List of Pediatric conditions related to Physiotherapy
A list of Pediatric conditions related to Physiotherapy are:
(1) Cerebral palsy
(2) Developmental delay
(3) Torticollis
(4) Cystic fibrosis
(5) Developmental coordination disorder
(6) Hypotonia
(7) Hip dysplasia
(8) Flat feet
(9) Fracture
(10) Childhood walking abnormalities
(11) Growing pains
(12) Benign joint hypermobility syndrome
(13) Joint pains
(14) Juvenile arthritis
(15) Perthes disease
(16) Post concussion syndrome
(1) Cerebral palsy: loss or impairment of motor function, Cerebral Palsy is actually caused by brain damage. Brain damage is caused by brain injury or abnormal development of the brain that occurs while a child’s brain is still developing — before birth, during birth, or immediately after birth. Cerebral Palsy affects body movement, muscle control, muscle coordination, muscle tone, reflex, posture and balance. It can also impact fine motor skills, gross motor skills and oral motor functioning.
Physiotherapy :
Passive Stretching
Manual Stretching
Weight Bearing
Splinting
Serial Casting
Static Weight-bearing Exercises
Muscle Strengthening Exercises
Functional Exercises
Body Weight Supported Treadmill Training
Electrical Stimulation
Hippotherapy
(2) Developmental delay: The condition of a child being less developed mentally or physically than is normal for its age.
Physiotherapy :
Physiotherapists are mainly concerned with the development of body postures and large movements (gross motor skills).
improve their gross motor skills by helping them to strengthen weak muscles, learn patterns of movement and integrate their sensory systems.
exercises to improve their posture, muscle strength and co-ordination.
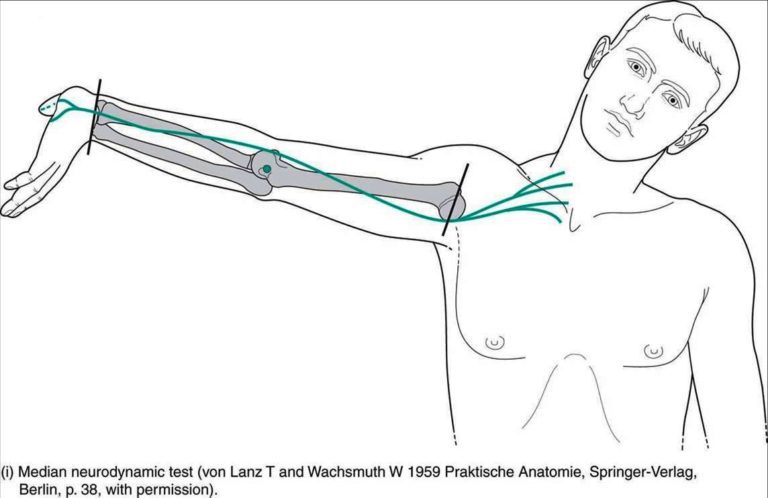
(3) Torticollis: Torticollis, also known as wry neck, is a dystonic condition defined by an abnormal, asymmetrical head or neck position,
which may be due to a variety of causes.
physiotherapy :
- Massage: Massage can relax the muscle preceding the stretching manoeuvres.
- Thermo Therapy Modality: Carefully administered thermo-therapy modality induces relaxation.
- Passive movements: The child is placed in a supine position with the head beyond the edge of the table with the neck in extension by positioning a pillow under the thoracic region; Shoulders are stabilized by an assistant. To attain relaxation, all the movements of the cervical spine are done in a form of slow relaxed passive movements.
This should be followed by sustained passive stretching to the affected sternomastoid. E.g. when the right sternomastoid is involved the head should be gradually bent inside flexion to the left, held there for a while and then rotated gradually to the right. Try to gain as much overcorrection as possible by applying gradual traction to gain further stretching.
Maintenance of Correction: Once the correction is achieved. It has to be maintained by passively holding or keeping a sandbag.
