Lou Gehrig’s Disease
Table of Contents
Introduction
Lou Gehrig’s disease, commonly known as, Amyotrophic lateral sclerosis (ALS) is a rare neurological disease that affects motor neurons—those nerve cells in the brain and spinal cord that control voluntary muscle movement.
Amyotrophic Lateral Sclerosis (ALS) is a rare neurological disease that includes the degeneration of neurons for controlling voluntary muscle action. Ultimately, many patients with ALS die within 3-5 years after symptom onset because of respiratory failure.
Definition
Amyotrophic lateral sclerosis (ALS) is a progressive neuromuscular disease that includes the neurons responsible for controlling voluntary muscle actions.
ALS usually appears between the ages of 55 to 75 but can impact a person within any age category. In ALS, both the upper motor neurons & lower motor neurons degenerate, & therefore, stop sending signals to the muscles. This interruption in signaling outcomes in the weakening of the muscles, twitching—called fasciculations—& muscle wasting. The initial symptoms commonly include muscle weakness & eventually progress to the unable to speak, eat, move, or breathe. Respiratory failure is the main reason for death in patients with ALS & commonly happens within 3 to 5 years from the onset of symptoms.
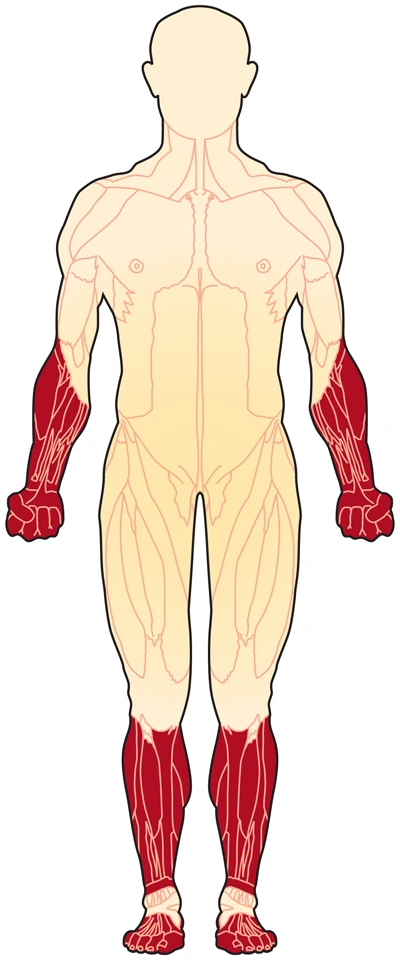
Approx 70 percent of individuals with ALS are found with limb-onset ALS—weakness in the arms & legs—& the residual individual is found with bulbar-onset ALS, which manifests with dysarthria which is motor speech disorder & dysphagia which is difficulty in swallowing. The sign and symptoms of ALS are not similar. There is considerable unevenness in the phenotypical expression of ALS, as shown throughout the literature. Jamorzik et al.discuss a 68-year-old male whom 1st presented with dysarthria in July 2012, & began suffering generalized fasciculations various months after. A year after, the patient’s speech became more slurred, but he did not found with muscular atrophy or weakness. Clinical evaluations supported by electrophysiological & biochemical testing led to the diagnosis of bulbar-onset ALS. Contrarily, Venizelos, Park & Fisher presented a case of 57-year-old Caucasian men who began suffering unexplained bilateral lower extremity weakness & fasciculations. between five months, his lower extremity weakness continues until he was the inability to sit independently.
He also presented with muscular atrophy in the upper limbs, especially in the intrinsic muscles. even though being diagnosed with multiple other diseases, involving chronic inflammatory demyelinated polyneuropathy (CIDP), the patient was diagnosed with ALS & died one year later after symptom onset. In an additional study, Majmudar, Wu, & Paganoni discussed a case involving a 45-year-old women patient who was found with an initial stage of ALS. This patient first began suffering from right lower limb & arm weakness, fatigue & suffered from various falls while playing with her child. Additionally, she described having difficulty with movement including fine motor control, for example cutting food & doing up buttons on clothing.
