal nerve (DPN).
The superficial peroneal nerve(SPN) supplies the lateral compartment of the leg, and the deep peroneal nerve(DPN) supplies the anterior part of the leg and the dorsum of the foot. These two nerves give the eversion and dorsiflexion movement of the foot. The nerve provides both motor and sensory functions.
Nerve Roots: L4, L5, S1, S2.
Branches of Common fibular nerve:
In the popliteal fossa, the common peroneal nerve gives off:
- The Genicular branches to the knee joint.
- The Lateral cutaneous nerve of the calf.
- A sural communicating branch.
The two terminal branches include:
- Superficial peroneal nerve (L5, S1, S2).
- Deep peroneal nerve (L4, L5, S1, S2).
The superficial branch supplies the lateral compartment muscles of the leg. it also supplies the skin over the lateral lower two-thirds of the leg and the whole of the dorsum part of the foot except the area between the 1st and 2nd toes, that supplied by the deep peroneal nerve.
The deep branch supplies the anterior compartment of the leg and the dorsum of the foot of the ankle. It supplies all of the muscles of the anterior compartment and also gives a cutaneous supply to the webspace of 1st and 2nd toes of the foot.
Muscles supplied by the SPN:
Motor branch:
- Lateral compartment
- Peroneus longus
- Peroneus Brevis
Sensory branch:
- Anterolateral leg
Muscle supplied by the DPN:
- Anterior compartment of leg muscles:
- Tibialis anterior
- Extensor hallucis longus
- Extensor digitorum longus
- Peroneus Tertius
Sensory:
- First dorsal webspace
The function of the peroneal nerve:
Motor: supply the short head of the biceps femoris, lateral and anterior compartments of the leg.
Sensory: supply the skin over the upper lateral and lower posterolateral leg. Also cutaneous supply to the skin of the anterolateral leg, and the dorsum of the foot.
Motor Functions:
The Biceps femoris muscle is responsible for the flexion at the knee.
Also, its terminal branches supply to the muscles:
- Superficial fibular nerve: Supply the muscles of the lateral compartment of the leg; fibularis longus and brevis. These muscles give the foot eversion movement.
- Deep fibular nerve: Supply the tibialis anterior, Extensor Digitorum Longus, and extensor hallucis longus muscles of the anterior compartment of the leg. These muscles respond to the dorsiflexion movement of the foot, and extension of the digits. It also supplies some intrinsic muscles of the foot.
If the common fibular nerve is injured, the patient can’t able to dorsiflexion, eversion of the foot, and extend the digits.
Sensory Functions:
Two cutaneous branches directly arise from the common fibular nerve as it runs over the lateral head of the gastrocnemius.
- Sural communicating nerve: It is combined with a tibial nerve branch to form the sural nerve. The sural nerve supplies the skin over the lower posterolateral leg.
- Lateral sural cutaneous nerve: Supply the skin of the upper lateral leg.
Also, the terminal branches of the common fibular nerve have a cutaneous function:
- Superficial fibular nerve: Supply the skin of the anterolateral leg, and dorsum of the foot.
- Deep fibular nerve: Supply the skin between the first and second toes.
What is Peroneal Nerve Palsy?
It is the most common entrapment neuropathy of the lower extremity. It happens due to the injury of the common peroneal nerve. Paralysis of the peroneal nerve results the movement and sensation loss in the foot and leg. This condition is also called common fibular nerve dysfunction and is also known as a foot drop deformity.
Signs and symptoms of peroneal nerve palsy:
- Diminished the sensation, numbness, and tingling in the upper part of the foot or the outer part of the upper or lower leg.
- Foot drops.
- Toes drag while walking.
- Weakness of the ankles or feet.
- Prickling sensation.
- Pain in the tibial shin.
- Pins and needles sensation.
- Slapping gait.
- Neuropathic pain is a common symptom of peroneal nerve neuropathy which can be managed with analgesia.
