Lumbar radiculopathy
Table of Contents
What is Lumbar Radiculopathy?
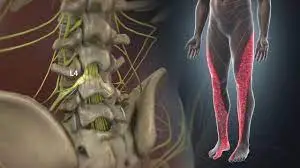
When radiating pain and/or tingling numbness(radiculopathy) occurs in the lower extremity due to nerve roots compression at the lower back at the lumbar spine level, it is called lumbar radiculopathy, also known as sciatica because nerve roots that originate from lumbar spine make the sciatic nerve. The lower back is the area most affected by radiculopathy.
Your spine is made of many bones called vertebrae, and your spinal cord runs through a canal in the center of these bones. Nerve roots split from the cord and travel through the vertebrae into many areas of your body. When these nerve roots become pinched or damaged, the resulting symptoms are called lumbar radiculopathy.
Types of Radiculopathy
Radiculopathy could have many symptoms and many names depending on where in the spine it worsens.
Lumbar Radiculopathy
When radiculopathy worsens in the lower back area, it is known as lumbar radiculopathy, also referred to as sciatica because nerve roots that make up the sciatica nerve are often involved. The lower back area is most frequently affected by radiculopathy.
Cervical radiculopathy
describes a compressed nerve root in the neck area cervical spine. Because the nerve roots in this area of the spine primarily control sensations in patients’ arms and hands, this is where the symptoms are most likely to worsen.
Thoracic radiculopathy
refers to a compressed nerve root in the thoracic area of the spine, which is the patient’s upper back part. This is the least common region for radiculopathy in the thorax. The symptoms often follow a dermatomal distribution and could cause pain and numbness that wraps around the front of your body.
Symptoms of lumbar Radiculopathy
- When a nerve root is compressed at the lumbar spine, it becomes inflamed. This results in several unpleasant symptoms that might include: Sharp pain in the back, arms, legs, or shoulders that might worsen with certain activities.
- something as simple as coughing or sneezing.
- Weakness and lack of reflex in arms and lower limb part.
- Numbness of the skin, “pins and needles,” and another abnormal sensation (paresthesia) in the arms and lower limbs.
- Patients’ main symptoms would depend on where the nerve root is pinched in the spine. However, it’s also possible that you do not experience any symptoms or you go through periodic flare-ups of symptoms.
- pain around the lower back area.
- tingling numbness, pain, and weakness run in the buttocks, hip groin, and leg region.
- muscles spasm
Causes of Radiculopathy
- Lumbar Radiculopathy is typically caused by many changes in the tissues around the nerve roots. These tissues involve bones of the spinal vertebrae, intervertebral disc, and tendons.
- When these tissues shift or change in size, they might narrow the spaces where the nerve roots travel inside the spine or exit the spine; these openings are called foramina. The narrowing of foramina is known as foraminal stenosis, which is really familiar to spinal stenosis that affects the spinal cord.
- Aging, injury, poor posture, extra body weight, and other issues could lead to problems in the low back. These problems might then irritate nerve roots.
- Damage to a disk in the lumbar spine. The damaged disk might then press on nearby nerve roots.
- Degeneration from wear and tear, and aging. This could lead to stenosis (narrowing) of the openings between the vertebrae. The stenosis openings press on nerve roots as they leave the spinal canal.
- Unstable spine. This is when a vertebra slips forward. It could then press on a nerve root.
- Other, less common things could put pressure on nerves in the low back. These involve diabetes, infection, or a tumor.
- In many cases, foraminal stenosis is caused by the gradual degeneration of the spine that happens as you age. But it could also be a result of a spinal injury
- Lumbar radiculopathy is caused by compression, inflammation, and injury to a spinal nerve root in the lower back area. because of this type of pain, in the order of prevalence, include:
- Herniated disc with nerve compression in the lumbar – by far the most common cause of radiculopathy
- Foraminal stenosis (narrowing of the hole through which the spinal nerve exits due to bone spurs or arthritis) – more commonly seen in elderly adults
- Diabetes
- Nerve root injuries
- Scar tissue from early spinal surgery that is affecting the nerve root
Diagnosis of Radiculopathy
Your doctor might take several steps to diagnose radiculopathy:
A physical exam and physical tests might be used to check the patient’s muscle strength and reflexes. If the patient has pain with certain movements, this might asses the doctor to identify the affected nerve root. Imaging tests, such as an X-ray, CT scan, or MRI scan, are used to better see the condition and the area of the problem. Nerve conduction studies, along with electromyography, could also be used to assess and pinpoint whether the problem is neurological or muscular.
Sciatica, the term commonly used to describe radicular pain along the sciatica nerve, describes where the pain is felt but is not an actual diagnosis. The clinical diagnosis is usually arrived at through a combination of the patient’s history (including a description of the pain) and a physical examination. Imaging studies (MRI, CT-myelogram) are used to confirm the diagnosis and would typically show the impingement on the nerve root.
Differential Diagnosis
Radicular syndrome/ Sciatica: a disorder with radiating pain in one or more lumbar or sacral dermatomes, and could be accompanied by phenomena associated with nerve root tension or neurological deficits.
- Pseudoradicular syndrome
- Thoracic disc injuries
- Low back pain
- Cauda equina syndrome
- Inflammatory/metabolic such as Diabetes, Ankylosing spondylitis, Paget’s disease, Arachnoiditis, Sarcoidosis
- trochanteric bursitis
- Intraspinal synovial cysts
Possible complications
Over time, irritated and inflamed nerves might become damaged. This might lead to permanent (long-lasting) numbness or weakness in patients’ legs and feet. If symptoms change suddenly or get worsen, be sure to let your doctor know.
Safety Considerations
To prevent further injury from a patient’s lumbar radiculopathy, your doctor might refer you to a physiotherapist to ensure you have positioned your body correctly.
When a patient dealing with radiculopathy (compressed nerve in the spine), it’s important to reduce or change any activities that make your pain worse. Use ice and heat to assess and reduce pain when needed.
Precautions With Lumbar Radiculopathy
Lumbar radiculopathy symptoms caused by disk herniation are typically worse with sitting or bending forward. Therefore, exercises that include these positions shall be performed with caution. The opposite is true for lumbar radiculopathy caused by stenosis or arthritis. Forward bending typically decreases pain for these individuals.
Treatment For Lumbar Radiculopathy
First aid–
In the Lumbar radiculopathy, gently make her way to the nearest comfortable chair or sofa. Here, you could try the following techniques to overcome the pain:
Gently massage the lumbar area with the hand or using the massage gun. This might give temporary relief to spasms.
As patients massage, they part, make sure that they should be mindful of their breathing. Take slow breathing to overcome stress-increase pain.
Diaphragmatic breathing could help the patient to become calm down.
Apply at once heat and ice in 15–20 after the break.
If possible, try to look out for a comfortable lumbar stretch, like Child’s Pose or a seated spinal twist. This requires the patient to stand up from the couch and get to the base, so only proceed if the patient feels comfortable with these movements.
Wrap ice packs in a towel to ensure ice burns, and give patients’ skin a break after icing.
Regular stretching helps an individual with chronic lumbar radiculopathy, but for acute lumbar radiculopathy, this might cause Trusted Source additional swelling to the affected area.
The best treatment for acute lumbar radiculopathy is to take some rest, take it easy, and call the doctor if the pain gets worse.
Medical Intervention-
Non-steroidal anti-inflammatory drugs (NSAIDs)–
such as Ibuprofen, would not give immediate relief, but it might help slow down within 30–60 minutes.
Muscle relaxants-
A doctor might determine muscle relaxants when a patient has severe radiculopathy that is visible and prominent.
People shall only take muscle relaxants for up to 72 hours.
Water and electrolytes-
Dehydration might cause lumbar radiculopathy, or make existing radiculopathy severe.
Carry with drinking water, or review switching to an electrolyte drink.
Physical therapy treatment-
It includes electrotherapy and exercise therapy techniques.
Electrotherapy-
TENS and ultrasound are most commonly used to control pain and decrease lumbar radiculopathy.
Exercise therapy –
Acute radiculopathy includes-Heat or ice application and massage techniques and stretching of specific muscles area and strengthening in the progression period.
Chronic lumbar radiculopathy includes-Spinal manipulation techniques
Heat or ice-
Both heat and ice might decrease the radiculopathy in the lumbar.
Both treatments could decrease inflammation and ease muscle tension.
Simultaneous hot and cold packs might be particularly helpful.
first of all, try to apply hot and then cold packs for 20 minutes at one time, with a 20-minute break in between this.
Do not apply too hot or cold packs directly to the skin. Instead, damp them in a towel or cloth before placing them against the lumbar area.
Massage-There are five different massage techniques to relieve lumbar radiculopathy-
1. Effleurage–
Describe by long, sweeping strokes from the top.
2. Petrissage
petrissage massage encompasses rolling and kneading.
Pressure commonly depends on the sensitivity of the patient.
This technique mainly focuses on the tense part of the back area.
The massage therapist starts the Swedish massage with a light petrissage and slowly induced the pressure to release tension.
3. Tapotement –
These manners include light and rhythmic tapping or drumming.
The pressure and speed are either relaxing or energizing.
4. Friction –
The massage therapist might put deep pressure on the affected muscle to release tension.
Firm pressure on the affected muscle may help decrease the tension.
Stretching-
Here, a few stretches are recommended for lumbar radiculopathy;
Ergonomic advise-
There are some tips that could help a person to relax their lumbar radiculopathy when it happens.
They could also help you prevent lumbar radiculopathy in the first place.
Exercise for Lumbar radiculopathy
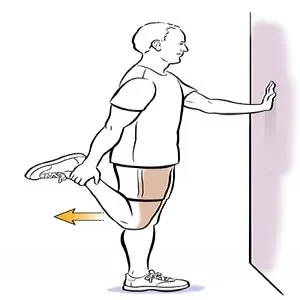
Hip Flexor stretch:
Hip Flexor Stretch exercise Exercises for lumbar radiculopathy often begin with the reverse. Use a hip flexor stretch to improve rotation and mobility. This exercise assesses cases of hips rotating more effectively, adding inflexibility and making it easier to move.
Step 1 Kneel with one knee on the patient’s mat.
Step 2 Lift the arm on the same side as the knee that’s down on the ground( back knee).
Step 3 Move your raised arm back. That should make the patient’s hips move forward and your reverse stretch.
Step 4 Hold that position for 15 to 20 seconds.
You should repeat this exercise three times.

