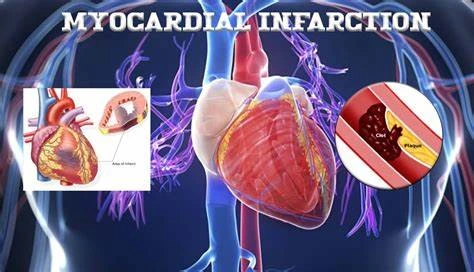
Myocardial Infarction (Heart attack)
Table of Contents
What is myocardial infarction (Heart attack)?
- Acute myocardial infarction, also called a heart attack, is a life-threatening condition that occurs when blood flow to the heart muscle is abruptly cut off, causing tissue damage.
- This is commonly the result of a blockage in one or more of the coronary arteries. A blockage can create due to a buildup of plaque, a substance mostly made of fat, cholesterol, & cellular waste products, or due to a sudden blood clot that forms on the blockage.
- A heart attack (medically known as a myocardial infarction) is a deadly medical emergency where your heart muscle starts to die because it is not getting enough blood flow. A blockage in the arteries that supply blood to your heart commonly causes this.
- If a healthcare provider does not restore blood flow quickly, a heart attack can cause permanent heart damage & death.
- Myocardial Infarction(MI) also known as heart attack is one of the most usual non-communicable diseases/ chronic diseases, which cannot be transmitted from person to person. It gradually progresses and harms the blood supply to the heart.
- A myocardial infarction is a serious medical emergency that happens due to the blockage of one of the arteries which are supplying blood to the heart. Due to this, a decrease in oxygen to the heart causes characteristic chest pain and death of myocardial tissue.
What are the symptoms of myocardial infarction?
While the classic symptoms of a heart attack are chest pain and shortness of breath, the symptoms can be quite different. The most common symptoms of a heart attack include trusted sources:
- pressure or tightness in the chest
- pain in the chest, back, jaw, and other areas of the upper body that lasts more than some minutes or that goes away & comes back
- shortness of breath
- sweating
- nausea
- vomiting
- anxiety
- feeling like you are going to faint
- a fast heart rate
- sense of impending doom.
It is important to note that not all patients who have heart attacks feel the same symptoms or the same severity of symptoms. Chest pain is the most usually reported symptom among both women and men. However, women are a bit more likely rested source than men to have more of the “atypical” symptoms, such as:
- shortness of breath
- jaw pain
- upper back pain
- lightheadedness
- nausea
- vomiting.
In fact, certain women who have had a heart attack report that their symptoms felt like the symptoms of the flu.
What causes myocardial infarction?
- Your heart is the main organ in your cardiovascular system, which also involves different types of blood vessels. Certain of the most important vessels are the arteries. They take the oxygen-rich blood to your body & all of your organs.
- The coronary arteries take the oxygen-rich blood specifically to your heart muscle. When these arteries become blocked or narrowed due to the buildup of plaque, the blood flow to your heart can decrease significantly or stop completely. This can cause a heart attack.
Who is at risk for myocardial infarction?
- A major trigger for heart problems can beTrusted the Source of the fat content of food. People who eat a lot of processed and fried foods, as well as certain meat and dairy foods that contain unhealthy saturated and trans-saturated fats, are at a higher risk for heart disease. Obesity can increase this risk.
- According to one study, replacing a two percent trusted Source of calories consumed from carbs with trans fat could double the risk of heart disease.
- In addition, your blood also contains a fat called triglycerides, which store trusted Source excess energy from the food that you eat. When the level of triglycerides in your blood increases, you may be at high risk for cardiovascular disease.
- If along with that, you have a high level of low-density lipoprotein (LDL) in your blood, your risk may be even higher. This is because low-density lipoprotein (LDL) cholesterol can stick to the walls of your arteries & produce plaque, a hard substance that blocks trusted source blood flow in the streets.
- Reducing your cholesterol and the unhealthy fat in your body commonly requires eating a balanced diet containing few processed foods and taking medications called statins when necessary.
- Your doctor would be able to recommend the best nutrition plan for you & determine whether you require to take medications.
Additional risks
In addition to your diet, the following factors can increase your risk of heart problems trusted Source:
- High blood pressure: This can damage your arteries & accelerate the buildup of plaque.
- High blood sugar levels: Having high levels of blood sugar can damage blood vessels and eventually leads to coronary artery disease.
- Smoking: Smoking may increase your risk for heart attack and leads to other cardiovascular conditions and diseases.
- Age: The risk of having a heart attack increases with the age. Men are at a higher risk of a heart attack later age 45, and women are at a higher risk of a heart attack later age 55.