Causes of peroneal nerve palsy:
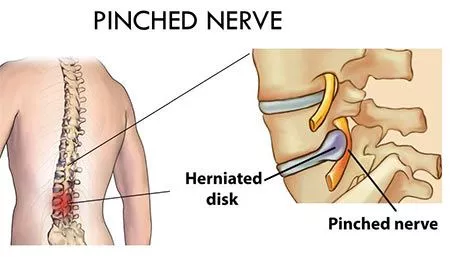
Factors that affect the cause of peroneal nerve palsy are musculoskeletal or peroneal nerve injuries. Commonly paralysis occurs at the outside of the leg and the top of the foot. Paralysis occurs due to decreased muscle strength to lift the foot, twist the ankle outside, and move the toes around. Injury to the nerve disruption to the myelin sheath it covers the axon (branch of the nerve cell). The axon also is injured, which is a more severe injury that causes similar symptoms of this.
The most cause of nerve injury is the dislocation of the knee. Other possible causes are metabolic dysfunction of the lower part of the knee or effects on the orientation of the hip or pelvis. Present a loss of feeling, muscle control, muscle tone, and eventual loss of muscle mass because the nerves aren’t responding to the muscles after they are injured. Dysfunction of a single nerve like the common peroneal nerve dysfunction is called mononeuropathy(Affects only one area).
Common causes of injury to the peroneal nerve following:
- Trauma or injury to the knee.
- Fracture of the fibula (Lower leg bone)
- The tight plaster cast was used on the lower leg.
- Crossing the legs regularly
- Wearing high boots regularly.
- Pressure on the knee from positions of deep sleep or coma.
- Long time bedridden patient.
- Broken to the leg bone.
Some neurologic conditions can cause symptoms similar to peroneal nerve injuries, the following:
- Amyotrophic lateral sclerosis(ALS)
- Multiple sclerosis
- Parkinson’s disease
- Herniated lumbar disk.
Many systemic diseases can cause compressive peroneal neuropathy and injury to the common peroneal nerve, the following:
- Diabetes mellitus
- Inflammatory disease
- Motor neuron diseases
- Anorexia nervosa is due to the loss of subcutaneous fat at this level causing compression of the nerve.
Common peroneal nerve injury is seen in which people?
Very thin persons.
Who have some autoimmune conditions, like polyarteritis nodosa.
Who has nerve injury due to other medical problems, suppose having diabetes or use of alcohol.
Who has Charcot-Marie-Tooth disease, is an inherited disorder that affects the nerves.
Epidemiology of peroneal nerve palsy:
Common peroneal neuropathy is the most common mononeuropathy seen in the lower limbs. Traumatic injuries to the common peroneal nerve (CPN) most commonly affect young athletic patients (like football, or soccer). Adult patients following high energy trauma (Like, motor vehicle collisions (MVCs)), with CPN injury occurring in 16 to 40% of patients with knee dislocations. Low-energy trauma knee dislocations can occur in obese patients during their daily living activities.
Diagnosis of peroneal nerve palsy:
The partial nerve paralysis, more than 80% of patients will completely recover and for complete nerve paralysis, less than 40% of patients will completely recover.
The doctor will do a physical examination, which may show:
- Loss of muscle control in the lower legs and feet.
- Muscle atrophy (thinning or loss of the foot or foreleg muscles).
- Difficulty in ankle-toe movement.
Examinations are required for the following reasons:
- Considering lumbar radiculopathy during the examination.
- Foot drop deformity.
- Sensations are decreased which may be difficult to determine because of the variable and a small autonomous zone of sensation.
- Tinel’s sign is present over the fibular neck so localized nerve compression is present.
Tests of nerve activity following:
- Electromyography (EMG) test for checking electrical activity in muscles.
- Nerve conduction tests(NCV).
- Magnetic resonance imaging (MRI).
- Nerve ultrasound.
Other tests may be done depending on the suspected cause of nerve dysfunction. Tests are blood tests, x-rays, etc.
Electromyography:
Electromyography is used to check the peroneal nerve palsy within one month of injuries. if it is partial paralysis, patients have more chance to recover completely from the palsy. More than 70 to 80 % of patients with partial paralysis recovered completely, but if the complete paralysis is done so the chances are less than 30% to recover completely. If the symptoms do not subside in a few months, so nerve decompression surgery is required.
