Facial Palsy
Table of Contents
What is Facial palsy?
The term facial palsy generally refers to weakness of the facial muscles, inability to move the muscles of the face, innervated by the facial nerve, one of the cranial nerves, mainly resulting from temporary or permanent damage to the facial nerve.
When the facial nerve is missing or not working properly, the muscles in the face do not receive the necessary signals in order to function properly. This results in paralysis of the affected part of the face, which can affect the movement of the eye and/or the mouth, as well as other areas. It can be categorized into two types based on the location of the casual pathology:
- Central facial palsy: Due to damage above the facial nucleus
- Peripheral facial palsy: Due to damage below the facial nucleus, there are different degrees of facial paralysis
Facial palsy can affect one or both sides of the face, with noticeable drooping of the mouth and problems with speaking, swallowing saliva, eating, blinking, or communicating through natural facial expressions.
What is the facial nerve?
The facial nerve is the VII of XII cranial nerves in the nervous system. We have two facial nerves, one on each side of the face.
The facial nerve is a pathway from the brain to specific muscles in the face. It controls muscles that help make expressions like raising an eyebrow, smiling, or frowning and functions in conveying taste sensations from the anterior two-thirds of the tongue.
The facial nerve supplies preganglionic parasympathetic fibers to respective head and neck ganglia.
And the facial and intermediate nerves can be collectively referred to as the nervus intermediofacialis.
The motor part of the facial nerve arises from the nucleus in the pons, while the sensory and parasympathetic parts arise from the intermediate nerve.
Nucleus
The cells for the facial nerve are grouped in the areas called nuclei or ganglia. The cell bodies for the afferent nerves are found in the geniculate ganglion for the taste sensation.
The cell bodies for muscular efferent nerves are found in the facial motor nucleus on the other hand the cell bodies for the parasympathetic efferent nerves are found in the superior salivatory nucleus.
Course
The facial nerve arises from the brainstem from an area posterior to the cranial nerve VI (abducens nerve) and anterior to cranial nerve VIII (vestibulocochlear nerve).
The facial nerve typically travels from the pons runs through the temporal bone and exits through the stylomastoid foramen after which it divides into terminal branches at the posterior edge of the parotid gland, a major salivary gland.
Branches
Intracranial branches
The greater petrosal nerve arises from the superior salivatory nucleus of the pons. It provides parasympathetic innervation to several glands, including the nasal glands, the palatine glands, the lacrimal gland, and the pharyngeal gland.
It also provides parasympathetic innervation to the maxillary sinus, frontal sinus, sphenoid sinus, ethmoid sinus, and nasal cavity. This also includes taste fibers for the palate via the lesser palatine nerve and greater palatine nerve.
The communicating branch to the otic ganglion arises from the geniculate ganglion and joins the lesser petrosal nerve to reach the otic ganglion.
The nerve to the stapedius provides motor innervation for the stapedius muscle in the middle ear
The chorda tympani provides parasympathetic innervation to the submandibular and sublingual glands, as well as special sensory taste fibers for the anterior two-thirds of the tongue.
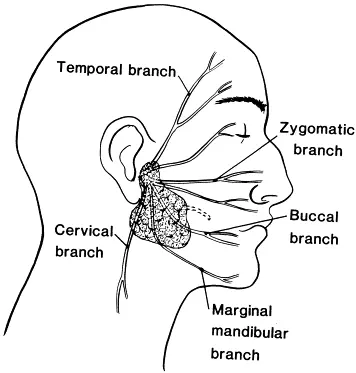
extracranial branches
Frontal (temporal): Controls your forehead muscles.
Zygomatic: Helps you close your eyes.
Buccal: This allows you to move your nose, blink, and raise your upper lip and corners of your mouth to make a smile.
Marginal mandibular: Draws your lower lip down (like a frown) and travels through your middle ear to help you respond to loud noises.
Cervical: Controls movement in your chin and lower corners of your mouth.
Function
The facial nerve performs motor and sensory functions:
Facial expression
The major function of the facial nerve is motor control of all of the muscles of facial expression. It also supplies the posterior belly of the digastric muscle, the stylohyoid muscle, and the stapedius muscle of the middle ear, it is a muscle in your inner ear that moderates the loudness of sound.
sensory
The facial nerve supplies taste sensations to the anterior two-thirds of the tongue via the chorda tympani. The taste sensation is sent to the gustatory portion of the solitary nucleus.