- Sex: Not only do men have a significantly higher risk of having a heart attack than women, yet they also often have heart attacks earlier in life.
- Family history: You are more likely to have a heart attack if you have a family history of early heart disease. Your risk is exceptionally high if you have male family members who developed heart disease previous age 55 or if you have female family members who developed heart disease before age 65.
- Stress: Although the evidence for this is still limited, stress may also trust a Source to be a trigger for acute myocardial infarction: Reducing chronic anxiety or stress can assist reduce the risk of a heart attack and other heart problems over time.
- Physical inactivity: Getting regular exercise can assist keep your heart healthy by helping you maintain moderate weight, as well as reduce your blood pressure, cholesterol, and blood sugar levels.
- Drug use: The use of certain drugs, including cocaine & amphetamines, can tiny the blood vessels, which could increase the risk of a heart attack.
- Preeclampsia: If you have a history of preeclampsia or high blood pressure during pregnancy, you may be at a higher risk of developing heart problems after in life.
How is myocardial infarction diagnosed?
- To determine whether you have had a heart attack, your doctor will look over the history of your symptoms, as well as your vital signs like as your blood pressure. Your doctor will then complete a physical exam with specific attention to the heart.
- Your doctor will also run a number of various tests if they suspect that you have had a heart attack. An electrocardiogram (EKG) may be done to measure your heart’s electrical activity.
- Blood tests will also be used to check for proteins that are associated with heart damage, like troponin.
- Your doctor may also perform an angiogram with coronary catheterization to look for parts of the blockage in your arteries.
ECG
- 12-lead electrocardiogram (ECG) showing ST-segment elevation in I and V1-V5 with reciprocal changes (blue) in the inferior leads, indicative of an anterior wall myocardial infarction. The 12-lead electrocardiogram (ECG) is used to classify patients into one of three groups:
- Those with ST-segment elevation or new bundle branch block,
- Those with ST-segment depression or T wave inversion (suspicious for ischemia), and
- Those with the so-called non-diagnostic or normal electrocardiogram (ECG). A normal electrocardiogram (ECG) does not rule out acute myocardial infarction (AMI).
- Errors in interpretation are relatively usual, and the failure to identify high-risk features has a negative harm on the quality of patient care.
Physical examination
- The appearance of patients may differ according to the symptoms. Cold and pale skin is usual and points to vasoconstriction.
- Certain patients have a low-grade fever (38–39 °C). Blood pressure may be increased or decreased, and the pulse can become irregular.
How is myocardial infarction treated?
- Heart attacks need immediate treatment, so most treatments begin in the emergency room. Treatment may involve taking medications to resolve blood clots, reduce pain, or slow down your heart rate.
- The doctor may also send you to undergo a minimally invasive procedure known as percutaneous coronary intervention (PCI), formerly referred to as an angioplasty with a stent. This procedure is used to unlock trusted sources of the arteries that supply blood to the heart.
- Only about 36 percent trusted Source of hospitals in the United States is equipped to perform this procedure. If your hospital cannot perform an angioplasty, they may transfer you to another hospital that can.
- During the procedure, your surgeon will insert a long, thin tube known as a catheter through your artery to reach the blockage. They will then inflate a little balloon attached to the catheter in order to reopen the artery, allowing blood flow to resume.
- Your surgeon may also place a tiny, mesh tube called a stent at the site of the blockage. The stent can cure the artery from closing again.
- Your doctor may want to perform a coronary artery bypass graft (CABG). In this procedure, your surgeon will restore blood flow by rerouting your veins & arteries so the blood can move around the blockage.
- A coronary artery bypass graft (CABG) is sometimes done immediately later a heart attack. In most cases, however, it is performed several days later the incident so your heart has time to heal.
- Another procedure your doctor may want you to undergo is a bypass surgery, which is used by trusted Sources to form new passages for blood to flow to the heart.
A number of various medications can also be used to treat a heart attack:
- Blood thinners, such as aspirin, are sometimes used to break up blood clots and improve blood flow through narrowed arteries.
- Thrombolytics are sometimes used to dissolve clots.
- Antiplatelet drugs, such as clopidogrel, can cure new clots from forming and existing clots from growing.
- Nitroglycerin can be used to broaden your blood vessels.
- Beta-blockers lower your blood pressure & relax your heart muscle. This can assist limit the severity of damage to your heart.
- ACE inhibitors can also be used to lower blood pressure & decrease stress on the heart.
- Pain relievers may be used to decrease any discomfort you may feel.
- Diuretics can assist decrease fluid buildup to ease the workload of the heart.