Nerve conduction velocity:
It measures the speed at which an electrochemical impulse propagates down a neural pathway. Conduction velocities are affected by different factors including age, sex, and other medical conditions. In the nerve conduction velocity, surface electrodes are placed onto the skin over the nerves at different areas. Each patch sends electrical impulses which stimulate the nerve and the electrical activity of the nerve is recorded by the other electrode.
MRI:
This MRI (magnetic resonance imaging) scan uses powerful magnets and radio waves to take pictures of the body, and no radiation is used. The MRI test detects the location and condition of the injured peroneal nerve.
A common peroneal nerve stress test (SLUMP test) reproduction of the patient’s symptoms.
The symptoms meet the 3 criteria for positive neural tension:
- Side-to-side difference.
- Reproduction of the patient’s symptoms.
- Changes with a distant component.
- reproduce the patient’s symptoms.
- changes with a distant component.
- The peroneal nerve tension test (A variation of the SLR where the ankle is plantarflexed and inverted at the point of first resistance) may reproduce symptoms.
- Tinel’s sign (palpation or tapping of the nerve) around the fibular head may also reproduce symptoms.
- Heel walking serves as a quick, gross screen of the deep peroneal nerve (dorsiflexion, L4, L5).
- Toe walking serves as a quick, gross screen of the tibial nerve (S1-2) and superficial peroneal nerve (L5, S1).
- Manual muscle tests may further reveal the weakness of the peroneus longus, peroneus brevis, peroneus tertius, tibialis anterior, extensor digitorum longus and brevis, and extensor hallucis longus and brevis. During gait examination, the therapist may notice foot drop, a “slapping” gait.
Prevention of peroneal nerve palsy:
- Avoid the long-term pressure on the back or side of the knee. Cure injuries to the leg or knee right away. Take a loose plaster cast or splint not too much tight over the leg.
- Avoid crossing your legs.
- Moving actively and frequently.
- Wear a knee brace during work.
Differential diagnosis of peroneal nerve palsy:
- Any tendon injury which is supplied by the peroneal nerve.
- Other compressive neuropathies:
- Tarsal tunnel syndrome.
- Anterior tarsal tunnel syndrome.
- Nonspecific tendinitis affecting lower limb muscles/tendons.
- Chronic ankle pain.
Complications of the peroneal nerve palsy:
- Reduce ability to walk.
- Decrease sensation in the legs or feet.
- Weakness or paralysis in the whole leg.
- Complications arise due to the Side effects of medicines.
Treatment of peroneal nerve palsy:
This treatment aims to improve mobility or movement and independence.
Medical treatment:
- Corticosteroid injection is given to reduce swelling and decrease pressure on the nerve.
- The doctor prescribed pain relieving medicine to control the pain.
- Other drugs are Gabapentin, Carbamazepine, and Tricyclic antidepressants, such as amitriptyline
- Orthopedic devices may improve the walking pattern and prevent muscle contractures. devices like; Braces, splints, Orthopedic shoes, and other equipment.
- A vocational counseling session was arranged.
- occupational therapy.
Ankle foot orthosis: An ankle-foot orthotic (AFO) is used for foot drop deformity. This orthosis is given the toe dorsiflexion during the swing phase, medial or lateral stability of the ankle during the stance, and, if needed some push-off stimulation provide during the stance phase.
Surgical treatment:
Surgery may help decrease the symptoms in critical cases.
The goal of surgery:
- To remove pressure on the nerve if the condition arises due to the pressure on the nerve.
- To remove tumors that press on the nerve.
The doctor may suggest the surgery if:
- The deformity was not correct. Rapidly deteriorating lesion and no sign of improvement within three months.
- The patient has problems with movement.
- If the nerve axons are damaged.
The Different types of surgery:
- Decompression surgery.
- Nerve repair.
- Nerve grafting.
- Nerve transfer.
- Tendon transfer.
Physiotherapy Treatment for common peroneal nerve palsy or foot drop:
The goal of physiotherapy:
- Correct or stop to worsen the condition.
- Reducing the pain.
- Improve ankle mobility.
- The patient can walk.