Another function of the facial nerve is, that it supplies parasympathetic fibers to the submandibular gland and sublingual glands via chorda tympani. The parasympathetic nerve supply serves to increase the flow of saliva. It also supplies to the nasal lacrimal gland and the nasal mucosa via the pterygopalatine ganglion.
Innervation
Temporal –this branch Innervates the frontalis, orbicularis oculi and corrugator supercilii.
Zygomatic –this branch Innervates the orbicularis oculi.
Buccal – this branch Innervates the orbicularis oris, buccinator, and zygomaticus.
Marginal mandibular –this branch Innervates the depressor labii inferioris, depressor anguli oris and mentalis.
Cervical –this branch Innervates the platysma.
The function of individual muscle
- Raising the eyebrows -frontalis
- Closing the eyes -orbicularis oculi
- Frowning -corrugator
- An open mouth smiling -zygomaticus
- A closed mouth smiling -risorius
- Pouting -orbicularis oris
- Lifting top lip -levator labii
- Pulling lower lip down -depressor labii
- Sticking bottom lip out -mentalis
- Pulling down of jaw and corners of mouth -platysma
- Wrinkling nose -procerus/nasalis
What are the causes of Facial Palsy?
Bell’s Palsy
A common cause of facial paralysis is bell’s palsy. It is idiopathic, although it has been associated with herpes simplex infection. Bell’s palsy may develop over several days and last several months, in the majority of cases recovering spontaneously.
Infection
Lyme infection is caused by Borrelia burgdorferi bacteria and is spread by ticks, which can lead to facial palsy in areas where Lyme disease is common. The first sign of about 80% of Lyme infections, typically one or two weeks after a tick a byte is usually an expanding rash accompanied by headaches, body aches, fatigue, or fever.
Reactivation of herpes zoster virus, as well as being associated with Bell’s palsy, also be a direct cause of facial palsy.
Reactivation of latent virus in the geniculate ganglion is associated with vesicles affecting the ear canal and termed Ramsay Hunt syndrome type II. Besides facial paralysis, symptoms may include ear pain and vesicles, vertigo, and sensorineural hearing loss.
Otitis media is an infection in the middle ear, which can spread to the facial nerve and inflame the nerve, causing compression of the nerve in its canal. Chronic otitis media usually presents in an ear with chronic hearing loss and discharge, with or without the ear pain. In the case of inflammation, the nerve is exposed to edema and subsequent high pressure, resulting in a peripheric type palsy.
Trauma
In blunt trauma, the facial nerve is the most commonly injured among the cranial nerves. Physical trauma mainly fractures of the temporal bone may also cause acute facial nerve paralysis. The possibility of facial palsy after trauma depends on the location.
Transverse fractures present the highest possibility of facial paralysis (40-50%). Patients may also come
with blood behind the tympanic membrane, sensory deafness, and vertigo; sensory deafness and vertigo occur due to damage to the vestibulocochlear nerve and the inner ear.
Longitudinal fracture in the vertical plane presents a lower likelihood of paralysis (20%). Patients may
present with blood coming out of the external auditory meatus), tympanic membrane tear, fracture of the external auditory canal, and conductive hearing loss.
Tumors
A tumor can compress the facial nerve anywhere along its complex pathway can result in facial paralysis. Common tumors are facial neuromas, congenital cholesteatomas, hemangiomas, acoustic neuromas, parotid gland neoplasms, or metastases of other tumors.
Often, since facial neoplasms have such a close relationship with the facial nerve, removing tumors in this part becomes
confound as the physician is unsure how to manage the tumor without causing even more palsy.
Patients with facial nerve paralysis resulting from tumors usually present with progressive, twitching paralysis, other neurological signs, or a recurrent Bell’s palsy.
Other neoplastic causes include leptomeningeal carcinomatosis.
Stroke
Central facial palsy can be caused by a lacunar infarct, which affects fibers in the internal capsule going to the nucleus. The facial nucleus can be affected by infarction of the pontine arteries. Unlike peripheral facial palsy, central facial palsy doesn’t involve the forehead, because the forehead is supplied by nerves coming from both motor cortexes.
Congenital
In very rare cases babies are born with congenital dysfunction of the facial nerve.
Other causes may include:
- Diabetes mellitus
- Sometimes bilateral facial nerve paralysis is a common manifestation of sarcoidosis of the nervous system, neurosarcoidosis.