There is currently no cure for ALS, however, riluzole is a medication that is moderately effective at increasing life for patients with ALS by about two to three months. as well, physical therapy in combination with other forms of healthcare has been displayed to be beneficial for clinical presentation treatment, optimizing functional independence, & enhancing the quality of life in those with ALS. Treatment for ALS must be tailored to the individual to full field their individual needs & aim. Majmudar et al. suggested that exercise, energy conservation techniques, stretching, & range of motion (ROM), as well as the assistive devices for the gait, may be appropriate for early-stage ALS. Nonetheless, the patient must be monitored for signs of overexertion, excessive fatigue, & an enhancement in pain. Tsitkanou et al. explain that both endurance & resistance training has a beneficial effect on the quality of life of the patient; Nonetheless, they do not increase life span.
Epidemiology
- ALS is a very common type of Motor neuron disease in adults The incidence of ALS is approximately 1-2.6 cases per 100 000 persons annually, with a prevalence of approx 6 cases per 100 000.
- In the United Kingdom ALS impact around two in every 100,000 people per year and at any one time, there are about 5,000 people living with the condition.
- For almost half of those with the condition, the average life expectancy from the onset of symptoms to death is 2-4 yrs
- Only 20 percent live above 5yrs
- 5 percent of those diagnosed had it back they were 47 years old
- Incidence high between 55 and 65 years of age
- Clinicians are conveying that they are seeing growing numbers of younger ALS individuals.
- Recently, there is no permanent treatment for motor neuron disease.
Causes of Lou Gehrig’s Disease
The cause of ALS basically indefinite but numerous factors are thought to be involved as well as environmental risk factors, Gene mutations have also been known in some cases of ALS
- Hereditary – this is not true for all cases but a few mutations have been identified in some individuals. In these cases, it is not unusual to have numerous cases in one family.
- Biochemistry – it appears that MND mostly happens through the activation of calcium-dependent enzymatic pathways.
- Premature aging of a few motor cells may direct injury and destruction of these cells. This then puts stress on the remaining cells
- Sporadic MND
- Sporadic ALS (90-95%) constitutes the huge majority of cases
- most common in male
- Incidence is 1-2 per 100,000/ year Familial MND
- Family history of either a motor neuron disease or an associated condition known as front temporal dementia.
- Autosomal dominant
- Ratio 1:1 (male to female)
- Mean age-onset 47 years of age
- Described 5-10% of all ALS occurrences
Pathophysiology
- In the progression of the disease, there is a lack of motor neurons from the anterior horn of the spinal cord, the primary motor cortex, and the hypoglossal nucleus in the lower medulla. adjacent glial cells are also affected. reduction and discoloration of the ventral nerve roots in the spinal cord take place due to axonal degeneration of the neurons and the associated demyelination.
- The pathophysiology behind the disease appears to be multi-factorial with compound interactions between genetics and molecular pathways.