- Reduce the edema,
- Maintain or increase the strength and endurance of the unaffected leg.
Treatments:
- Ankle mobility exercise
- Active assisted movement of ankle dorsiflexion.
- Stretching of the calf muscle, hamstring muscle, and gastrocnemius soleus muscle.
- Strengthening exercises for ankle movement.
- mobilization techique.
- Heat and Cold therapy.
- Electric stimulation.
- Ultrasound.
- Iontophoresis.
- The ankle-foot orthosis is advised.
- Gait(Walking) training.
- Taping technique.
- Improve proprioception.
Electrical stimulation:
- Electrical Stimulation is given in mainly two ways: Surge Faradic (SF) And Inter-mittens Galvanic(IG) Current.
- RD Test is required according to which one will be given IG or SF.
- If RD Test is positive, IG current is given on the muscle, and in progress, SF current is given to improve the muscle strength. The progression of the nerve is checked by the curve.
- IG Current Maintain Muscle property and decrease the Wasting of muscle.
- SF Current strengthens the muscle and stimulates the muscle.
- Mainly Electrical stimulation is given over the tibialis anterior muscle and other dorsiflexor muscles.
Heat and Cold therapy:
First, check the patient’s sensation according to the result apply a Heating pad or an ice cube (ice pack) over the ankle to reduce the pain and decrease the swelling of the foot or ankle. caring for the patient skin that does not too much burn.
Iontophoresis:
Iontophoresis has suggested the relief of pain in peroneal neuropathy or peroneal nerve palsy. In this, ionic medications are given to the soft tissue with the use of an electrical current.
Ankle mobility exercise:
- If the patient cant does the ankle eversion, and inversion movement actively so the patient does the ankle movement on the inner side (inversion movement), and ankle movement outside(eversion movement) passively by the therapist.
- If some degree of movement is present in the ankle so does that movement actively assisted by the therapist.
- In this condition, ankle dorsiflexion movement is not present. so therapists do first passively the dorsiflexion movement. once the patient does half range of movement actively given the active assisted movement and then the patient does active movement in the normal range.
- After that therapist goes for strengthening exercises of the ankle.
Isometric exercises for the ankle:
Isometrics for eversion movement:
- Pushing the ankle outward.
- When seated on the chair, place the foot outside of the table or close to the door.
- Push outward the foot against the table. This will make your muscles contract. The ankle joint should not move.
- Hold this position for 15 seconds then relax. again it repeats this way 5 to 10 times.
Isometrics of inversion:
- This exercise focuses on inversion movement, which involves pushing the ankle inward.
- While seated, place the foot inside of the table leg or closed door.
- Push inward with the foot into the table. That will make the contraction of muscles. Your ankle joint should not move.
- Hold it for 15 seconds and then relax. Repeat it 5 to 10 times.
Resisted strengthening exercise for ankle:
This exercise will perform with a theraband for resistance ankle strengthening exercises. It will help strengthen the muscles around the ankle and give support to the joint.
Resisted Strengthening Dorsiflexion:
- Didn’t tie a theraband or any other around the foot, ankle, or leg because that would restrict blood flow.
- This resistance exercise helps strengthen the anterior tibialis muscle of the leg.
- Fix the band around a table leg. Put the foot inside the band, with the band across the top of the foot.
- Move only the ankle, keep the knee straight and foot move backward or towards the body.
- Hold this position for 2 seconds and then release slowly.
- Back to the neutral position. Repeat it 10 times.
Resisted Strengthening Inversion:
- Tie the theraband under the foot and hold the theraband ends in your hands.
- Move only the ankle and keep toes pointed up, turn the foot inward so the sole is facing another leg.
- Hold it for 2 seconds.
- Back to the neutral position.
Resisted Strengthening Eversion:
- Tie the theraband under the foot and hold the theraband ends in your hands.
- Move only the ankle and keep the toes pointed up, turn the foot outward direction, away from another leg.
- Hold it for 2 seconds.
- Back to the normal position.
Ankle foot orthosis:
An ankle-foot orthotic (AFO) is used for foot drop deformity. This orthosis is given the toe dorsiflexion during the swing phase, medial or lateral stability of the ankle during stance, and, if needed some push-off stimulation provide during the stance phase.
