CEREBRAL PALSY
Table of Contents
What is a Cerebral Palsy?
- Cerebral palsy (CP) is a group of permanent movement disorders that appear in early childhood.
- Signs and symptoms vary among people and over time.
- Often, symptoms include poor coordination, stiff muscles, weak muscles, and tremors.
- There may be problems with sensation, vision, hearing, swallowing, and speaking.
- Often, babies with cerebral palsy do not roll over, sit, crawl or walk as early as other children of their age.
- Other symptoms include seizures and problems with thinking or reasoning, which each occur in about one third of people with CP.
- While symptoms may get more noticeable over the first few years of life, underlying problems do not worsen over time.
- Cerebral palsy is caused by abnormal development or damage to the parts of the brain that control movement, balance, and posture.
- Most often, the problems occur during pregnancy; however, they may also occur during childbirth or shortly after birth. Often, the cause is unknown.
- Risk factors include preterm birth, being a twin, certain infections during pregnancy such as toxoplasmosis or rubella, exposure to methyl mercury during pregnancy, a difficult delivery, and head trauma during the first few years of life, among others. About 2% of cases are believed to be due to an inherited genetic cause.
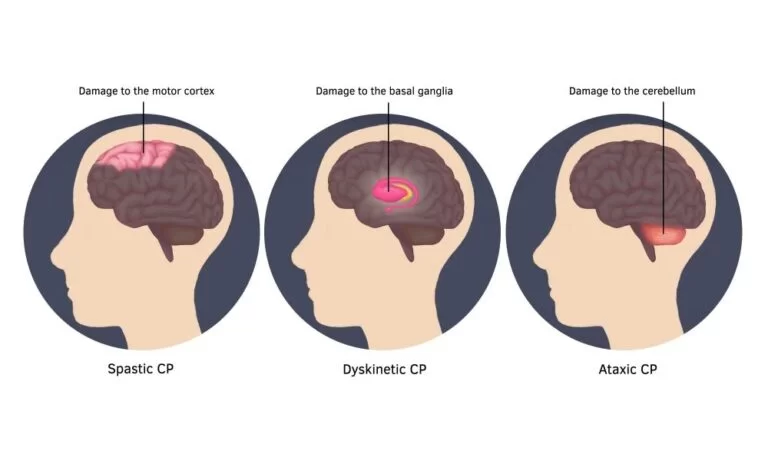
- A number of sub-types are classified based on the specific problems present.For example, those with stiff muscles have spastic cerebral palsy, those with poor coordination have ataxic cerebral palsy and those with writhing movements have athetoid cerebral palsy.
- Diagnosis is based on the child’s development over time.
- Blood tests and medical imaging may be used to rule out other possible causes.
- CP is partly preventable through immunization of the mother and efforts to prevent head injuries in children such as through improved safety.There is no cure for CP; however, supportive treatments, medications and surgery may help many individuals.
- This may include physical therapy, occupational therapy and speech therapy.
- Medications such as diazepam, baclofen and botulinum toxin may help relax stiff muscles.
- Surgery may include lengthening muscles and cutting overly active nerves Often, external braces and other assistive technology are helpful.
- Some affected children can achieve near normal adult lives with appropriate treatment.
- While alternative medicines are frequently used, there is no evidence to support their use.
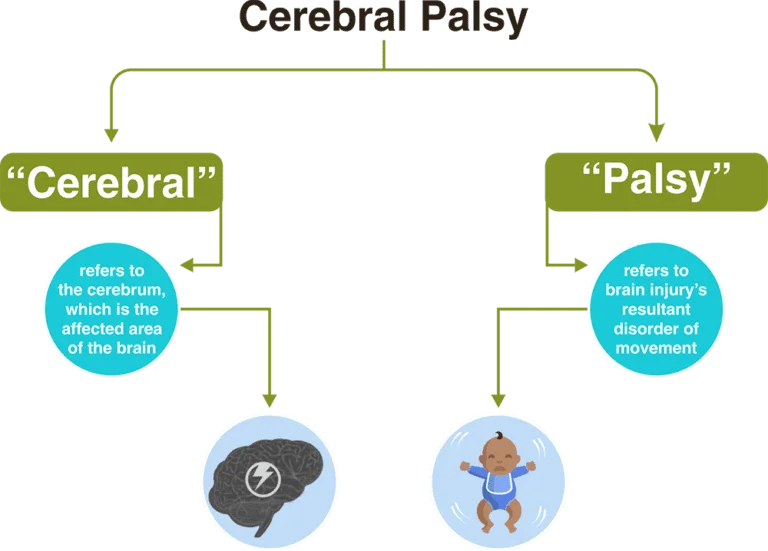
- Cerebral palsy is a term used to describe a set of neurological conditions that affect movement.
- Cerebral palsy is the most common movement disorder in children & form of childhood disability.
- It occurs in about 2.1 per 1,000 live births. It affects around 764,000 individuals in the United States.
History :
- First known descriptions occurring in the work of Hippocrates in the 5th century BCE.
- Extensive study of the condition began in the 19th century by William John Little, after whom spastic diplegia was called “Little’s disease”.
- William Osler first named it “cerebral palsy” from the German zerebrale Kinderlähmung (cerebral child-paralysis).
- Dr. Sigmund Freud, a renowned psychiatrist, along with a neurologist, made the connection.