- Melkersson-Rosenthal syndrome
- Millard-Gubler syndrome (ventral pontine syndrome)
An ipsilateral facial palsy with contralateral hemiplegia that involves the corticospinal tract and paralysis of the lateral rectus on - the ipsilateral side because of the involvement of the abducent nerve of the cranial nerve.
- Foville Syndrome (inferior medial pontine syndrome)
An ipsilateral facial palsy with contralateral hemiplegia and ipsilateral conjugate gaze effects
Eight-and-a-half syndrome
Facial paralysis with internuclear ophthalmoplegia and horizontal gaze palsy - Bilateral facial paralysis may occur in Guillain–Barré syndrome, which is an autoimmune disease of the peripheral nervous system.
- Moebius syndrome is a bilateral facial paralysis resulting from the underdevelopment of the facial nerve which is the VII cranial nerve, which is present at birth. The VI cranial nerve, the abducens nerve which controls lateral eye movement, is also affected, so people with Moebius syndrome cannot form facial expressions or move their eyes from side to side. Moebius syndrome is very rare, and its causes are not known.
- Facial piercings, like tongue piercings or eyebrow piercings, can cause damage to the facial nerve but it occurs in very rare cases.
- Multiple sclerosis
Syphilis
HIV
Vasculitides
What are the symptoms of Facial Palsy?
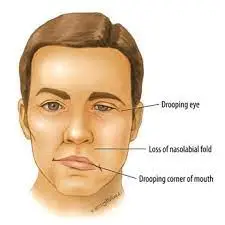
Facial nerve paralysis is characterized by facial weakness, usually only on one side of the face, with other symptoms possibly including loss of taste, movement, and many more.
Other signs may be connected to the cause of the paralysis, such as vesicles in the ear, which might occur if the facial palsy is due to shingles.
While facial paralysis takes place, it does not always mean that patient is having a stroke. The common diagnosis is in fact Bell’s palsy.
facial paralysis affects one side and rarely occurs on both sides.
- loss of blinking on the affected side
- a drop of the mouth on the affected side
- If nevertheless, the person is in synkinesis, the affected side of the mouth sits higher than the unaffected side. Facial synkinesis is defined as “it is abnormal facial movements that take place during spontaneous or volitional movement, for example, voluntary movement of the mouth might result in the closure of the eye”
- Ectropion – the lower eyelid may droop & turn outward
- slurred speech
- drooling
- pain in or behind the ear
- sound hypersensitivity on the affected side
- Difficulty eating and drinking because of the lack of lip seal which makes it difficult to keep fluids and food in the mouth
- Speech clarity is decreased as the “labial consonants” all require lip seal
- Dryness of the affected eye
- Somatic Effects
- Lack of tear production in the affected eye causes a dry eye, and the risk of corneal ulceration
- There are two factors that contribute to dry eye in facial nerve palsy: The greater petrosal nerve is derived from the facial nerve is affected; which supplies the parasympathetic autonomic component of the lacrimal gland and controls the production of the tears in the eyes
- The zygomatic branch of the facial nerve supplies orbicularis oculi, and the resulting paralysis leads to an inability to close the eye or blink. Thus, tears or artificial lubrication are not spread across the cornea properly
- Hyperacusis – i.e. sensitivity to sudden loud noises
- Altered taste sensation
- Painful eye with symptoms of irritation
- Sensitivity to light
- Appearance at rest of a flaccid facial palsy Illustration of left-sided flaccid facial palsy, position at rest. It shows the absence of horizontal forehead lines on the left, larger left eye, and lower resting position of the left corner of the mouth.
Stroke
People experiencing a stroke often experience the same symptoms as with Bell’s palsy. Nevertheless, a stroke usually causes additional symptoms which are not seen with Bell’s palsy. The following symptoms in addition to Bell’s palsy’s symptoms could indicate a stroke:
- changes in the level of consciousness
- confusion
- dizziness
- loss of coordination
- seizure
- changes in vision
- weakness in arms and legs on one side of the body
- Often people experiencing a stroke will still have the ability to blink & move their foreheads on the affected side. This is not possible with Bell’s palsy.