Physiotherapy treatment
Physiotherapy role in myocardial infarction treatment program:
- complete bed rest-up for up to two days.
- partial bed rest for up to four days.
- up and about in the hospital from the third or fourth day for up to two weeks.
- later discharge from the hospital: 3 weeks to 12 weeks.
- outpatient rehab: 3-9 months.
- Complete bed rest:
Aims of physiotherapy :
- to cure accumulation of secretion in the lungs.
- to cure deep vein thrombosis.
- to cure pressure sores.
- to teach & encourage relaxation.
- explain the purpose of the active rehabilitation program.
Techniques used in myocardial infarction treatment program: - relaxation: lying or half-lying, conscious relaxation ten min approx. Modified physiological relaxation may be indicated. If the patient can learn to relax, the heart rate is decreased and this aids recovery by easing the load on the heart.
2. breathing exercises: bilateral basal breathing- 3 times. There must be no forceful breathing. This will improve the oxygenation of the blood and therefore decreases the demand on the heart.
3. free active exercises: lying or half-lying
a. ankle pumps
b. foot turning in & out
c. fingers bending & stretching
d. wrists bending & stretching
4. breathing exercises: anterior basal expansion within patient’s normal pattern- three times.
5. passive movements
6. breathing exercises: posterior basal exercises- three times.
7. passive movements- repeat again
Partial bed rest:
The patient is up to sit for 1-2 hours per day. Feeding, and washing is allowed.
Aims of physiotherapy:
- to maintain clear lung fields.
- to increase the load on the heart like that there is hypertrophy of the myocardium.
- to educate the patient to recognize the signs & symptoms of excess exercise.
- to begin rebuilding the patient’s confidence.
- to train postural awareness.
- to strengthen leg and trunk exercises.
Example of myocardial infarction treatment program:
- half lying: relaxation- five minutes.
2. posterior basal breathing exercises.
3. half lying or lying.
alternate foot pulling up & pushing down feet circling, q-drill, gluteal contractions.
4. diaphragmatic breathing
5. high sitting: posture training.
6. half lying: lateral basal breathing.
7. lying: active exercises & stretching.
8. lying: relaxation & posture training.
9. crook lying should be done three times.
Up & about in the hospital:
The patient is allowed to wash, feed, go to the toilet & have a bath with supervision.
Aims of physiotherapy:
- To continue the promoting hypertrophy of the heart muscle to strengthen trunk & leg muscles.
2. To continue rebuilding patient confidence.
3. To improve exercise tolerance to teach awareness of exercise capacity.
Myocardial infarction treatment program:
- stop the formal relaxation.
2. stop the localized breathing exercises.
3. stride standing: holding bedrail or chair-knees & hips bending & stretching.
4. bend standing: elbow circling.
5. standing: arms raising forwards & upwards.
6. walk standing: one hip & knee bending forward and stretching.
7. standing: posture checking.
8. sitting: deep breathing exercises.
9. bend sitting: trunk bending & turning side to side.
10. progress each exercise.
11. improve confidence.
Myocardial infarction treatment Home Programme: General exercises
After discharge from the hospital:
- Home management will be given before leaving the hospital. The patient can progress the exercise a week to 10 days later discharged. Usually, the patient is advised not to drive the car till 4-8 weeks later discharge.
Out-patient rehabilitation:
- This is usually taken in the gymnasium. Patients benefit from meeting fellow patients in the group.
Equipment required:
- defibrillator
- suction apparatus
- oxygen
- electrocardiograph
Aims of physiotherapy:
- To increase exercise tolerance.
- To maintain or improve confidence.
- To provide support & encouragement.
- To assist reduce risk factors & thereby reduce recurrence.
- half-yard grasp standing-one leg swinging forward and backward then repeat with another leg.
- half yard grasp standing: knees & hip bending & stretching.
- yard standing: arms circling backward.
- yard standing: trunk bending & turning to the touch left knee.
- lying: alternate hip & knee bending & stretching.
- sitting: throwing and catching the ball.
- standing: arms bending and stretching.
- wing wide standing, trunk bending side to side.
- standing: stepping up and down.
- sitting, standing up, and sitting down.
- stride standing: bouncing ball.
- stride standing: throwing the ball.
- sitting: trunk turning side to side.
- crook lying-pelvis raising & lowering.
Progression:
- increase no. of repetitions.
- increase the length of the time for each exercise.
- increase speed.
- add weights.
- alter range.
Support & encouragement are necessary for Myocardial Infarction Treatment. Golf is a suitable sport to recommend.
Management after a heart attack
- Your chances of recovering from a heart attack turn on how much damage there is to your heart & how quickly you receive emergency care. The sooner you collect the treatment, the more likely you are to survive.