- He was first to state that cerebral palsy might be caused by abnormal development before birth
- A number of potential treatments are being examined, including stem cell therapy .
- However, more research is required to determine if it is effective and safe.
- The condition makes it hard to move certain parts of the body. There are many degrees of severity.
- Because of damage to certain parts of the brain, voluntary or involuntary movements or both can be affected.
- Cerebral palsy is not contagious, it does not necessarily affect intelligence or cognitive ability, and it is not progressive, so it does not get worse with age.
- Some people find that symptoms improve over time.
- People with cerebral palsy tend to have a normal lifespan, and in many cases, a good quality of life can be expected.
Causes :
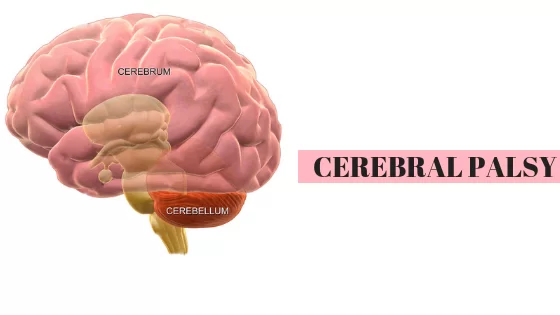
Cerebrum :
- Muscle control takes place in a part of the brain called the cerebrum.
- The cerebrum is the upper part of the brain. Damage to the cerebrum before, during, or within 5 years of birth can cause cerebral palsy.
- The cerebrum is also responsible for memory, ability to learn, and communication skills.
- This is why some people with cerebral palsy have problems with communication and learning.
- Cerebrum damage can sometimes affect vision and hearing.
Prenatal causes [ before delivery ] :
- Heredity
- Infection
- Trauma
- Prenatal anoxia
- Prematurity
- Early pregnancy
- Metabolic disorders
- Some vaccine
- Late age pregnancy
- Psychological stress
- Jaundice
- Hypoglycemia
Perinatal causes [ during delivery ]:
- Trauma [ birth injury ]
- Rapid delivery
- Lack of oxygen [ fetal asphyxia , anoxia or hypoxia ]
- Forceps delivery
- Asphyxia [ decrease oxygen ]
- Prolong second stage of delivery
- Child gulp stool / urine
- Breech presentation
Postnatal causes [ after delivery ] :
- Traumatic head injuries
- Toxic condition
- Sever jaundice
- Hypoglycemia
- Neonatal meningitis
- Encephalitis
- Brain tumors
- Brain hemorrhages
- Cerebral anoxia
Risk factor :
- Multiple births, for example, twins
- Damaged placenta
- Sexually transmitted infections (STIs)
- Consumption of alcohol, illegal drugs, or toxic substances during pregnancy
- Malnourishment during pregnancy
- Random malformation of the fetal brain
- Small pelvis in the mother
- Breech delivery
- Brain damage after birth
- A small proportion of cases happen because of damage after birth. This can happen because of an infection such as meningitis, a head injury, a drowning accident, or poisoning.
When damage occurs, it will do so soon after the birth. With age, the human brain becomes more resilient and able withstand more damage.
Symptoms :
- An infant with cerebral palsy may have muscular and movement problems, including poor muscle tone.
- Muscle tone refers to a person’s automatic ability to tighten and relax muscle when required.
- overdeveloped or underdeveloped muscles, leading to stiff or floppy movements
- Poor coordination and balance, known as ataxia
- Involuntary, slow writhing movements, or athetosis
- Stiff muscles that contract abnormally, known as spastic paralysis
- Crawling in an unusual way
- Lying down in awkward positions
- Favoring one side of the body over the other
- A limited range of movement
- Late achievement of developmental milestones such as crawling, walking, or speaking
- Hearing and eyesight problems
- problems controlling bladder and bowel movements
- Seizures
- Drooling, and problems with feeding, sucking, and swallowing
- Being easily startled
- Symptoms normally start to show during the first 3 years of life.
Types :
There are five types of cerebral palsy:
- Spastic
- Athetoid-dyskinetic
- Ataxic
- Hypotonic
- Mix.
Spastic cerebral palsy :
There are three different types of spastic cerebral palsy.
Spastic hemiplegia:
- A child with spastic hemiplegia will typically have spasticity, or muscle stiffness, on one side of the body.
- This is usually just a hand and an arm, but it may also involve a leg.
- The side that is affected may not develop properly. There may be speech problems.
- Intelligence is not usually affected. Seizures may occur.
Spastic diplegia:
- The lower limbs are affected, and the upper body has no spasticity or only a little.
- The leg and hip muscles are tight. Legs cross at the knees, making walking more difficult.
- The crossing of the legs when upright is often referred to as scissoring.
Spastic quadriplegia:
- The legs, arms, and body are affected.
- This is the most severe form of spastic cerebral palsy.
- It may involve cognitive deficits.
- Walking and talking will be difficult.
- Seizures may occur.
Athetoid or dyskinetic cerebral palsy :

- Also known as athetoid dyskinetic cerebral palsy, this is the second most common type.
- Intelligence is usually normal, but muscle problems affect the whole body.
- Weak or tight muscle tone causes random and uncontrolled body movements.