latent cellular & molecular mechanisms that contribute to the neurodegeneration of MND:
- Unusual mitochondria functioning
- Enhanced oxidative strain
- Enhanced free radicals
- Dysfunction axonal transport
- Sodium-potassium pump dysfunction
- Enhanced inflammatory mediators
- Enhanced toxin secretion
- Potential gene mutations that are damaging to neurons and can contribute to the disease:
- TARDBP (transactive response DNA binding protein)
- FUS (Fused In Sarcoma)
Sign and Symptoms of Lou Gehrig’s Disease
- Early Clinical Presentation can be Little and go unobserved. ALS may begin with intermittent muscle twitching, weakness of the muscle, and in a few cases slurred speech. The progression of ALS can also differ from person to person
Initial Symptoms are:
- Weakened of the grip
- Weakness in the shoulder
- Weakness at the hip and ankle
- extensive twitching of the muscles (fasciculations)
- Cramps in the muscle
- Noticeable wasting of the muscles with significant weight lossBulbar-Onset Disease
- gradually more slurred speech (dysarthria)
- Trouble in swallowing (dysphagia)Respiratory-Onset Disease
- Difficulties in breathing
- Dyspnea
- Waking up often during the night for the reason that the brain is momentarily starved of oxygen when lying down
- Advanced Symptoms
- Weakness of the muscle
- Muscle Atrophy
- Movement difficulty
- Spasticity
- Excess saliva from reduced swallowing
- Thicker saliva may from time to time be hard to clear from the chest or throat because of the weakening of muscles
- Excess yawning
Emotionality
- Difficulties with attention, planning, and use of language
- Frontotemporal dementia – this affects their ability to problem solve and counter to new situations
- Difficulties in breathing, for example, shortness of breath
Last-Stage Symptoms
- Increasing chances of body paralysis
- Significant shortness of breath
Secondary Symptoms
These are not directly reasoned by the disease but are associated with the stress of living with it.
- Depression
- Insomnia
- Anxiety
Diagnosis
- There is not only a test that diagnoses a person with ALS nevertheless but various characteristics of the disease can also be identified and as a result, used to point practitioners in the right direction.
- El Escorial Criteria explain the exact characteristics and features that require to be displayed in a person for an accurate ALS diagnosis; even though they are not exclusive. It classifies diagnosis into four distinct categories depending on the severity of upper (UMN) as well as lower motor neuron (LMN) degeneration (which must not be explained by the existence of her neurological disorder).
- Physicians use a combination of some methods for instance electromyography and neuroimaging to identify UMN and LMN degeneration which is the most important feature in neurodegenerative disorders.
- Furthermore, the present research is looking into whole-brain magnetic resonance spectroscopic imaging (MRSI) as a source of determining disability levels in ALS in the future.
- With the exception of one genetic test, no definitive diagnostic test or biological marker is present for ALS – yet, not all persons with the disease present with this gene
- El Escorial Criteria diagnosis for the ALS
- The diagnosis of Amyotrophic Lateral Sclerosis (ALS) needed:
- Indication of lower motor neuron (LMN) degeneration by the clinical, electrophysiological, or neuropathologic examination,
- Indication of upper motor neuron (UMN) degeneration by clinical examination, and Progressive increase of symptoms or signs surrounded by a region or to other regions, as determined by history or examination.
- The lack of Electrophysiological and a pathological indication of other disease processes that might explain the signs of LMN and/or UMN degeneration, and Neuroimaging facts of other disease processes that may explain the observed clinical presentation and electrophysiological sign
Treatment of Lou Gehrig’s Disease
- There is an indication that ALS should be regarded as a multisystem health condition instead only a motor disease. There is no cure or permanent treatment for ALS so the center is on helpful treatments that aim to keep the patient’s quality of life.
- Treatment should take a holistic approach as the disease may be very distressing for the patient and their family & it is necessary not only to focus on the physical aspect of the disease but the emotional and psychosocial components also.
- Physiotherapy, respiratory and occupational therapy, and social care are vital in those with ALS. Dietitians can aid ensure that those with ALS consume a balanced healthy diet and take enough proper nutrition to help them to maintain weight and keep up their strength as individuals may frequently lose weight as their ability to swallow is impaired.
- Dietitians can also advise patients on specific foods, for example, dairy products can contribute to the production of thicker secretions.
- As the disease continues breathing becomes progressively difficult and the need for non-invasive ventilation can significantly improve the quality of life and can also enhance the patient’s life span by around 7 months.
Physiotherapy treatment
- Physical therapy as a practice aid individual better their mobility and function by preferring what restrictions are required to be managed and how best to address them,” says Renée Hetzler, PT, DPT, a physical therapist at the University of Rochester Medical Center’s multidisciplinary ALS. “Physical therapists are the movement experts.
