CHILDHOOD WALKING ABNORMALITIES
During the early years there can be some obvious gait abnormalities in children. While many of these disturbances are quite common and correct themselves on their own, some require medical assistance.
Walking abnormalities are abnormal, uncontrollable walking patterns. Genetics may cause them or other factors, such as diseases or injuries. Walking abnormalities can affect the muscles, bones, or nerves of the legs.
Abnormalities may be present in the entire leg or in certain parts of the leg, such as the knee or ankle. Problems with the foot may also result in walking abnormalities.
These can be temporary or long-term conditions, depending on their cause. Severe walking abnormalities may require continuous physical therapy and medical care.
Walking abnormalities are often referred to as gait abnormalities. Gait refers to the pattern of walking.
There is a considerable variation in normal gait patterns and the ages at which the changes occur, and these appear to be family-history related. Black children tend to walk sooner and Asian children later than average.
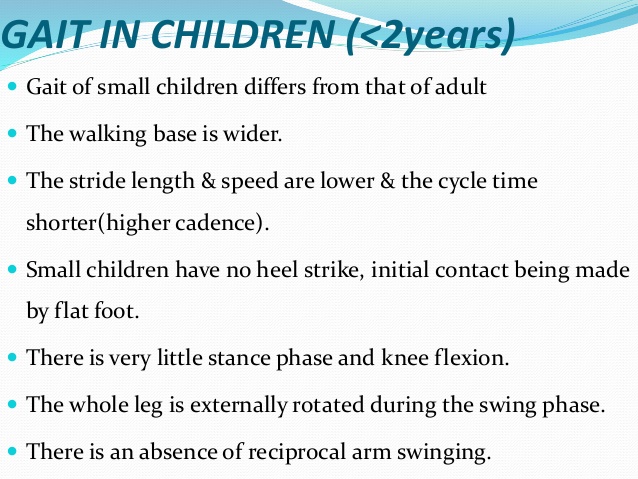
Until a child is approximately 3 years old, their normal gait doesn’t resemble that of an adult.
Initially there is a wide-based stance with rapid cadence and short steps.
Toddlers have a broad-based gait for support, and appear to be high-stepped and flat-footed, with arms outstretched for balance.
Legs are externally rotated, with a degree of bowing.
Heel strike develops at around 15-18 months with reciprocal arm swing.
Running and change of direction occur after the age of 2 years.
In the school-aged child, the step length increases and step frequency slows.
Adult gait and posture occur around the age of 8 years.
Watch a 1 year old wobble around, and you’ll see her gait, or walking cycle, doesn’t quite resemble that of an adult. She’ll have a wider stance, rapid cadence and short steps. In fact, it takes until around age 3 for kids to display clear adult walking patterns.
• During your child’s first few years walking, they may have obvious gait abnormalities—disturbances in what is considered the normal walking cycle for that age group
• The most common types of gait abnormalities are intoeing, outtoeing, limping and toe walking
• Many gait disturbances are common and correct themselves on their own .
• Gait disturbances rarely require medical assistance.
Abnormal gait patterns in children
The following is a list of abnormal gait patterns which may be seen in children and which may need further evaluation.