- The child will have problems walking, sitting, maintaining posture, and speaking clearly because the tongue and vocal cords are hard to control.
- Some children drool if they have problems controlling facial muscles.
Ataxic cerebral palsy :
- Balance and coordination are most affected.
- Tasks that need fine motor skills will be difficult, such as tying shoelaces, buttoning up shirts, and cutting with scissors.
- Balance difficulties may cause the child to walk with their feet far apart.
- Most children with ataxic cerebral palsy have normal intelligence and good communication skills, but some may have erratic speech.
Hypotonic cerebral palsy :

- Hypotonic cerebral palsy results from an injury to the cerebellum.
- Muscle problems appear earlier.
- The infant’s head and body will be floppy, “like a rag doll.”
- There is only moderate resistance when an adult tries to move the infant’s limbs.
- The infant may rest with their elbows and knees loosely extended, instead of flexed.
- There may be breathing difficulties.
Mixed cerebral palsy :
- Some people have a combination of symptoms from the different types of CP.
- This is called mixed CP.
- In most cases of mixed CP, people experience a mix of spastic and dyskinetic CP.
Gross Motor Function Classification System (GMFCS) :
- Cerebral palsy is classified according to the Gross Motor Function Classification System (GMFCS).
- The World Health Organization (WHO) and the Surveillance of Cerebral Palsy in Europe developed the GMFCS as a universal standard for determining the physical capabilities of people with CP.

The system focuses on:
- The ability to sit
- The capability for movement and mobility
- Charting independence
- The use of adaptive technology
- The five levels of the GMFCS increase with decreasing mobility:
Level 1 cerebral palsy :
- CP is characterized by being able to walk without limitations.
Level 2 cerebral palsy :
- A person with level 2 CP can walk long distances without limitations, but they can’t run or jump.
- They may need assistive devices, such as leg and arm braces, when first learning to walk.
- They also may need to use a wheelchair to get around outside of their home.
Level 3 cerebral palsy :
- A person with level 3 CP can sit with little support and stand without any support.
- They need handheld assistive devices, such as a walker or cane, while walking indoors.
- They also need a wheelchair to get around outside of the home.
Level 4 cerebral palsy :
- A person with level 4 CP can walk with the use of assistive devices.
- They’re able to move independently in a wheelchair, and they need some support when they’re sitting.
Level 5 cerebral palsy :
- A person with level 5 CP needs support to maintain their head and neck position.
- They need support to sit and stand, and they may be able to control a motorized wheelchair.
Diagnosis :
The diagnosis of cerebral palsy has historically rested on the person’s history and physical examination.
Physical examination :
- A general movements assessment, which involves measuring movements that occur spontaneously among those less than four months of age, appears most accurate Children who are more severely affected are more likely to be noticed and diagnosed earlier.
- Abnormal muscle tone, delayed motor development and persistence of primitive reflexes are the main early symptoms of CP.
- Symptoms and diagnosis typically occur by the age of 2 although persons with milder forms of cerebral palsy may be over the age of 5, if not in adulthood, when finally diagnosed.
- Early diagnosis and intervention are seen as being a key part of managing cerebral palsy.
- It is a developmental disability.
Once a person is diagnosed with cerebral palsy, further diagnostic tests are optional.
CT OR MRI :
- Neuroimaging with CT or MRI is warranted when the cause of a person’s cerebral palsy has not been established.
- An MRI is preferred over CT, due to diagnostic yield and safety.
- When abnormal, the neuroimaging study can suggest the timing of the initial damage.
- The CT or MRI is also capable of revealing treatable conditions, such as hydrocephalus, porencephaly, arteriovenous malformation, subdural hematomas and hygrometers, and a vermian tumour(which a few studies suggest are present 5–22% of the time). Furthermore, an abnormal neuroimaging study indicates a high likelihood of associated conditions, such as epilepsy and intellectual disability.
- There is a small risk associated with sedating children in facilitate a clear MRI.
Age-related diagnosis :
- The age when CP is diagnosed is important, but medical professionals disagree over the best age to make the diagnosis.
- The earlier CP is diagnosed correctly, the better the opportunities are to provide the child with physical and educational help, but there might be a greater chance of confusing CP with another problem, especially if the child is 18 months of age or younger.
- Infants may have temporary problems with muscle tone or control that can be confused with CP, which is permanent.A metabolism disorder or tumors in the nervous system may appear to be CP; metabolic disorders, in particular, can produce brain problems that look like CP on an MRI.
- Disorders that deteriorate the white matter in the brain and problems that cause spasms and weakness in the legs, may be mistaken for CP if they first appear early in life. However, these disorders get worse over time, and CP does not(although it may change in character).
- In infancy it may not be possible to tell the difference between them.In the UK, not being able to sit independently by the age of 8 months is regarded as a clinical sign for further monitoring.
- Fragile X syndrome (a cause of autism and intellectual disability) and general intellectual disability must also be ruled out .Cerebral palsy specialist John McLaughlin recommends waiting until the child is 36 months of age before making a diagnosis, because by that age, motor capacity is easier to assess.
Classification :
According to motor impairment :
- CP is classified by the types of motor impairment of the limbs or organs, and by restrictions to the activities an affected person may perform.
