Coma
Table of Contents
What is Coma?
- Coma is an abnormal state in which a person is not alert and not completely responsive to their surroundings.
- situations of coma range from drowsiness to collapse and may range in severity from fainting to coma.
- Unlike when a person is asleep, someone who is coma can’t cough, clear their throat, or turn their head if in distress.
- When coma, a person is in danger of choking, making it most important to keep the airway clear while awaiting medical care.
- Coma is a state in which a patient is fully unaware of both self and external surroundings, and unable to respond meaningfully to external stimuli.
- Coma results from gross impairment of both cerebral hemispheres and the ascending reticular activating system.
- A coma is a deep state of unconsciousness. Few patients following moderate to severe traumatic brain injury will present with profound and prolonged consciousness impairment.
- Coma may occur as an anticipated progression or complication of an underlying illness, or as a result of an event similar to head trauma.
- This occasionally follows a coma, which refers to a condition in which individuals have lost cognitive neurological function and awareness of the environment but retain noncognitive function and a preserved sleep-wake cycle.
- It’s occasionally described as when a person is technically alive, but their brain is dead.
- Still, that description is not completely accurate. In the persistent vegetative state the individual loses the higher cerebral powers of the brain, but the functions of the brainstem, similar to breathing and circulation, remain relatively intact.
- Spontaneous movements may do and the eyes may open in response to external stimuli, yet the patient does not speak or obey commands.
- Patients in a vegetative state may appear kindly normal.
- They may occasionally cry, grimace, or laugh.
Causes of Coma
Many types of problems can cause a coma. Some examples are:
- Traumatic brain injuries
- Stroke
- Tumors and Bleeding
- Diabetes
- Swelling
- Blood sugar
- Lack of oxygen
- Infections
- Seizures
- Toxins
- Drugs and alcohol
- Traumatic brain injuries: These are oft caused by traffic collisions or acts of violence.
- Stroke: Stopped or Reduced blood supply to the brain, known as a stroke, can result from blocked arteries or a burst blood vessel.
- Tumors and Bleeding: Tumors in the brain or brainstem can cause a coma. Bleeding in the layers of the brain may cause coma due to compression and swelling on the injured side of the brain. This compression causes the brainstem to shift, causing damage to the brain. Ruptured cerebral aneurysms, High blood pressure, and tumors are non-traumatic causes of bleeding in the brain.
- Diabetes: Blood sugar levels that become too low or too high can cause a coma.
- Swelling: Swelling of brain tissue can do even without distress. Sometimes Oxygen deprivation, electrolyte imbalance, or hormones can cause swelling.
- Blood sugar: In people with diabetes, a coma can do when blood sugar levels stay very high. That’s a condition known as hyperglycemia. Blood sugar, or Hypoglycemia that’s too low, can also lead to a coma. This type of coma is commonly reversible once the blood sugar is corrected. Still, prolonged hypoglycemia can lead to permanent brain damage and persistent coma.
- Lack of oxygen: Lack of oxygen for a few minutes causes cell death in brain tissues. People who have been rescued from drowning or revived after a heart attack might not awaken due to a lack of oxygen to the brain. Oxygen is essential for brain function. Cardiac arrest causes a sudden cutoff of blood flow and oxygen to the brain, called anoxia or hypoxia. After cardiopulmonary resuscitation, survivors of cardiac arrest are oft in comas.
- Infections: Infections such as meningitis and encephalitis cause swelling of the brain, spinal cord, or the tissues that surround the brain. Tough cases of these infections can result in brain damage or a coma.
- Seizures: Ongoing seizures can lead to a coma. A single seizure rarely produces a coma. Repeated seizures can help the brain from recovering in between seizures. This will cause prolonged unconsciousness or coma.
- Toxins: Exposure to toxins, such as carbon monoxide or lead, can create brain damage and a coma. Substances that are commonly found in the body can accumulate to toxic levels if the body fails to dispose of them correctly. As an example, ammonia due to liver disease, carbon dioxide from a severe asthma attack, or urea from kidney failure can accumulate toxic levels in the body.
- Drugs and alcohol: Overdosing on drugs or alcohol can affect a coma.
Types of Coma
Types of coma can include:
- Brain death
- Toxic-metabolic encephalopathy
- Anoxic brain injury
- Locked-in syndrome
- Persistent vegetative state
- Medically induced
Complications of Coma
- Although many people gradationally recover from a coma, others enter a persistent vegetative state or die. Some people who recover from a coma end up with minor or major disabilities.
- During a coma, urinary tract infections, bedsores, blood clots in the legs, and other problems may develop.
Signs & Symptoms of Coma
The signs and symptoms of a coma generally include:
- Closed eyes
- Irregular breathing
- Depressed brainstem reflexes, like as pupils not responding to light
- No responses from both limbs, except for reflex movements
- No response to painful stimulants, except for reflex movements
- pupils not responding to light
Diagnosis
- If available, the history from relatives or ambulance staff will oft give all the necessary clues needed to make a provisional diagnosis of the cause of unconsciousness.
- Still, if they are a pyrexial, depressed epileptic diabetic that has been unwell recently and then fallen down stairs.
- Making a diagnosis is important for it will direct appropriate therapy.
- Still, it does not reduce the need for generic supportive care, such as that offered in intensive care.
- Sometimes, the diagnosis allows the withdrawal of care, if the cause of the coma is untreatable and the brain damage irreversible.
Evaluation
- The comatose case should be physically examined for any useful signs, such as lumps on the head and non-blanching rashes.
- The system which will be examined most intently ( and often providing the least information) is the nervous system.
- There are certain zones of the central nervous system that are easy to examine, including the eyes and reflexes, yet other information is provided by the posture and muscle tone, and respiratory pattern.