In the early stages of peripheral facial palsy, whatever the cause, the following differences between the two sides of the face will be apparent:
Mouth
- The corner of the mouth pulls down/droops
- Difficulty in speaking because of weakness
- Inability to smile on the affected side
- Inability to puff up cheeks or blow the air out
- Tingling in the affected half of the tongue
- Difficulty eating and drinking
- Difficulty brushing your teeth and spitting out
- Drooling from the weak corner of the mouth
- Excess or reduced salivation or dry mouth
- Inability to pout
Ear
- Pain in or near the affected ear
- Loss of hearing
- Increased sensitivity to high-pitched noise
Nose
- Nose runs or feels stuffy
- Inability to flare nostril
- Inability to wrinkle nose
- If a person develops symptoms of facial palsy slowly for about some weeks or months, then they should immediately be referred for further investigations.
Since it is sometimes hard to discriminate between a stroke and other causes of facial paralysis, it is a good idea to get a patient to a doctor quickly if you notice facial paralysis.
How is Facial Palsy classified?
Facial nerve palsy may be divided into supranuclear and infranuclear lesions. In a clinical setting, other commonly used classifications include acute, subacute, and chronic duration, based on degrees of nerve injury and intra-cranial and extra-cranial palsies.
- Supranuclear and nuclear lesions
Central facial palsy is caused by a lacunar infarct affecting fibers in the internal capsule going to the nucleus. The facial nucleus itself is affected by infarction of the pontine arteries. These are corticobulbar fibers traveling in the internal capsule. - Infranuclear lesions
These lesions refer to the majority of causes of facial palsy.
Differential diagnosis of Facial palsy:
Upper Motor Neuron versus Lower Motor Neuron
If the forehead is not affected and the patient is able to raise eyebrows then the facial palsy is likely to be an upper motor neuron lesion. Paralysis which covers the forehead, such that the patient is unable to raise the affected side eyebrow is a lower motor neuron lesion called bell’s palsy.
Nevertheless, caution is advised in using preservation of forehead movement to diagnose a central lesion. Patients may have to spare forehead function with lesions in the pontine facial nerve nucleus, some lesions in the temporal bone, or injury to the nerve in its distribution in the face. It is worth remembering that a cortical lesion that produces a lower facial palsy is usually associated with a motor deficit of the tongue and weakness of the fingers, thumb, or hand on the ipsilateral side.
another condition is:
- multiple sclerosis
- Ramsay hunt syndrome
- stroke
- tumor
What is the Diagnostic procedure for facial palsy?
A detailed medical history and physical examination, are the most important things for the diagnosis.
observation is The first step to checking which parts of the face do not move normally when the person tries to smile, blink, or raise eyebrows.
If the forehead wrinkle is normal, a diagnosis of central facial palsy is made, and the person should be evaluated for stroke. Otherwise, the diagnosis should be peripheral facial palsy, and if possible its cause needs to be identified.
Electromyography is to check the health of the muscles and the nerves.
Many conditions cause facial palsy proper tests can differentiate them. Ramsey Hunt’s syndrome causes pain and small blisters in the ear on the same side as the facial palsy, Otitis media or, trauma may alternatively become apparent from history and physical examination. If there is a history of trauma, or a tumor is suspected, a CT scan or MRI may be used to clarify the impact.
Blood tests, including blood sugar, CBC, Lyme test, or x-rays may be ordered depending on suspected causes. The possibility that the facial palsy is caused by Lyme disease should be estimated, based on the recent history of outdoor activities in likely tick habitats during warmer months, the recent history of rash or symptoms such as headache and fever, and whether the palsy affects both sides of the face. If that possibility is more than negligible, a serological test for Lyme disease should be performed. If the test is positive diagnosis is Lyme disease. And if no other cause is found, the diagnosis is Bell’s Palsy.
Sunnybrook facial grading system
It is generally preferred by physiotherapists because of its sensitivity, and the section on synkinesis
The result is expressed as a percentage so instinctively easy to understand and the unaffected side of a face is used for comparison.
The areas of the face are evaluated separately, with the use of five standard expressions:
- Eyebrow raise
- Eye closure
- Open mouth smile
- Show teeth
- Lip pucker
Synkinesis assessment questionnaire
House-Brackmann facial nerve grading scale
Linear measurement index
What are the treatment plans for Facial palsy?
Medical treatment for Facial palsy:
High-dose corticosteroids are frequently administered as well, such as prednisone 60 mg daily, also for 3 weeks, followed by a taper to prevent acute adrenal insufficiency. Corticosteroids may produce multiple side effects & patients should be counseled about the possibility of irritability, insomnia, gastroesophageal reflux, and hyperglycemia.