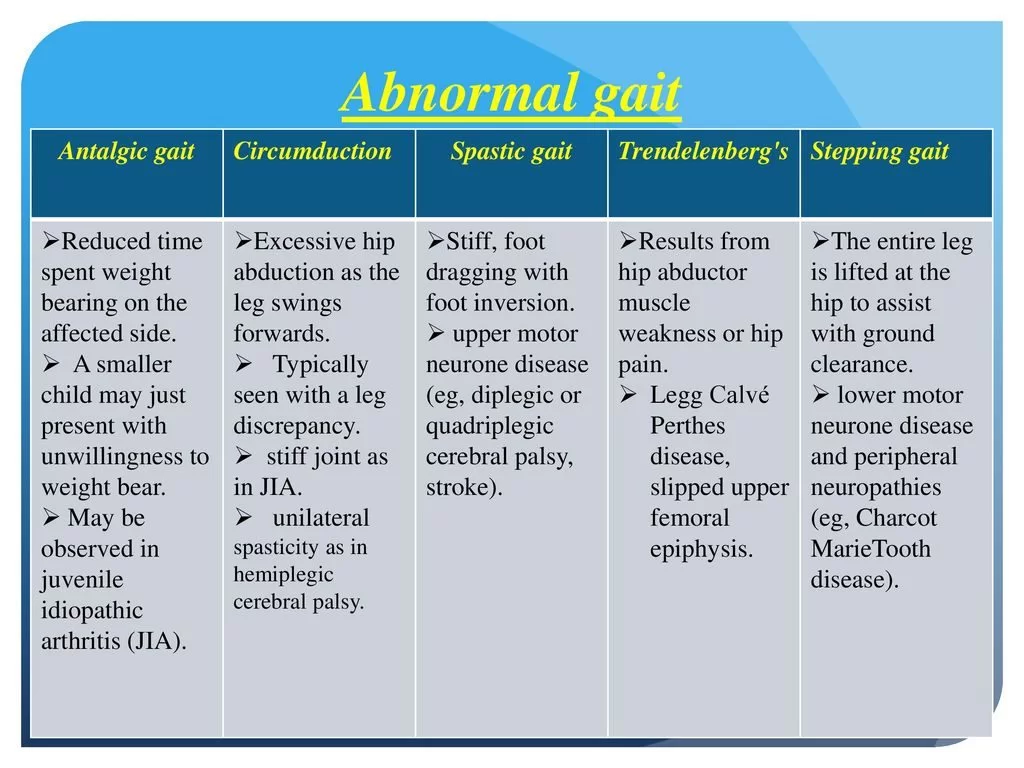
Antalgic gait (caused by pain)
Reduced time spent weight-bearing on the affected side.
A multitude of possible causes.
A smaller child may just present with an unwillingness to weight-bear, so an index of suspicion is required.
May be observed in juvenile idiopathic arthritis (JIA), although children do not always complain of pain.
Circumduction gait
Excessive hip abduction as the leg swings forward
Typically seen with a leg length discrepancy, with a stiff/restricted joint movement as in JIA, or with unilateral spasticity as in hemiplegic cerebral palsy.
Spastic gait
Stiff, foot-dragging with foot inversion. This is often seen in upper motor neurone neurological disease (eg, diplegic or quadriplegic cerebral palsy, stroke).
Ataxic gait
Instability with an alternating narrow-to-wide base.
Seen in ataxic cerebral palsy affecting the cerebellum, in cerebellar ataxia, and in Friedreich’s ataxia.
Trendelenberg’s gait
Results from hip abductor muscle weakness or hip pain. While weight-bearing on the ipsilateral side, the pelvis drops on the contralateral side, rather than rising as is normal. With bilateral hip disease, this leads to a waddling ‘rolling sailor’ gait with hips, knees, and feet externally rotated.
May be observed in Legg-Calvé-Perthes disease, slipped upper femoral epiphysis, developmental dysplasia of the hip, arthritis involving the hip, muscle disease (eg, inherited myopathies), and neurological conditions.
Toe-walking gait with absent heel contact
Habitual toe walking is common in children and associates with normal tone, range of movement around the feet and normal walking on request. However, persistent toe walking is observed in spastic upper motor neurone neurological disease (eg, cerebral palsy). It can (rarely) be a presentation of mild lysosomal storage disorder.
Stepping gait
The entire leg is lifted at the hip to assist with ground clearance.
Occurs with weak ankle dorsiflexors, compensated by increased knee flexion.
Observed in lower motor neurone neurological disease (eg, spina bifida, polio) and peripheral neuropathies (eg, Charcot-Marie-Tooth disease).
‘Clumsy’ gait
This term is commonly used to describe difficulties in motor co-ordination (fine and gross motor skills).
The child may present with frequent falls, and with difficulty in self-help skills such as dressing or feeding at school.
Poor handwriting and learning disabilities may be noted.
It is important to exclude specific, albeit mild, neurological disabilities (cerebral palsy, cerebellar ataxia, or lower motor neurone disorders), inflammatory arthritis or myopathies, and orthopaedic problems such as in-toeing.
Dyspraxia is a term for children with delayed motor development who fall in the bottom 5% for their age group. By definition this includes 5% of children and is a late-maturation problem which tends to be familial and is more common in boys. It causes ‘clumsiness’ but there is no specifically altered gait.