- Keep in mind that recovery is a long process and may take so many weeks or months later leaving the hospital. Later having a heart attack, you may be at a higher risk of having other heart problems in the future.
- For example, if there is substantial damage to your heart muscle, your heart may be unable to pump an adequate amount of blood throughout your body. This can conduct to heart failure. Heart damage increases your risk of valve problems & developing an abnormal heart rhythm or arrhythmia.
- Your risk of having another heart attack will be higher as well. In fact, it is estimated that one in 5 trusted Source people who have had a heart attack will be readmitted to the hospital for a second heart attack within 5 years.
- Many people experience trusted Source chest pain after having a heart attack, especially later eating a large meal or engaging in physical activity. Be sure to ask your doctor if you attend any chest pain. They can recommend certain medications or exercises to assist relieve symptoms.
- As part of your treatment plan, you may be needed a trusted Source to take medications or undergo a cardiac rehabilitation program. This type of program can assist you slowly regaining your strength, teach you about healthy lifestyle changes, & guide you through treatment.
Follow-up
- There are several ways to cure another heart attack and promote healing, including working with your doctor to make changes to your diet & lifestyle.
- It is also important to speak with your doctor about your concerns during recovery. Because many people who have had heart attacks often experience anxiety & depression, it may be beneficial to join a support group trusted Source or to speak with a counselor about what you are going through.
- Most people are able to resume their normal activities later after a heart attack. However, you will need to ease back into any intense physical activity. Your doctor will assist you to develop a specific plan for recovery.
How can myocardial infarction be prevented?
- In general, there are many things that you can do that may cure a heart attack. However, certain factors beyond your control — especially your family history — can still lead to a heart attack despite your best efforts.
- Still, decreasing your risk can postpone when you have a heart attack & reduce the severity if you have one.
- There are many steps you can take to cure a heart attack, even if you have had one before. One way to lower your risk is to eat a heart-healthy diet.
Trusted Source This diet should longly consist of:
- whole grains,
- vegetables,
- fruits,
- lean protein.
You should also try to decrease the following in your diet:
- sugar,
- processed foods.
- This is especially important for people with diabetes, high blood pressure, & high cholesterol. Exercising several times a week will improve your cardiovascular health.
- If you have had a heart attack recently, you should ask your doctor before starting a new exercise plan. It is also important to stop smoking if you smoke.
- Quitting smoking will significantly decrease your risk of a heart attack & improve both your heart & lung health. You should avoid being around secondhand smoke.
Takeaway
- Myocardial infarction, or heart attack, is a serious condition that happens when blood flow to the heart is cut off, which requires immediate medical treatment.
- Fortunately, there are many ways to cure complications associated with this condition & minimize the long-term effects on health.
- Not only can making changes to your diet and lifestyle promote recovery later in a heart attack, but it can also cure heart attacks from occurring again in the future.
FAQs
Heart Attack (Myocardial Infarction) Menu. A heart attack, or myocardial infarction (MI), is permanent damage to the heart muscle. “Myo” means muscle, “cardial” refers to the heart, and “infarction” means the death of tissue due to lack of blood supply. Your heart muscle needs to receive a good supply of blood at all times to function properly.
Myocardial infarction ( MI ), commonly known as a heart attack, occurs when blood flow decreases or stops in a part of the heart, causing damage to the heart muscle. The most usual symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck, or jaw.
The complete blockage of a coronary artery caused by a rupture of an atherosclerotic plaque is commonly the underlying mechanism of an MI. MIs are usually caused by coronary artery spasms, which may be due to cocaine, significant emotional stress, and extreme cold, among others.
This classifies myocardial infarctions into five types: [24] MI related to ischemia, like from increased oxygen demand or decreased supply, e.g. coronary artery spasm, coronary embolism, anemia, arrhythmias, high blood pressure, or low blood pressure.
If the ischemia lasts long enough, the heart muscle that is not getting enough oxygen dies. This is called an infarction. “Myocardial infarction” means “infarction (muscle death) in the heart muscle.”. A heart attack is a medical emergency.
Myocardial infarction. interruption of blood supply to a part of the heart. An acute myocardial infarction, also called a heart attack, happens when a blood vessel in the heart suddenly becomes blocked. Blood vessels carry blood and oxygen. When a blood vessel in the heart gets blocked, blood cannot get to a part of the heart.
Most MIs occur due to coronary artery disease. Risk factors include high blood pressure, smoking, diabetes, lack of exercise, obesity, high blood cholesterol, poor diet, and excessive alcohol intake.



9 Comments