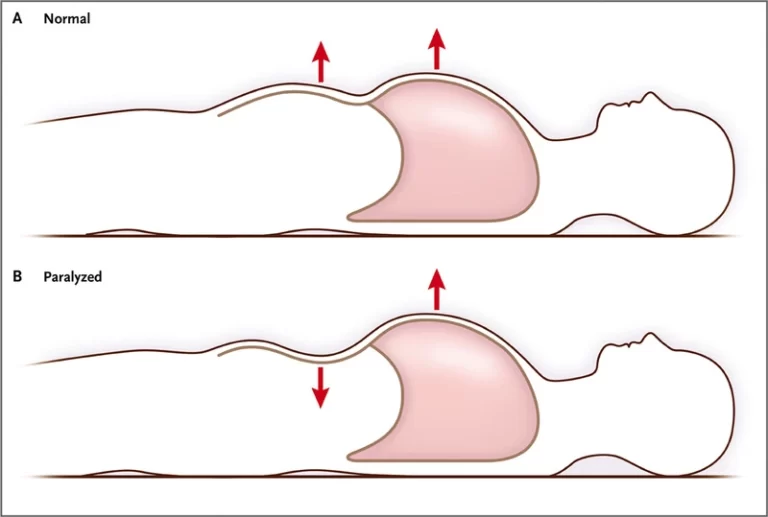
(4) Cystic fibrosis: Cystic fibrosis is a progressive, genetic disease that causes persistent lung infections and limits the ability to breathe over time. In people with CF, mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene cause the CFTR protein to become dysfunctional.
physiotherapy :
Manual chest physical therapy (CPT) is the traditional airway clearance technique for cystic fibrosis (CF) patients.
The removal of obstructive, thick sticky secretions is important in preventing infections and helps ease breathing.
Manual chest physiotherapy consists of two parts: Postural drainage.
(5) Developmental coordination disorder: DCD occurs when a delay in the development of motor skills, or difficulty coordinating movements, results in a child being unable to perform common, everyday tasks.
By definition, children with DCD do not have an identifiable medical or neurological condition that explains their coordination problems.
physiotherapy :
Improving strength: Your physical therapist will teach you and your child exercises to increase muscle strength. The therapist will identify games and fun tasks that improve strength, reduce obesity, and increase cardiac health.
Improving balance: Your therapist may use equipment such as a balance beam to improve your child’s one-foot standing, walking with one foot directly in front of the other foot, and jumping to the floor.
Improving body awareness: Your physical therapist might have your child participate in obstacle courses to help your child with learning how to plan movement.
Improving skills through task-oriented and task-specific learning. Your physical therapist may work individually with you or recommend a community program to help your child learn a specific task such as bike riding. The therapist may suggest adaptations, such as a 3-wheeled bike or training wheels, to keep your child safe while accomplishing a new skill.
(6) Hypotonia: Hypotonia, commonly known as a floppy baby syndrome, is a state of low muscle tone (the amount of tension or resistance to stretch in a muscle), often involving reduced muscle strength.
physiotherapy :
Proximal Strength and Support in order to Facilitate Distal Strength and Function
Improve Postural Control
Facilitate Motor Development and Foundations of Motor Planning
Improve Postural Responses and Protective Reactions
Address Fluidity and Efficiency of Movements
Improve Functional Strength
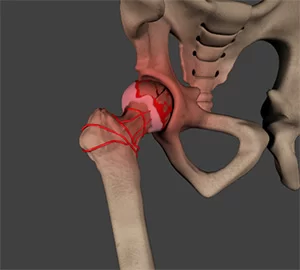
(7) Hip dysplasia: Developmental dysplasia of the hip (DDH) is a condition where the “ball and socket” joint of the hip does not properly form in babies and young children. It’s sometimes called congenital hip dislocation or hip dysplasia. The hip joint attaches the thigh bone (femur) to the pelvis.
physiotherapy :
Movements of the hip and gentle stretching exercises are recommended because motion may help lubricate and nourish the joint surfaces.
Stretching exercises can be performed to move your leg away from your body in the lying position and in the sitting position
When working on hip strengthening exercises concentrate on hip abduction.
(8) Flat feet :
Flat feet, also called pes planus, is a deformity that occurs when the arch of the foot collapses and comes into complete or near-complete contact with the ground.
The condition may be congenital (occurring at the time of birth) or acquired (developing over time, most often as a result of age or injury).
physiotherapy :
Arch muscle strength exercise. Sit down and cross your involved foot over the other thigh.
Toe curls. Sit up straight in a chair with a towel placed under your forefoot.
Heel raised with scrunch.
Calf stretch.
Plantar fascia stretch.
Plantar fascia muscle release.
(9) Fracture: The bones of a child are more likely to bend than to break completely because they are softer and the periosteum is stronger and thicker. The fractures that are most common in children are the incomplete fractures; these fractures are the greenstick and torus or buckle fractures.
physiotherapy :
Your physiotherapist will work closely with you and your child to ensure the treatment plan is designed to meet your child’s needs and fit within their other commitments. At Physio.co.uk we are able to offer a comprehensive package which uses the most up-to-date evidence-based treatment options available. Listed below are some of the key treatments that we can offer please click on the link for more details.