Common types of gait abnormalities include intoeing and outtoeing:
If your child’s feet point inward instead of pointing straight ahead when walking or running, it’s called intoeing. Out-toeing means that the feet curve outward instead of pointing straight.
• Intoeing and outtoeing are the most common gait disturbances that cause parents to seek advice from their child’s doctor .
• Most children outgrow the condition naturally and don’t need special shoes,stretching exercises or special casts, braces or surgery .
• Infants and toddlers with intoeing and outtoeing can go barefoot without causing problems to the feet
• Intoeing and outtoeing usually don’t cause your child pain and don’t interfere with the way your child learns to walk
What causes intoeing and outtoeing?
The most common conditions that can cause a child’s foot or feet to curve inward or outward include:
Tibial torsion
Tibial torsion is the turning of your child’s lower leg (tibia) either inward (internal tibial torsion) or outward (external tibial torsion).
The condition improves without treatment, usually before age 4. Consider surgery only if your child is at least 8 to 10 years old, and the problem has persisted, causing significant walking problems Occasionally, a brace is used at night in children 18 to 30 months of age.
Femoral torsion
Femoral torsion is the inturning or outturning of your child’s upper leg bone (femur). It’s most apparent when your child is about 5 to 6 years old, however the condition can improve without treatment. Intoeing from femoral torsion becomes worse between 2 and 4 years of age.
Consider surgery only if your child is older than 9 and has a very severe condition that causes a lot of tripping and an unsightly gait.
Bowlegs and knock-knees
Children with bowlegs or knock-knees usually straighten out as your child grows. A wide range of knee alignment is normal in young children.
Special shoes and wedges don’t help either condition.
Flat feet
Flatfeet are normal in infants and young children; the arch develops in your child’s foot until at least age 5.
Metatarsus adductus
Metatarsus adductus is a common birth defect in which your child’s feet bend inward from the middle to the toes. In severe cases, it may resemble clubfoot deformity. The condition improves by itself most of the time, and newborns with Metatarsus adductus are not treated until they’re at least several months old.
Treatment usually involves special exercises, applying casts or special corrective shoes and has a high rate of success in babies aged 6 to 9 months.
Limping
If your child is suddenly limping, it’s most likely due to pain caused by a minor, easily treated injury.
• Splinters, blisters or tired muscles are common culprits, but sometimes limping can involve a more serious
problem such as a sprain, fracture, dislocation, joint infection, arthritis or, less commonly, a tumor
• While evaluating your child, the doctor will try to distinguish between painful limping and non-painful limping
• Non-painful chronic limping may be indicative of developmental problem, such as developmental dysplasia of the hip or neuromuscular problem, such as cerebral palsy
Toe-walking
Toe-walking is one of the least common gait abnormalities. After age 3, if your child walks on his or her toes, they need careful evaluation by a physician.
Most cases of persistent toe-walking are familial or are simply secondary to tight muscles. Treatment may involve observation, physical therapy, casting or surgery. Toe-walking may indicate a neuromuscular disorder such as cerebral palsy or it could be a sign of developmental dysplasia of the hip or leg length discrepancy.
Assessment of gait disturbance
Developmental and general history
Establish the parent’s concerns.
Take a detailed pregnancy, birth and development history (perinatal events and motor development abnormalities may reveal a diagnosis of cerebral palsy).
Walking delay beyond 18 months needs investigation, particularly in boys, to exclude neuromuscular diseases, as does global delay with speech, hearing, vision, and fine motor milestones.
Delay and evidence of multisystem involvement warrant consideration of metabolic causes (osteomalacia and lysosomal storage disease).
Regression of motor milestones is always significant. Inflammatory arthritis (ie juvenile idiopathic arthritis (JIA)), inflammatory myopathies (eg, juvenile dermatomyositis) and neurodegenerative disorders need to be considered.
Family history: there is frequently a familial tendency to clumsiness or in-toeing. However, muscular dystrophies are also familial and presentation is usually in children aged 2-3 years.
Ethnicity:
Black children tend to walk earlier than Asian children.