- The Gross Motor Function Classification System-Expanded and Revised and the Manual Ability Classification System are used to describe mobility and manual dexterity in people with cerebral palsy, and recently the Communication Function Classification System, and the Eating and Drinking Ability Classification System have been proposed to describe those functions.
- There are three main CP classifications by motor impairment: spastic, ataxic, and athetoid/dyskinetic.
- Additionally, there is a mixed type that shows a combination of features of the other types. These classifications reflect the areas of the brain that are damage.
According to the topographic distribution :

- Cerebral palsy is also classified according to the topographic distribution of muscle spasticity.
- This method classifies children as diplegic, (bilateral involvement with leg involvement greater than arm involvement)
- Hemiplegic (unilateral involvement)
- Quadriplegic (bilateral involvement with arm involvement equal to or greater than leg involvement).
Spastic CP :

- Spastic cerebral palsy, or cerebral palsy where spasticity (muscle tightness) is the exclusive or almost exclusive impairment present, is by far the most common type of overall cerebral palsy, occurring in upwards of 70% of all cases.
- People with this type of CP are hypertonic and have what is essentially a neuromuscular mobility impairment (rather than hypotonia or paralysis) stemming from an upper motor neuron lesion in the brain as well as the corticospinal tract or the motor cortex .
- This damage impairs the ability of some nerve receptors in the spine to receive gamma-Aminobutyric acid properly, leading to hypertonia in the muscles signaled by those damaged nerves.[citation needed]
- As compared to other types of CP, and especially as compared to hypotonic or paralytic mobility disabilities, spastic CP is typically more easily manageable by the person affected, and medical treatment can be pursued on a multitude of orthopedic and neurological fronts throughout life.
- In any form of spastic CP, clonus of the affected limb(s) may sometimes result, as well as muscle spasms resulting from the pain or stress of the tightness experienced.
- The spasticity can and usually does lead to a very early onset of muscle stress symptoms like arthritis and tendinitis, especially in ambulatory individuals in their mid-20s and early-30s.
- Occupational therapy and physical therapy regimens of assisted stretching, strengthening, functional tasks, or targeted physical activity and exercise are usually the chief ways to keep spastic CP well-managed.
- If the spasticity is too much for the person to handle, other remedies may be considered, such as antispasmodic medications, botulinum toxin, baclofen, or even a neurosurgery known as a selective dorsal rhizotomy (which eliminates the spasticity by reducing the excitatory neural response in the nerves causing it).]
- Botulinum toxin is effective in decreasing spasticity.
- It can help increase range of motion which could help mitigate CPs effects on the growing bones of children.
- There is an improvement in motor functions in the children and ability to walk.
Ataxic CP :
- Ataxic cerebral palsy is observed in approximately 5-10% of all cases of cerebral palsy, making it the least frequent form of cerebral palsy.
- Ataxic cerebral palsy is caused by damage to cerebellar structures.
- Because of the damage to the cerebellum, which is essential for coordinating muscle movements and balance, patients with ataxic cerebral palsy experience problems in coordination, specifically in their arms, legs, and trunk.
- Ataxic cerebral palsy is known to decrease muscle tone.
- The most common manifestation of ataxic cerebral palsy is intention (action) tremor, which is especially apparent when carrying out precise movements, such as tying shoe laces or writing with a pencil.
- This symptom gets progressively worse as the movement persists, making the hand shake.
- As the hand gets closer to accomplishing the intended task, the trembling intensifies, which makes it even more difficult to complete.
Athetoid CP :

- Athetoid cerebral palsy or dyskinetic cerebral palsy (sometimes abbreviated ADCP) is primarily associated with damage to the basal ganglia and the substantia nigra in the form of lesions that occur during brain development due to bilirubin encephalopathy and hypoxic-ischemic brain injury.ADCP is characterized by both hypertonia and hypotonia, due to the affected individual’s inability to control muscle tone.
- Clinical diagnosis of ADCP typically occurs within 18 months of birth and is primarily based upon motor function and neuroimaging techniques.
- Athetoid dyskinetic cerebral palsy is a non-spastic, extrapyramidal form of cerebral palsy.
- Dyskinetic cerebral palsy can be divided into two different groups; choreoathetoid and dystonic.
- Choreo-athetotic CP is characterized by involuntary movements most predominantly found in the face and extremities.
- Dystonic ADCP is characterized by slow, strong contractions, which may occur locally or encompass the whole body.
Mixed :
- Mixed cerebral palsy has symptoms of athetoid, ataxic and spastic CP appearing simultaneously, each to varying degrees, and both with and without symptoms of each.
- Mixed CP is the most difficult to treat as it is extremely heterogeneous and sometimes unpredictable in its symptoms and development over the lifespan .
Prevention :
- Because the causes of CP are varied, a broad range of preventative interventions have been investigated.
In those at risk of early delivery,
- Magnesium sulphate appears to decrease the risk of cerebral palsy.
- It is unclear if it helps those who are born at term. In those at high risk of preterm labor a review found that moderate to severe CP was reduced by the administration of magnesium sulphate, and that adverse effects on the babies from the magnesium sulphate were not significant.
- Mothers who received magnesium sulphate could experience side effects such as respiratory depression and nausea.
- However, guidelines for the use of magnesium sulfate in mothers at risk of preterm labour are not strongly adhered to
prematurity

- Caffeine is used to treat apnea of prematurity and reduces the risk of cerebral palsy in premature babies, but there are also concerns of long term negative effects.