- We guide patients forward to achieve their goals of being able to do any activity that is necessary by the use of exercise prescriptions, education, and equipment recommendations.
- While physical therapy can not halt the inevitable lack of muscle strength for patients living with ALS, the practice can aid them in maintaining as much as independent function patients are capable of at distinct points throughout the disease progression.
- Therapists frequently prescribe equipment for example braces or walking devices initial in the disease that aid patients maintain the ability to walk for longer periods.
- “We examine any home modifications that may be essential as the disease progresses, always keeping in mind that it is best to plan ahead with a fastly progressing disease.” When patients lose the ability to walk, they also aid them to get into modified costume wheelchairs according to the patient’s requirement that will help keep them comfortable while allowing them to continue to transfer on their own.
- Dr. Hetzler says they also prescribe exercises for example moderate strengthening to maintain function and stretching to help decreased joint stiffness and pain.
- Due to the various sign & symptoms of individuals with ALS [PALS], the great variability in prognosis, & the classically rapid, progressive, & deteriorating nature of ALS, we as physical therapists are continuously challenged when developing the most appropriate intervention plan for PALS.
- The physical therapist required an understanding of the nature & course of the disease & required to consider future problems in addition to recent status.
- In order to make appropriate & effective decisions, the nature & significance of the activity limitations, & participation restrictions need to be determined.
- Decision-making includes determining which dysfunctions, activity limitations, & participation restrictions can be restored.
- Require compensatory plan or interventions
- Need a referral to a distinct health care professional(s) &
- Can not be affected by physical therapy interventions at all.
- Most of the clinical presentation of ALS can be addressed by appropriate physical therapy interventions
- energy conservation techniques for fatigue
- stretching exercises for muscle stiffness and Muscle cramps
- Pain (intervention dependent upon the cause of the pain)
- Exercises must focus on improving the posture of the individual, avoiding joint immobility, & declined progressive muscle weakening & atrophy. Stretching & strengthening exercises can help to reduce spasticity, improve range of motion & improve blood circulation.
- Physical therapy can increase an individual’s independence throughout the course of the disease. gentle and light, low-impact aerobic workouts, for example, walking, swimming, & stationary bicycling can strengthen uninvolved muscles, enhance cardiovascular health, & heal people’s fight against fatigue & depression, and contractures of muscles.
- Team members of the ALS multidisciplinary care, physical therapists perform vital roles in an individual living with ALS. As the disease progresses, many individuals slowly lose their ability to use their arms and legs as a result of muscle weakness.
- Physical therapists help patients maintain as much independent function and functionality as they are capable of at distinct points throughout the disease to improve their daily routine.
FAQ
ALS frequently starts with muscle twitching and weakness in extremities or slurred speech. Eventually, ALS affects the control of the muscles required to move, speak, eat, and breathe. There is no permanent cure for this deadly disease.
There is no official list of foods to prevent ALS patients. some research suggests that milk, pork, and luncheon meats can harmfully affect ALS function. Additionally, since patients can be taking drugs, alcohol consumption is not recommended.
Many people who have ALS are between the ages of 40 and 70, with a mean age of 55 at the time of diagnosis. yet, cases of the disease do happen in people in their twenties and thirties. ALS is 20% more usually in males than females.
The cause of amyotrophic lateral sclerosis (ALS) is still widely not characterized. This study reports peak odds of receiving an ALS diagnosis for individuals who reported head trauma, suffering extreme electrical burns, hobbies including lead, and employment in mechanics, painting, or construction.
As ALS patients get sicker, their motor neurons deteriorate, causing muscles throughout the body to atrophy. Despite decades of research, it’s still unclear what damage the neurons. Researchers have long suspected a virus, perhaps one associated to poliovirus or HIV, but the evidence was circumstantial.



One Comment