The risk of osteomalacia is higher in children of Asian families with poor sun exposure and dietary vitamin D deficiency (eg, from chapati flour not fortified with vitamin D and with a high phytic acid content that inhibits calcium absorption).
Sickle cell disease is common in children of central African origin and may be present in children of Mediterranean and western Asian origin
History of symptoms
Signs and symptoms; ask about pain, limping, tripping and falling.
Ask about difficulty getting up from sitting.
Sitting habits: internal tibial torsion is commonly associated with sitting on the feet, while increased femoral anteversion is associated with sitting in a ‘W’ position.
Aggravating factors: torsional deformities become more apparent with fatigue. Age at onset of symptoms is helpful in considering the differential diagnoses of limp. For example, transient synovitis (toxic synovitis, irritable hip) is more likely in the young of school age.
If there is pain, ask for information on the site of the pain, its duration, and periodicity (acute onset and persistent pain/limp suggest trauma or serious causes such as infection).
Unwitnessed trauma is common in very young children. Toddler’s fracture needs to be considered in apparently well but non-weight-bearing young children. Put non-accidental injury (NAI) through your diagnostic sieve.
Overuse injuries (stress fractures, avulsion fractures) may be subacute or acute and are more common in active children.
Gait disturbance (antalgic limp) and stiffness are more common in JIA. Parents may observe irritability, poor sleep, unwillingness to walk (regression of motor milestones).
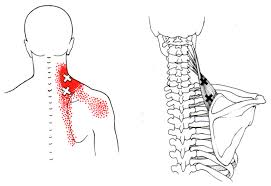
Referred pain (especially spinal or hip disease manifesting as thigh and knee pain) must always be considered, especially in young children who may have difficulties localising problems.
Intermittent symptoms that increase with or after exercise suggest mechanical problems.
Diurnal variation, with symptoms often worse in the mornings or after periods of rest (gelling), suggests inflammatory causes, and may be chronic for several weeks before presentation.
Relieving factors
A good response to non-steroidal anti-inflammatory drugs (NSAIDs) suggests inflammatory causes.
Postures that alleviate pain are helpful for diagnosis. Children with an irritable hip (toxic synovitis, transient synovitis) usually adopt a position of hip flexion, external rotation, and slight abduction.
Red flags
In all history-taking check for the presence of red flags:
Systemic upset (eg, fever, chills, weight loss, night pain) always necessitates consideration of infection or malignancy.
Suspicions raising concern of NAI – eg, inconsistent parental history, delayed presentation, minimisation of symptoms, incongruent injuries, recurrent injuries, previous concerns, parental anger.
Limitation of activities always warrants concern. Marked functional limitation despite few physical signs suggests complex regional pain syndromes. Specialist assessment is warranted.
Travel history
History of recent travel abroad may be relevant for acute monoarthritis, Lyme disease (there may also be history of a tick bite or rash) and reactive arthritis (following a gastrointestinal infection, Shigella, Yersinia, Campylobacter species).
Travel history of family members may be relevant for tuberculosis.
Systematic factors
Recent sore throat, chest infection and upper respiratory tract infection may precede symptoms of an irritable hip (characteristically following an interval of 10 to 14 days after the infectious episode).
Gastrointestinal upset (possibly following foreign travel) may predate reactive arthritis.
Sexual history may be relevant in the older child/adolescent with a presentation suggestive of reactive arthritis.
Rashes such as psoriasis may associate with psoriatic arthritis.
Photosensitive rash in the presence of arthralgia and malaise, especially in an adolescent girl, may indicate systemic lupus erythematosus but is less likely to present with limp.
A maculopapular rash, often occurring at times of high fever, is characteristic of systemic-onset JIA.
Prior history of red eye is typical of acute uveitis in HLA-B27-associated arthritis in children.
How to examine gait and stability
First, observe the child entering the room – speed, stride, balance.
Ask them to walk across the room, turn, and come back.
Ask them to walk heel-to-toe in a straight line.
Ask them to walk on their toes in a straight line, and then to walk on their heels in a straight line.
Ask them to hop in place on each foot.
Ask them to do a shallow knee bend.
Ask them to rise from a chair and walk forwards across the room, turn and come back to you.