Quadriceps Stretch:
This stretch is aimed at improving lumbar elasticity.
Step 1 Lie down, face down.
Step 2 On the side most affected by Lumbar Radiculopathy, attach a towel or therapeutic band to the bottom. Use the towel/ band to pull the patient’s heel to your buttock.
Step 3 Hold it for 1 minute.
You can repeat this stretch three times.
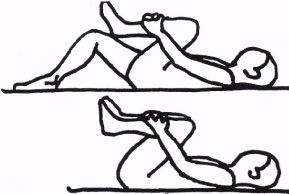
Bring Your Knees to Your Chest:
This is a simple move that stretches out the lower of your back and can help with a spondylolisthesis(a condition affecting the lower vertebrae of your spinal column).
Step 1 Lie down, knees bent.
Step 2 Bring the patient’s knees( both of them) into the patient’s chest.
Step 3 Keep them there for roughly 5- 10 seconds.
Step 4 Take a break.
Repeat this exercise 5 to 10 times a day.
Upward dog:
A common yoga pose, an overhead-facing dog offers a deep chest stretch and helps make your core muscles.
Step 1 patient’s Position is flat on the mat, face down.
Step 2 Lift your head a bit. Put the patient’s hands beneath your shoulders with the patient’s palms down.
Step 3 Point your toes.
Step 4 Breathe out.
Step 5 Told to Raise your body and legs off the ground by pushing through the patient’s hands and through the tops of the patient’s feet.
Step 6 Make sure your neck is long and relaxed, and engage your hams so they’re tight while you hold the upward dog and continue breathing.
Step 7 When you hold this plank exercise, start with a 10-15-second break and slowly increase, as your core strengthens, up to 30 seconds.
Perform the upward dog pose once a day. It’s common to begin your day with this popular yoga position to assess you and warm up your back muscles.