- A moderate quality level of evidence indicates that giving women antibiotics during preterm labor before her membranes have ruptured (water is not yet not broken) may increase the risk of cerebral palsy for the child.
- Additionally, for preterm babies for whom there is a chance of fetal compromise, allowing the birth to proceed rather than trying to delay the birth may lead to an increased risk of cerebral palsy in the child.
- Corticosteroids are sometimes taken by pregnant women expecting a preterm birth to provide neuroprotection to their baby.
- Taking corticosteroids during pregnancy is shown to have no significant correlation with developing cerebral palsy in preterm births.
- Cooling high-risk full-term babies shortly after birth may reduce disability, but this may only be useful for some forms of the brain damage that causes CP.
- A woman who is planning to become pregnant should ensure that all her vaccinations are up-to-date.
Treatment in Cerebral Palsy :
During pregnancy, it is important to:
- Attend all antenatal appointments
- Avoid alcohol, tobacco, and illegal drugs
- Carry out regular exercise, according to the physician’s advice
- Eat healthily
- For second or subsequent pregnancies, it may be useful to identify potential Rh incompatibility, as this can increase the risk of cerebral palsy.
- There is no cure for cerebral palsy, but treatment can help manage symptoms and increase independence.
- When a child receives a diagnosis of cerebral palsy, a team of health professionals will help to look after their needs. The team may include a doctor, a pediatrician, a speech therapist, and an educational psychologist, among others.
- An individual care plan will address the needs of the child and the family.
- As the child gets older, the plan will be reviewed and revised.
- Treatment depends entirely on individual needs.
- The aim is to help the child achieve as much independence as possible.
Age-related challenges :
Walking:
- Because cerebral palsy affects movement and flexibility, musculoskeletal abnormalities can worsen as the person ages.
- This may necessitate the use of mobility aids, such as a stick or wheelchair.
Swallowing problems:
- Known as dysphagia, problems with swallowing are common.
- They are generally caused by damage to the nerves in the neck or head. Symptoms can include coughing after eating or drinking,
- Food getting stuck in the mouth, pneumonia, weight loss, and poor nutrition. Working with a speech or physical therapist can help.
Premature aging:
- Although the total lifespan of individuals with cerebral palsy is similar to the general population, some signs of aging can arrive early.
- Because the condition puts additional strain on the body, there can be increased pain when, for instance, climbing the stairs.
- There is also an increased risk of dental problems, falls, and stiff muscles.
Post-impairment syndrome:
- This is caused due to the increased energy that it takes to move around.
- Symptoms include weakness, increased pain, repetitive strain injuries, and fatigue.
- Working with a therapist can help strengthen the muscles most affected by the condition.
Mental health conditions:
- Due to social stress, bullying, or teasing, individuals with cerebral palsy are more likely to become shy in social situations and have depression or anxiety disorders..
PHYSIOTHERAPY TREATMENT :
- A wide range of therapeutic interventions have been used in the treatment and management of children with cerebral palsy.
- They show that there is evidence to support the use and effectiveness of neuromuscular electrical stimulation, while evidence in support of the effectiveness of the neurodevelopmental treatment is equivocal at best
- The effectiveness of many other interventions, including include: sensory integration, body-weight support treadmill training, conductive education, constraint-induced therapy, hyperbaric oxygen therapy used in the treatment of cerebral palsy have not been clearly established based on well-controlled trials.
- We provides an overview of salient aspects of popular approaches and interventions used in the management of children with Cerebral Palsy.
Neurodevelopmental Treatment (NDT) :

- One of the more popular approaches utilised in the management of cerebral palsy, the NDT also know as Bobath Approach, The basis of this approach is that motor abnormalities seen in children with Cerebral Palsy are due to atypical development in relation to postural control and reflexes because of the underlying dysfunction of the central nervous system.
- This approach aims to facilitate typical motor development and function and to prevent development of secondary impairments due to muscle contractures, joint and limb deformities.
- Although the effectiveness of NDT in Cerebral Palsy has been questioned by some published reports, there are some studies suggesting its effectiveness.