Assess cerebellar function – eg, Romberg’s test, finger-nose pointing, heel-to-shin testing
The assessment and examination of gait and balance need to be supplemented by appropriate history and examination of all systems. In particular in children, attention must be paid to developmental history, speed of onset and any deterioration or regression, and any signs of systemic involvement.
Examination
General examination should include height, weight, temperature, and general appearance.
Look for evidence of dysmorphia.
Growth charts including height and weight are important in assessment; normal size for age is reassuring for good general health, and makes chronic pathological conditions much less likely.
Check heart, lungs, abdomen, lymph nodes.
The child should be examined comprehensively, barefoot and with legs exposed, as the symptoms may be vague and poorly localised.
Joint examination should include all joints and a screening examination of gait, arms, legs, and spine as a minimum.
Look for asymmetry. Handedness before the age of 18 months is abnormal.
Simple screening tests for gross motor skills include walking on sides of the feet or standing on one leg, hopping, skipping, and kicking a ball, or heel-toe walking.
Look for asymmetry in limb function. Handedness before the age of 18 months is abnormal.
Musculoskeletal assessment
First, observe the walk.
Joint screening using the pGALS (paediatric gait, arms, legs, spine) screen has been validated in school-aged children and comprises a series of simple manoeuvres to screen all joints involving the following (clinician’s action italicised below):
GAIT
Observe the child walking. Then ask the child to do the following:
Walk on your tip-toes and on your heels.
ARMS
Ask the child to do the following:
Put your hands out in front of you.
Turn your hands over and make a fist.
Pinch your index finger and thumb together. Touch the tips of your fingers with your thumb.
Squeeze the child’s metacarpophalangeal joints.
Put your hands together/put your hands back to back.
Reach up and touch the sky.
Look at the ceiling.
LEGS
Ask the child to do the following:
Put your hands behind your neck.
Feel for effusion at the knee.
Bend and then straighten your knee
Feel for crepitus.
Passively flex the knee and internally rotate the hip.
SPINE
Open your mouth and put three fingers in.
Touch your shoulder with your ear (each side)
Observe the spine from behind.
Bend and touch your toes.
Observe the curve of spine from behind and sideways.
The spine should be examined for scoliosis, hairy patches or sinus openings.
The lower extremities should be examined for Trendelenburg’s sign. This is when the pelvis tilts toward the normal hip when weight is borne on the affected side.
Leg length should be measured. If there is no discrepancy, hip dysplasia can be ruled out.
The range of motion of the hips, knees, and ankles should be determined. Evidence of joint laxity that mimics the appearance of a torsional/angular deformity should be checked.
Presence or absence of flat feet should be determined.
The lateral border of the foot should be checked. If it is curved inwardly, the child has metatarsus adductus.
Normal ankle dorsiflexion above the neutral position should be checked to determine if the foot deformity is flexible.
Look for bone tenderness or soft tissue swelling/bruising.
Consider symmetry of joint appearance, joint range of movement, hypermobility, muscle wasting and muscle bulk, and leg length discrepancy.
Use Trendelenberg’s test for weak hip abductors (consider hip pathology).
In babies and toddlers screen for ‘clicky hips’ using Barlow’s and Ortalani’s manoeuvres.
Neurological assessment
Muscle wasting, sensation, tone and power (particularly in the lower limbs) should be assessed to rule out neuromuscular disorders.
Evidence of muscle wasting raises the possibility of peripheral neuropathies (Charcot-Marie-Tooth syndrome).
Pseudo-hypertrophy is typical of Duchenne muscular dystrophy and Becker’s muscular dystrophy.
Persistent primitive reflexes suggest neurological disease or cerebral palsy.
Gower’s test for proximal weakness (muscle dystrophies, hip disease) involves asking the child to get up unaided from a sitting position on the floor and observing for evidence of difficulty.An abnormal Gower’s test can often be predicted in a child over 5 years of age who is not able to jump.
Investigations
If abnormalities are suspected, investigations are likely to be done in secondary care.
Investigation may include:
Blood tests; FBC, ESR, CRP.
Blood cultures and serology.
Bone chemistry and autoantibodies, muscle enzymes, coagulation screen.
Plain X rays as the situation requires.
CT and MRI scans.
Ultrasound.
Bone scan.
Genetic testing.