The greatest danger of facial paralysis is eye damage. Bell’s palsy often keeps eyelids from closing fully. When the eye can not blink normally, the cornea might dry out, and particles may enter and damage the eye.
Patients with facial paralysis should use artificial tears throughout the day and apply an eye lubricant at night. They might also need to wear a special plastic moisture chamber to keep the eye moist & protected.
If facial weakness remains after the completion of medical treatment, the physician may recommend physical therapy to help regain proper action of the facial muscles.
Long-term management of synkinesis can be skilled with both conservative and surgical approaches. Conservative approaches include physical therapy & massage as well as chemo denervation with botulinum toxin. Surgical management of synkinesis may involve selective neurectomy and myomectomy, or even nerve or functional free muscle transfer to improve smile symmetry.
Strong anti-inflammatory drugs called steroids are usually given. Antiviral medicines, such as acyclovir or valacyclovir can also be used.
For those who don’t recover fully, cosmetic surgery can help to correct eyelids that won’t fully close.
Surgical treatment for Facial palsy:
Paralysis of the face may be permanent or temporary. The plastic surgery team determines the best treatment based on how long the paralysis has been present, the cause, and whether it is complete paralysis or incomplete paralysis.
Facial reanimation surgeries which involve nerve graft or anastomosis & muscle transposition
Static surgeries (eg. plastic surgery) are used to improve symmetry at rest but do not improve movement Physiotherapy.
Because of the importance of facial mobility in making recognizable facial expressions and communicating with others, addressing paralysis of the face.
Nerve Transfers
When a facial nerve is injured, there is a period of time during which it may be possible to restore the nerve function to the muscles by transferring another nerve to that area.
If nerve function is absent, as time goes on the muscles of the face weaken, atrophied, and degrade. When one year or more has passed, the opportunity to reinnervate the facial muscles may be lost. Even after that, there are options to restore movement and expression to the face.
The masseter to facial nerve transfer is one of the most advanced treatment options. It involves making an incision near the front of a patient’s ear, following sewing the facial nerve and masseteric nerve together. That way, the patient can restore their natural smile in the months following the procedure.
Gracilis Muscle Transplant
The gracilis muscle is situated in the inner thigh. A small part of this muscle, called a flap, along with its corresponding nerve and blood supply can replace the facial muscles that allow the person to smile.
Using highly specialized techniques, the surgeon transplants the gracilis muscle’s artery and vein and attaches them to corresponding vessels in the head and neck region. This situation is critical for the muscle to survive in its new environment in the face.
There are other stronger muscles in the leg that perform the same function as the gracilis muscle, so even after the surgeon removes this muscle to use in the patient’s face, the patient is not likely to have any long-term problems in moving or walking after the procedure.
Though the gracilis transplant takes longer and involves two surgeries and a two-day hospital stay, it has certain advantages over the temporalis transplant procedure. The smile created by a gracilis transplant does not require teeth clenching and it is more natural looking, involving the whole face rather than just the corner of the mouth.
The first procedure involves moving a nerve to the facial area, Once it is done and heals, the surgeon can perform the second procedure the transplantation of the muscle itself.
The surgeon has many different nerve-grafting options for facilitating motion and sensation to the transplanted muscle and empowering it to work in a new location.
Temporalis Tendon Transfer
The temporalis muscles are located in the face. The muscle’s action is to help with chewing. The plastic surgeon can move these parts to another position.
This technique is very effective in lifting the sagging or droopy mouth. It can restore symmetry, reduces drooling, and even allows the patient to smile again.
One drawback to this surgery is that the patient must clench the teeth to smile. With work, over time, most patients can achieve an almost effortless smile. Although there is minimal risk with chewing.
Cross-Facial Nerve Graft
Because this procedure of nerve graft involves crossing the face from the normal side to the paralyzed side, it is called a cross-facial nerve graft.
First, the surgeon removes a sensory nerve from the lower leg, the sural nerve, and attaches it to a facial nerve branch on the person’s normal side, tunneling the other end of this nerve below the skin to position it in the paralyzed portion of the person’s face. Removal of the leg nerve may result in some numbness around the little toe and the outer edge of the foot.
It takes 6-9 months after this procedure to allow the nerve signal to grow across the nerve graft, from the patient’s normal side to the paralyzed side.
The surgeon then connects the nerve graft to the nerve that moves the gracilis muscle at the time of the gracilis muscle transfer.
Hypoglossal Nerve
The hypoglossal nerve moves half tongue, and the surgeon can use a portion of this nerve to power the transferred gracilis muscle.