Constraint-Induced Movement Therapy (CIMT) :
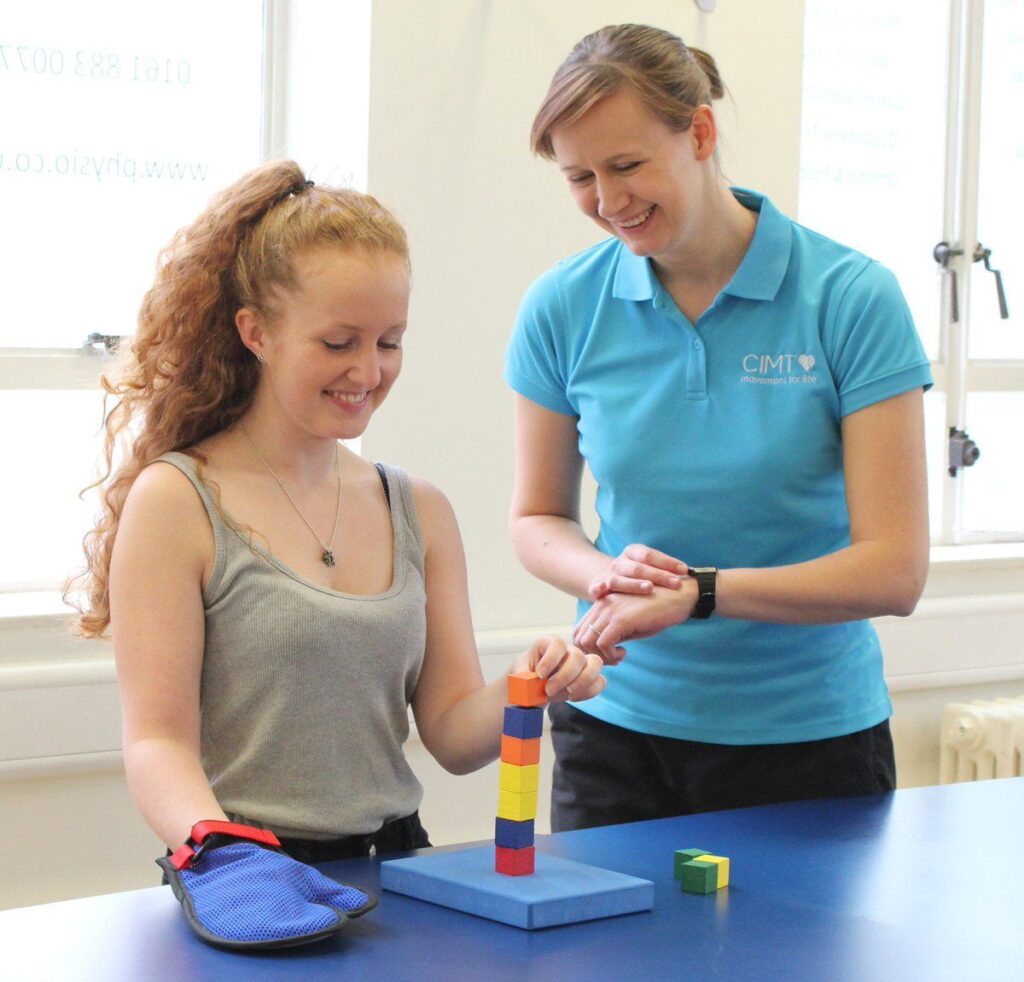
- Constraint-induced Movement therapy is used predominantly in the individual with Hemiplegic Cerebral Palsy to improve the use of the affected upper imb.
- The stronger or non-impairmed upper limb is immobilized for a variable duration in order to Force Use of the impried upper limb over time identified one high and one lower-quality trials which measured both body functions and structures, and activity and participation outcomes through use of CIMT.
- Use of a cast with CIMT showed positive effects in the amount and quality of functional hand use in th eimpaired limb and new emerging behavior as compared to the no-therapy group, but no effects were found on QUEST
- . Use of sling during CIMT also had positive effects on functional hand use on teh impaired upper limb, time to complete tasks, and speed and dexterity, but no effects on sensibility, handgrip force, or spasticity.
- Thus Antilla et al found there is moderate evidence for the effectiveness of CIMT therapy on functional hand use in th eimpaired upper limb .
- This approach has not been established, in particular in relation to the adverse effects of prolonged immobilization of the normally developing upper limb .
Patterning :
- The concept of patterning is based on theories developed during the 1950’s and 1960’s by Fay, Delacato, and Doman.
- Patterning is based on the principle that typical development of the infant and child progresses through a well-established, per-determined sequence’s; with failure to typically complete one stage of development causing inhibition or impairment in the development of subsequent stages.
- Based on this principal they suggested that in children with Cerebral Palsy typical motor development can be facilitated by passively repeating and putting the child through the sequential steps of typical development, a process called patterning
- Parents and other care givers are taught to carry out this patterning process at home but the approach is hugely labor intensive and time consuming as it requires multiple sessions every day.
- Although Patterning has been utilized for many years its use is now certainly controversial and the effectiveness has not been established.
- It is a very passive therapy, with little opportunity to encourage the child in their active involvement and its use in children with Cerebral Palsy is not recommended.
Physiotherapy exercise in Cerebral Palsy :
Passive Stretching :

- It is a manual application for spastic muscles to relieve soft tissue tightness.
- Manual stretching may increase range of movements, reduce spasticity, or improve walking efficiency in children with spasticity.
- Stretch may be applied in a number of ways during neurological rehabilitation to achieve different effects.
- The types of stretching used include;
- Fast / Quick
- Prolonged
- Maintained
- When we look at the use of stretch for facilitation we employ a fast/quick stretch.
- The fast/quick stretch produce a relatively short lived contraction of the agonist muscle and short lived inhibition of the antagonist muscle which facilitates a muscle contraction.
- It achieves its effect via stimulation of the muscle spindle primary endings which resuts in reflex reflex facilitation of tech muscle via the monosynaptic reflex arc.
- The presence of increased tone can ultimately lead to joint contracture and changes in muscle length.
- When we look at the use of stretch to normalize tone and maintain soft tissue length we employ a slow, prolonged stretch to maintain or prevent loss of range of motion.
- While the effects are not entirely clear the prolonged stretch produces inhibition of muscle responses which may help in reducing hypertonus, e.g. Bobath’s neuro-developmental technique, inhibitory splinting and casting technique.