Differential diagnosis
The differential diagnosis below includes conditions which are normal for age or normal variants for age, together with conditions which need further investigation and those which require urgent secondary care review.
In-toeing and out-toeing
These are the most common gait disturbances and are common causes of parental concern.
Clinical features
In-toeing means that the feet point inwards instead of pointing straight ahead when walking or running.
Out-toeing means that the feet curve outwards instead of pointing straight.
Aetiology
Out-toeing patterns largely result from one of the following.
External rotation hip contracture.
External tibial torsion.
External femoral torsion.
In-toeing in otherwise normal newborns and infants may result from:
Metatarsus adductus – the diagnosis if a ‘C’-shaped curve, rather than a straight border, is present on the lateral aspect of the foot. About 90% of cases resolve by one year of age. Treatment usually involves special exercises, and applying casts or special corrective shoes, and has a high rate of success in babies aged 6-9 months.
Internal tibial torsion – although a normal finding in the newborn, this is usually a matter of concern at walking age. When the child is walking or standing, the patella can be seen to point forward, with the foot pointing inward.
Excessive femoral anteversion – the most common cause of in-toeing. The normal range is from 30-40° at birth and decreases progressively throughout growth to about 15° at skeletal maturation. Children walk or stand with both patellae and feet pointing inward. If found in conjunction with internal tibial torsion it may lead to patellofemoral subluxation.
Assessment
A normal neurological examination and normal height and weight for age help exclude most associated skeletal dysplasias, and neuromuscular or metabolic diseases.
Advice to the parents
Children outgrow the condition naturally in the majority of cases.
Infants and toddlers with in-toeing and out-toeing can go barefoot without causing problems to the feet.
Severe in-toeing or out-toeing may cause the child to stumble or trip.
They usually do not cause the child pain or interfere with the way the child learns to walk.
Neither problem has been linked to arthritis in adulthood.
Management
Since disability from in-toeing is extremely rare and most cases resolve spontaneously, observation and parental education are important from the time of diagnosis. Non-surgical treatment of in-toeing, with the exception of casting in children with metatarsus adductus, has not been shown to be effective. Conditions that support considering a surgical approach include:
The child is older than 8 years of age.
There is severe deformity that creates significant cosmetic and functional disability – anteversion in excess of 50°.
Deformity of more than three standard deviations beyond the mean.
A family which is aware of the risks of the procedure.
Osteotomy, the only effective treatment for rotational abnormalities of the femur and tibia, has high complication rates and should not be considered until the patient is 8-10 years of age.
Bow legs and knock knees
A wide range of knee alignment is normal in young children.
Assessment
Early radiographic screening and/or referral to a clinical specialist are often used to distinguish between physiological bow-leg deformity and infantile tibia vara disease in young children. Most of these children have physiological bowing: routine radiographic screening and referral are not cost-effective and expose children to unnecessary radiation.
The ‘cover up’ test is an effective screening tool for the assessment of bow legs in children aged between 1 and 3 years and qualitatively assesses the alignment of the proximal portion of the lower leg relative to the thigh or upper leg.It is performed with the patella pointing up and the hand perpendicular to the thigh, covering the mid-tibia. Assess the upper third of the tibia in relation to the femur:
Obvious valgus alignment is considered a negative test and is indicative of physiological bowing.
Neutral or varus alignment is considered a positive test and suggests that the child is at greater risk for having infantile tibia vara.
Children with a negative ‘cover up’ test do not require radiographic evaluation and should be followed clinically for resolution of the bowing.
Management
Children with a positive ‘cover up’ test should have radiographic evaluation of the lower extremities or be referred to a specialist for further evaluation and treatment.

Surgery should be performed only after the age of 8-10 years, for persistent, severe deformity – ie the child should have more than 50° of measured anteversion and more than 80° of medial hip rotation.
Prognosis
The majority of children will grow out of this condition.
Flat feet
Flat feet are normal in infants and young children. The arch does not develop in a child’s foot until at least 2-3 years of age.
Limping
If a child is suddenly limping, (walking with an unsteady gait, favouring one leg), it is most likely due to pain caused by a minor, easily treated injury. However, if an obvious cause cannot be found or if the limp does not resolve quickly, a thorough investigation for serious pathology should be undertaken.