Towel Stretch (Calf muscle stretch):
Sit on the floor or bed, both legs straight out in front of you. Tie a towel or exercise band around the affected foot. Pull the towel or band towards the body with the hand. Hold for 30 seconds. Then relax and Repeat 3 times.
Toe to Heel Rocks:
- Stand in front of the wall and take support with your hands. shift the weight forward and stand up on the toes. Hold this position for 5 seconds.
- Shift the weight backward onto the heels and lift the toes off the ground. Hold for 5 seconds. Repeat it 10 times.
Marble Pickup (curling of toe):
The patient sits in a chair and both feet are placed on the floor. Place 20 marbles on the floor in front of you. Using the affected toe of the foot, pick up each marble and put it into the bowl. Complete the task with pick up the all marbles.
Kinesio Tapping Technique:
Kinesio taping is given the fast improvement of walking in foot drop patients.
Gait training:
- Gait means the way a person walks. A gait abnormality means a deviation in the walking pattern from normal walking.
- Gait training is given to those who have a significant walking problem. This treatment helps the patient walk more efficiently and improves stability through different strength and balance exercises.
- In this condition, during gait training requires walkers, canes, and parallel bars for the safety of the patient.
- A gait belt is an assistive device that is used to help the patient to maintain balance during walking.
FAQ:
What are the symptoms of peroneal nerve damage?
Decreased sensation, numbness or tingling in the foot or outer part of the legs, muscular weakness of the ankle or feet, walking difficulty, foot drop, a “slapping” gait, toes dragging while walking, neuropathic pain present in the limb.
What are the treatments for peroneal nerve palsy?
mainly the medical treatment and physiotherapy treatment cure this condition but if the condition not cures and become worsens so surgical treatment is necessary. In medical treatment the advised pain-relieving medicines and corticosteroids injection. Occupational therapy is also used in this condition. The physiotherapy treatment improves ankle mobility, strengthens the ankle muscles, and corrects the walking pattern and other different exercises are advised. In surgical treatment nerve grafting or nerve repair surgery is advised it depends on the patient’s condition.
What is Peroneal Nerve Palsy?
It is the most common entrapment neuropathy of the lower extremity. It happens due to the injury of the common peroneal nerve. Paralysis of the peroneal nerve results the movement and sensation loss in the foot and leg. This condition is also called common fibular nerve dysfunction and is also known as a foot drop deformity.
What are the preventions for peroneal nerve palsy?
1. Patients avoid long-term pressure on the back or side of the knee. Cure injuries to the leg or knee right away.
2. Take a loose plaster cast or splint not too much tight over the leg.
3. Avoid crossing your legs.
4. Moving actively and frequently.
5. Wear a knee brace during work.What are the functions of the common peroneal nerve?
Motor Functions:
The Biceps femoris muscle is responsible for the flexion at the knee.
Also, its terminal branches supply to the muscles:
Superficial fibular nerve: Supply the muscles of the lateral compartment of the leg; fibularis longus and brevis. These muscles give the foot eversion movement.
Deep fibular nerve: Supply the tibialis anterior, Extensor Digitorum Longus, and extensor hallucis longus muscles of the anterior compartment of the leg. These muscles respond to the dorsiflexion movement of the foot, and the extension of the digits. It also supplies some intrinsic muscles of the foot.
If the common fibular nerve is injured, the patient can’t able to dorsiflexion, eversion of the foot, and extend the digits.
Sensory Functions:
Two cutaneous branches directly arise from the common fibular nerve as it runs over the lateral head of the gastrocnemius. Gives the sensation to that particular muscle.
• Sural communicating nerve: It is combined with the tibial nerve branch to form the sural nerve. The sural nerve supplies the skin over the lower posterolateral leg.
• Lateral sural cutaneous nerve: Supply the skin of the upper lateral leg.
Also, the terminal branches of the common fibular nerve have a cutaneous function:
Superficial fibular nerve: Supply the skin of the anterolateral leg, and dorsum of the foot.
Deep fibular nerve: Supply the skin between the first and second toes.