- It appears to have an influence on both the neural components of muscle, via the Golgi Tendon Organs and Muscle Spindles, and the structural components in the long term, via the number and length of sarcomeres.
Muscle Immobilized Shortened Position = Loss of Sacromeres and Increased Stiffness related to increase in connective tissue
Muscle Immobilized Lengthened Position = Increase Sacromeres
- Studies in Mice show that a stretch of 30 mins daily will prevent the loss of sacromeres in the connective tissue of an immobilized muscle, although the timescale in humans may not relate directly.
Manual Stretching :
- Prolonged manual stretch may be applied manually, using the effect of body weight and gravity or mechanically, using machine or splints.
- Stretch should provide sufficient force to overcome hypertonicity and passively lengthen the muscle.
- Unlikely to provide sufficient stretch to cause change in a joint that already has contracture.
Weight Bearing :

- Weight-bearing has been reported to reduce contracture in the lower limb through use of Tilt-tables, and standing frames through a prolonged stretch.
- Angles are key to ensure the knees remain extend during the prolonged stretch as the force exerted on the knee can be quite high.
- Some research also challenges the assumption of the benefits of prolonged standing.
Splinting :

- Splints and casts are external devices “Splints and casts are external devices designed to apply, distribute or remove forces to or from the body in a controlled manner to perform one or both basic functions of control of body motion and alteration or prevention in the shape of body tissue.”
- Splinting can be used to produce low-force, long duration stretching although there is a dearth of evidence to support this.
- A wide range of splint have been used to influence swelling ,resting posture, spasticity, active and passive ROM.
Static Weight-bearing Exercises in Cerebral Palsy :
- Stimulation of anti gravity muscle strength, prevention of hip dislocation, reduction in spasticity and improvements in bone mineral density, self-confidence and motor function have all been achieved through the use of Static Weigh Bearing exercises such as Tilt-Table and Standing Frame.
Muscle Strengthening Exercises :
- It aims to increase the power of weak antagonist muscles and of the corre- sponding spastic agonists and to provide the functional bene ts of strengthening in children with CP.
Functional Exercises :
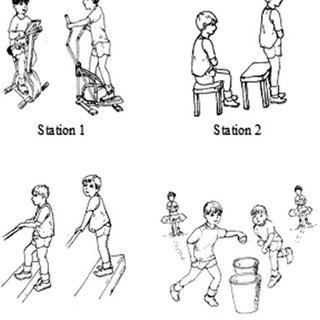
- Training related to specific functional activities combining aerobic and anaerobic capacity and strength training in ambulatory children, has been shown to significantly improve overall physical fitness, the intensity of activities, and quality of life.
- Training programs on static bicycles or treadmill have been shown to be beneficial for gait and gross motor development but have not shown to have any impact on spasticity or abnormal movement patterns.
Body Weight Supported Treadmill Training :

- Stepping movements from Reflex Stepping Reactions are normally present in newborns and infants, before the infant starts to bear weight, stand and walk. Body Weight Supported Treadmill Training, is achieved through supporting the child in a harness on the treadmill in an upright posture limiting overall weight bearing, on a slow moving treadmill, eliciting the stepping movements.
- Treadmill training, thus allows development of stepping movements needed for ambulation.
- Studies using 3-4 sessions per week lasting for 3-4 months have shown improvement in lower extremity movements and gait patterns in children with cerebral palsy.
Electrical Stimulation for Cerebral Palsy :
- The goal of the electrical stimulation is to increase muscle strength and motor function.
- Electrical stimulation is provided by Transcutaneous Electrical Nerve Stimulation (TENS) Unit which is portable, non-invasive and can be used in the home-setting by parents or the patient.
- Neuromuscular Electrical Stimulation (NMES) involves application of transcutaneous electrical current that results in muscle contraction.
- NMES has been postulated to increase muscle strength by increasing the cross-sectional area of the muscle and by increased recruitment of type 2 muscle fibers. Functional Electrical Stimulation (FES) refers to the application of electrical stimulation during a given task or activity when a specific muscle is expected to be contracting. has shown there is some evidence to support the use and effectiveness of NMES in children with Cerebral Palsy but found that many of the studies are limited by confounding variables including concomitant use of other therapies, wide variation in methods of application, heterogeneity of subjects, difficulty in measuring functional outcomes and lack of control subjects .
- Mintage proposes that neuromuscular and threshold electrical stimulation as a modality in Cerebral Palsy is used for strengthening the quadriceps muscles in ambulatory diplegic children with Cerebral Palsy, who have difficulty with specific resistive strength training .
Hippotherapy :
- Gross Motor Function including Muscle tone, Range of Movement, Balance, Coordination and Postural Control in children with CP have been shown to improve with Therapeutic horse-back riding which may reduce the degree of motor disability.
- Many none physical benefits may also be developed through enjoyment and providing a setting for increased social interaction, cognitive and psychosocial development .
- Sharan et al have noted satisfactory results with Hippotherapy in Bangalore, especially in post-surgical rehabilitation . There is limited evidence available with two lower-quality trials on saddle riding on a horse found no between-group differences in muscle symmetry or in any of the seven different outcome measures, except on a sub-item of grasping.