Differential diagnosis
Splinters, blisters or tired muscles are common causes. More serious problems include:
Developmental – eg, hip dysplasia, cerebral palsy.
Trauma – eg, fracture, non-accidental injury, puncture wound, slipped femoral epiphyses.
Infections – eg, osteomyelitis, septic arthritis, synovitis (viral, bacterial or atypical – Lyme disease).
Osteochondroses – eg, Perthes’ disease.
Neoplasia – eg, leukaemia.
Inflammatory – eg, JIA.
Non-painful chronic limping may be indicative of a developmental problem, such as developmental dysplasia of the hip, or of a neuromuscular problem, such as cerebral palsy.
Assessment
A limp may be secondary to disorders in the abdomen, genitourinary tract, back, pelvis, hip, knee, foot or elsewhere on the body. The assessment focuses on the pain, weakness, or both, surrounding the gait abnormality. The onset, quality, location, resolving or precipitating factors, and duration of pain and weakness, are also important. A review of systems may reveal weight loss, night sweats, fever, or psychosocial issues.
Examination
Begin with an overall assessment of the child, including their vital signs.
The abdomen, pelvis, back, and extremities of the supine or sitting child should be inspected and palpated. Inspection and palpation are best done with the child sitting in the parent’s lap.
Neurovascular status (including strength, sensation and reflexes) can also be assessed while the child is sitting or supine.
Each digit and joint should be examined for motion, ligamentous stability and occult trauma.
The child should be observed barefoot and minimally clothed to assess stance and gait. The child should be observed in an open area to observe several gait cycles to elicit the gait abnormality and anatomic location. Running often brings out subtle abnormalities.
Measure and compare lower-leg lengths.
It is difficult to identify the range of gait deviations associated with JIA using simple clinical observations. Scientific gait analysis allows accurate targeting of physiotherapy and orthotic interventions to suit each individual.
Investigations
Blood tests should include FBC, ESR and CRP.
Blood cultures may be indicated.
Sickle cell tests, Lyme disease titres, lupus antibodies, anti-double-stranded DNA, rheumatoid factor, human leukocyte antigen, creatine kinase are only requested if suggested from the history.
Plain X-ray should be the initial study. Anteroposterior (AP) radiographs of the pelvis and AP and lateral views of both lower extremities are recommended, particularly in very young children.
Ultrasound is a valuable diagnostic tool.
Bone scintigraphy using technetium highlights areas of increased bone metabolism and may help to identify occult fractures, osteomyelitis, and Calvé-Legg-Perthes disease.
CT scanning is effective for abdominal and pelvic pathology (eg, sacroiliac trauma) and bony pathology of the hip, knee, spine, and foot.
MRI is the study of choice for soft tissue pathology and for evaluation of bone tumours.
Toe-walking
Toe-walking is one of the least common gait abnormalities.
If the child walks on his or her toes and is under 3 years old, the problem can be normal.
After age 3, if the problem persists, it requires careful evaluation.
Aetiology
Most cases of persistent toe-walking are familial or are simply secondary to tight muscles.
Toe-walking may indicate a neuromuscular disorder such as cerebral palsy or it could denote developmental dysplasia of the hip or leg length discrepancy (if it involves one foot only).
Management
Treatment may involve observation, physical therapy, casting or surgery.
Urgent causes of limp in children
Sepsis
a febrile unwell child with acute limp, not weight-bearing, or unable to move the joint (septic arthritis or osteomyelitis) requires urgent medical attention.
Malignancy
Malignancy should be suspected in children with persistent pain, bone pain, bone/soft-tissue swelling, and systemic upset (fever, weight loss, night sweats, or presence of lymphadenopathy, abdominal mass, or organomegaly). Possible causes include primary bone tumours, neuroblastoma and leukaemia.
Non-accidental injury (NAI)
If suspected, child protection management procedures should be followed.
Inflammatory disorders
Inflammatory disorders may present with fatigue, rash, myalgia, arthralgia, pain, fever, malaise, and multisystem involvement.
In some cases of inflammatory arthritis (such as JIA) or inflammatory muscle disease, the presentation can be indolent with regression of motor milestones, with or without systemic upset.