Patients undergoing this surgery have a small risk of tongue weakness that can result in difficulty speaking & eating. Exercise is also required to coordinate tongue movement to create a smile.
Dual Innervation
A recent innovation in the field of facial reanimation involves powering the gracilis muscle with multiple nerve sources, such as the masseteric nerve, which boosts the spontaneous smile of the cross facial nerve graft with added power from the masseteric nerve.
Consulting a Plastic Surgeon for Facial Paralysis
The aim of surgery to correct facial palsy is to achieve the best possible function and appearance of the lower part of the face. A patient with facial paralysis should consult with an experienced surgeon who has experience and skill in addressing this problem. The surgeon will consider:
- The cause of the paralysis and which areas of the face are affected
- The results are what the patient expects from the procedure
- The patient’s general health
- The type of surgery most appropriate for the patient
Surgery Procedure and Care
Muscle transplantation surgery is an inpatient procedure. The surgery itself takes an average of six to eight hours. Most patients can go home after three to four days after the hospital.
The patient spends the first day after surgery in the intensive care unit because the team must monitor the gracilis flap every hour for the first 24 hours, every two hours for the following day, and every four hours after that.
If the doctor places a drain in the thigh where the gracilis muscle tissue was removed, the patient will get detailed instructions on caring for the drain at home. When the patient comes for the first postoperative visit the week after surgery, the surgeon will remove the sutures and the drain.
Patients can return to work after two to three weeks of surgery. The surgeon will provide instructions on avoiding strenuous activities such as lifting.
After surgery, it will take several months for the return of the smile function with the movement of the transplanted gracilis muscle. Recovery will vary based on the nerve option chosen. It is important for patients to focus on recovery and maintain a positive attitude.
Swelling After Gracilis Flap Surgery
There will be quite a facial swelling right after surgery, but it will improve during the first couple of weeks. A certain kind of fullness in the face will persist until the transplanted gracilis muscle begins to move. Up to 20 % of patients require revision procedures to reduce the volume of the flap.
Physiotherapy treatment for Facial palsy:
The therapist should instruct the patient about the management of the dry eye if this has not been done by other medical personnel. If the eye becomes red or the patient frequently complains of redness then refer him or her to an opthalmologist. Alternatively, they should be advised to attend an eye hospital emergency department. For more information on dry eye including presentation, risk of corneal ulcer, and management such as the use of artificial lubrication.
- Neuromuscular re-education is essential for recruiting the appropriate muscles and ensuring adequate cortical maps.
- Electrical stimulation treatment includes stimulation on each motor point of the facial muscle – direct current at an intensity sufficient to generate a motor response, a pulsatile waveform that is sent to the threshold of the sub motor, to reduce pain in three times a week
- Electromyography (EMG) and mirror biofeedback
- Trophic electrical stimulation
- Proprioceptive neuromuscular facilitation (PNF) techniques
- Kabat technique therapy
- Self-massage
- The facial massage was performed 10-15 minutes per day consisting of effleurage, kneading, and stretching exercises on the affected side. Studies show that light massage can help muscle relaxation
- Breathing & relaxation exercises
- Relaxation training is needed to increase the patient’s awareness of facial tones & the small stimuli needed to increase muscle activity
- To magnify coordination Exercises between both sides of the face and reduce synkinesis
- Neuromuscular re-education techniques have been found to be effective in increasing facial range of movement and symmetry, as well as reducing or minimizing synkinesis
- Exercises to help with eye & lip closure
- Letter, word & facial expression exercises
- Observation
- Using a mirror during facial movements of the unaffected side will provide visual clues to help the patient make movements on the affected side of the face.
What is the outlook for facial paralysis?
Follow-up care is vital to make sure optimal healing. It is very important to follow the doctor’s post-surgery instructions carefully, like:
Avoiding strenuous activity or lifting according to the instructions
Warn the surgery team immediately in the case of any problem or unexpected change
Keeping follow-up appointments in one day, one week, and one month after surgery.
For patients who have had a stroke, getting medical attention quickly can greatly improve the possibility of a full recovery with limited damage to the brain and body. Rehabilitation and preventative measures will vary depending on the type and severity of the stroke.
Unfortunately, even with all current procedures for therapy, some cases of facial paralysis may never completely go away. For this patient, physical therapy, and eye care can help prevent any further damage and improve quality of life.





One Comment