Importance of physiotherapy for cerebral palsy :
Physiotherapy treatment can improve :
- Coordination
- Balance
- Strength
- Flexibility
- Endurance
- Pain management
- Posture
- Gait
- Overall health
- The types of exercises used vary and have specific benefits for each type of cerebral palsy.
- Some of the benefits by cerebral palsy type include:
Spastic Cerebral Palsy:
- Physiotherapy stretching exercise can reduce the muscle tension and jerky movements associated with spastic cerebral palsy.
- Exercises such as stretching can even relieve stiffness over time.
Athetoid :
People with athetoid cerebral palsy use physical therapy to increase muscle tone and gain more control over their movements.
Ataxic :
There are exercises that can improve balance problems faced by those with ataxic cerebral palsy.
- Physiotherapists also tailor treatment based on the location of movement issues.
- Movement issues in children with cerebral palsy can be limited to one half of the body (hemiplegia), the legs (diplegia) or in the torso and all four limbs (quadriplegia).
- Therapists prescribe special exercises and routines for hemiplegia, diplegia and quadriplegia that may help the child regain movement in the affected area over time.
- physiotherapy can also treat a range of other issues experienced by children with CP, including:
- Scoliosis – an abnormal curvature in the spine, common in up to 30 percent of children with cerebral palsy
- Thoracic kyphosis – a contortion of the upper spine
- Lumbar lordosis – a contortion of the lower spine
- Pelvic inclination – a protrusion of the pelvis either in the front or rear
- Pelvic rotation – a horizontal contortion of the pelvis
- Pelvic obliquity – a contortion of the pelvis at angle
- Knee deformity – abnormally straight or bent knees that may be caused by pelvic deformities
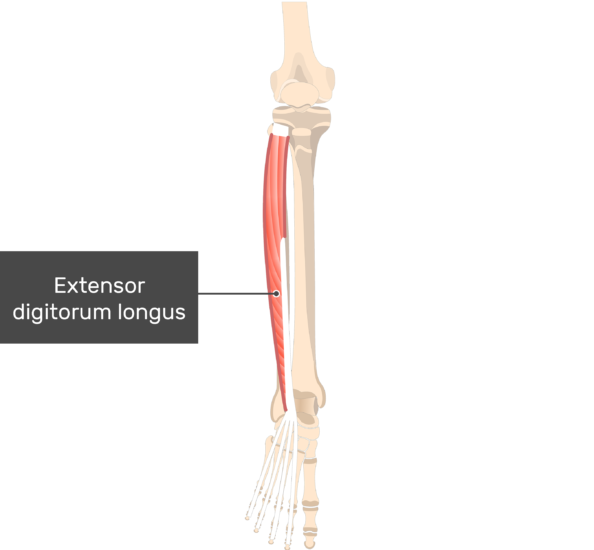
- Shortened Achilles tendon – a shortened tendon that causes issues with walking and standing
- Hand and wrist deformities – abnormal flexing in the hand and wrist that prevents development of fine motor skills.
- Physiotherapy is different for every child with cerebral palsy.
- First, the therapist has to evaluate the child’s movement problems to create a treatment plan.
- Then, generally, a combination of exercises, muscle relaxing techniques and special equipment is used to improve movement.
- The degree to which physical therapy can improve a child’s specific issues depends on the severity of the condition.
Exercises :
- Exercises for cerebral palsy are geared toward treating either high or low muscle tone.
- High muscle tone causes stiffness and spasticity, whereas low muscle tone causes too much flexibility and weakness.
Improving muscle tone :
- Flexibility exercises and massages are often used for children with spastic cerebral palsy;
- These exercises not only help improve mobility, but also can prevent painful muscle tightening that could require surgical correction.
- Strength training exercises are used to increase muscle tone in children with athetoid cerebral palsy.
Assisting posture and walking :
- Special exercises are also used to help with walking, posture, transitional movements and sensory impairments like touch and balance.
- Posture is improved through exercises that emphasize sitting, kneeling and standing.
- Transitional movements are those used by infants that lead to walking, such as rolling over and sitting up.
Equipment :
- Physiotherapists use a range of mobility aids to make therapy more effective.
- Braces, casts, splints and shoe inserts are types of orthotic equipment used to help with walking, posture and joint mobility.
- Exercise balls
- Resistance bands
- Free weights
- Swimming pools
- Hot and cold packs
- Electric muscle stimulation
- In some cases, electric stimulation is used to improve gait and upper limb function. This therapy uses small electrodes to stimulate certain muscles.
Physiotherapy by Age :
- As children get older, their physiotherapy needs change.
- Physiotherapists have to adjust and adapt treatments at different stages in development. T
- he most important stages are when the child is a toddler and in the early school years.
Toddlers :
- Therapy for toddlers tends to focus on playtime.
- Children in early developmental stages learn and experience a lot through play, making it an important aspect of early therapy.
- Toddlers with CP are often reluctant to touch their face or practice certain movements that are necessary for learning and physical development.
- A therapist can help children overcome this reluctance.
- Young children – During school age, roughly ages 5 to 12, children with cerebral palsy experience new movement issues in part because their bodies are growing.
- Physical therapy can help ensure children grow in a way that is conducive to their motor function.
- Exercises and orthotics are most commonly used at this age.
- Therapy also helps instill healthy habits and a proactive mindset.




29 Comments