Crunches( Curl- ups):
Crunches isolate the muscles in your abdomen. Strengthening the patient’s abdominal muscles can help reduce sciatica pain.
Step 1 taradiddle on your back.
Step 2 Bend your knees, deposited at a 90-degree angle.
Step 3 Check that your feet are about a base away from your body and are flat on the bottom.
Step 4 Told patients to place their hands on their shoulders, and crossed over each other.
Step 5 Bring your stomach muscles in, stretching them.
Step 6 Lift your shoulder blades upward and down from the bottom.
Step 7 Keep your heads and shoulders aligned. Don’t put your head down toward your chest.
Step 8 Stay for 1- 2 seconds.
Step 9 Gently lower yourself back to the bottom.
Complete 8- 12 crunches per day to help make up muscles.

Pelvic tilt:
The pelvic tilt exercise is done by lying on your back with your knees bent and bottoms flat on the floor. You’ll also contract your stomach muscles and tilt your pelvis up so that you feel a gentle lift in your belly. This movement could assess strengthening the abdominal muscles and also assess loosening the lower back muscles.

FAQ
It depends on what caused the patient’s radiculopathy, and which type you are experiencing. In general, some people feel better sooner (in a few weeks). It may be longer if the patient has severe symptoms or other conditions that affect the patient’s spine.
Other risk factors involve driving occupations, frequent lifting, especially with a twisting movement, heavy industry work, back trauma, taller height, smoking, being overweight, sedentary lifestyle, multiple pregnancies, history of back pain, and chronic cough.
Numbness and tingling could interfere with your ability to write, type, use the telephone, or carry and move objects. While patient cervical radiculopathy might only affect one arm or hand, it could prevent you from using your both arms or hands in unison.
After a long period of time, an irritated and inflamed nerve might become damaged. This might lead to permanent(long-lasting) numbness or weakness in patients’ legs and feet.
Lumbar radiculopathy could be diagnosed with a thorough history and physical examination in some cases, but MRI shall be used to confirm the diagnosis. The affected dermatomes could both overlap and vary for a certain nerve root in lumbar radiculopathy.






5 Comments