Electrotherapy
Strengthening exercises
Hydrotherapy
Gait training
Musculoskeletal physiotherapy
Strengthening Exercises
Intensive Rehabilitation
(10)childhood walking abnormalities: 1-year-old wobble around, and you’ll see her gait, or walking cycle, doesn’t quite resemble that of an adult. She’ll have a wider stance, rapid cadence and short steps. In fact, it takes until.
• During your child’s first few years of walking, they may have an obvious gait
abnormalities—disturbances in what is considered the normal walking cycle
for that age group
• The most common types of gait abnormalities are intoeing, outtoeing, limping
and toe walking
• Many gait disturbances are common and correct themselves on their own
• Gait disturbances rarely require medical assistance
physiotherapy:
Increase independence
Enable more participation at school
Increase confidence
Reduce fatigue
Sense of achievement
Reduce care needs
Increase ability to exercise
More efficient walking patterns
Decrease reliance on walking aids
Holistic services meeting all your child’s needs
(11)Growing pains: Growing pains are cramping, and achy muscle pains that some preschoolers and preteens feel in both legs. The pain usually occurs in the late afternoon or evening. But it may cause your child to wake up in the middle of the night. Growing pains usually start in early childhood, around age 3 or 4.
physiotherapy: Repeat several times. Lying on her tummy, get your child to bend her leg to 90 degrees at the
the knee then pushes the front of your child’s foot down to stretch out her calves. Hold for a few seconds and repeat.
Your child lies on her back and you lift each leg gently by the heel to stretch out the hamstring.
(12)Bening joint hypermobility syndrome: Bening joint hypermobility syndrome means your joints are “looser” than normal. It’s typically referred to as being double-jointed. It is a common joint or muscle problem in children and young adults.
physiotherapy: Joint hypermobility can sometimes be developed, for example by gymnasts and athletes, through the training exercises they do. Yoga can also make the joints more supple by stretching the muscles.
(13)Joint pains: Joint pain refers to discomfort, aches, and soreness in any of the body’s joints. … Sometimes, joint pain is the result of an illness or injury. Arthritis is also a common cause of joint pain. However, it can also be due to other conditions or factors.
Physiotherapy: Joint mobilisation & soft tissue techniques. Hands-on treatment to joints and muscles can help reduce pain and allow the body to start to move more freely. Physiotherapists may use these techniques on patients alongside other treatment approaches such as exercise therapy to help patients get better quicker.
(14)Juvenile arthritis: Juvenile idiopathic arthritis, also known as juvenile rheumatoid arthritis, is the most common form of arthritis in children and adolescents. . JIA is an autoimmune, noninfective, inflammatory joint disease of more than 6 weeks duration in children less than 16 years of age.
Physiotherapy: the body produces endorphins during exercise, which help to reduce pain, joint stiffness and anxiety.
Different types of exercise include a range of motion, stretching, strengthening and cardiovascular fitness.
(15)Perthes disease: Perthes disease is a rare childhood condition that affects the hip. It occurs when the blood supply to the rounded head of the femur (thighbone) is temporarily disrupted. Without an adequate blood supply, the bone cells die, a process called avascular necrosis.
Physiotherapy: Relieving Pain
• Hot Pack for pain management with stretching
• Cryotherapy for 20min at a time
Increasing Strength
• Hip abductors
• Hip flexors
• Hip extensors
• Hip internal & external rotators
• Gluteus medius
**Avoid single-limb stance activities due to increased force through the hip joint during the severe involvement stage
Improving Range of Motion
**ROM is typically lost in this population due to muscle guarding secondary to pain from incongruent joint surfaces
• Static Stretching of LE musculature
• Dynamic ROM and AAROM for muscle guarding due to pain and if unable to achieve through static stretching
• AROM & AAROM following passive stretching to maintain newly gained ROM
• Stretching should include the following muscle groups: hip internal and external rotators, hip abductors, hip extensors, and any other LE motion that is significantly limited.
Functional Activities
• Single leg dynamic function activities such as side steps and step-ups, according to WB status and involvement phase
Home Exercise/Modality Use
• Cryotherapy for 20min at a time may be used to decrease pain and inflammation
• The HEP should be based on orthopedist recommendations due to the staging of the disease, age of onset of the disease, radiographic data, and patient presentation
(16)Post-concussion syndrome: Post-concussion syndrome is a complex disorder in which various symptoms — such as headaches and dizziness — last for weeks and sometimes months after the injury that caused the concussion. A concussion is a mild traumatic brain injury that usually happens after a blow to the head.
Physiotherapy: Exercising regularly, especially aerobic exercise, is crucial for recovery because it increases blood flow to the brain, bringing vital nutrients to your brain. Exercise also activates neuroplasticity, which as we mentioned earlier, will help you restore lost function.