- The eyes do give useful information – pupil size and equality, and direction of aspect.
- A truly comatose case is deeply unconscious, with no response to pain.
- Still, it is often found that patients are not completely unconscious, and so can be categorized onto a point on a “coma scale”.
Then’s an example of a simple 5-point scale:
1 = Fully awake
2 = Conscious but drowsy
3 = Unconscious though responsive to pain with purposeful movement e.g. flexion/extension
4 = Unconscious though responding to pain by extension
5 = Unconscious and unresponsive to pain
- This scale gives a simple measure of the degree of unconsciousness, yet disregards other information that may be available.
- The most commonly used complex scale, using three groups of conformances, is the Glasgow Coma Score, which was initially suggested for the assessment of head injury cases.
GCS SCALE POINTS
This looks at eye exercise, and verbal and motor responses, and assigns points for each to give a compound score, 3 being deeply unconscious and 15 being totally conscious:
Best eye response
Eyes open spontaneously = 4
Eyes open to command = 3
Eyes open to response to pain = 2
Eyes remain closed = 1
Best verbal response
Fully orientated = 5
Confused = 4
Inappropriate words = 3
Incomprehensible sounds = 2
No response = 1
Best motor response
Movement in response to command = 6
Localizes pain = 5
Withdraws from pain = 4
Flexes in response to pain = 3
Extends in response to pain = 2
No response = 1
- These scales and scores are most useful in allowing the assessment of changing positions of consciousness, either improvement or deterioration. A worsening of the GCS in a head-injured case indicates the need for instant neurosurgical intervention.
There are different coma scales, which apply to definitive types of coma, such as that found in hepatic failure:
Stage 1: impaired personality or thinking. EEG usually normal
Stage 2: confusion, abnormal sleep, and drowsiness. & Increased reflexes, with plantar responses up or down. EEG abnormal.
Stage 3: marked confusion, with the inability to perform the fine movement. Responds to painful stimuli
Stage 4: comatose with depressed reflexes
- These problems in hepatic failure are caused by cerebral edema, due to problems such as hypoglycemia, hypokalemia, hyponatremia, hypothermia, and respiratory and renal default.
- The Rancho Los Amigos Scale: It is most practical during the first weeks or months after the injury. Based on the results of these two scales, doctors put cases in one of four awareness states:
Comatose and unresponsive – The patient cannot move or respond to stimulants.
Comatose and responsive – The patient does respond to stimulants, with responses such as movement or increased heart rate.
Conscious and unresponsive – The patient can see, touch, hear, and taste, but can’t respond.
Conscious and responsive – The patient is out of a coma and can respond to commands.
Examinations
- A full blood count, and easy biochemistry, give lots of useful information which may make the diagnosis.
- Other simple tests oft useful in the diagnosis of unexplained coma include blood sugar, paracetamol, and aspirin category.
- An investigation that is used increasingly, and often without a proper physical examination of the case, is the computerized tomogram of the head, the CT scan.
- The process puts the case at some risk while in the scanner, but it does give quite a lot of information about what is going on inside the head.
- It will view space-occupying lesions, bleeds, and swelling of the brain.
- There is a more sophisticated scan available, the MRI, which shows like things but in better detail.
- They take longer and are less readily available, and are so not utilized in the acute stages of management very oft.
- Lumbar puncture is oft undertaken and will give information about infection or bleeding. The EEG may issue useful information, especially if epilepsy is suspected.
Prognosis of Coma
- The result of coma and vegetative state depends on the cause and on the position, severity, and extent of neurological damage outcomes range from recovery to death.
- People may emerge from a coma with a combination of physical, intellectual, and cerebral difficulties that need special attention.
- The chances of a person’s recovery depend on the cause of the coma, whether the problem can be corrected, and the life of the coma.
- Still, The person can oft return to his or her original level of functioning, If The problem can be resolved,
- occasionally, however, if the brain damage is severe, a person may be permanently disabled or noway regain consciousness.
- Recovery commonly occurs gradually, with patients acquiring more and more ability to respond.
- Some cases noway progress beyond very basic responses, but many recover full awareness.
- Cases recovering from comas require close medical supervision.
- A coma rarely lasts further than 2 to 4 weeks.
- In some cases may regain a degree of awareness after a vegetative state.
- Others may remain in a vegetative state for years or indeed decades.
- The very common cause of death for a person in a vegetative state is infection such as pneumonia.
Treatment
- Treatment depends on the cause of the coma. A coma is a medical emergency. coma patients will normally be placed in an Intensive Care Unit (ICU) immediately, then the maintenance of the patient’s respiration and circulation becomes a first priority.
- A drug or procedure to relieve pressure on the brain due to brain swelling might be needed.
- Emergency responders might be given antibiotics or glucose through a vein in the arm.
- These may be given indeed before blood test results return in cases of very low blood sugar or an infection affecting the brain.
- Healthcare providers normally first check the affected person’s airway and help maintain breathing and rotation.
- Providers might give breathing assistance, ventilation, administration of intravenous fluids or blood, and other supportive care.
- The coma is the result of a drug overdose, and healthcare providers commonly give medicines to treat the condition.
- The coma is due to seizures, drugs can control seizures. Other treatments might focus on drugs or therapies to address an underlying disease, such as diabetes and liver disease.
- The cause of a coma can be fully reversed, and the affected person regains function.
- A person with severe brain damage might have permanent disabilities or noway regain consciousness.
- Recovery usually does gradually.
Continued care
- Once a patient is stable and no longer in immediate danger, there may be a shift of priority from stabilizing the patient to maintaining the state of their physical well-being.
- Moving patients every 2–4 hours by turning them side to side is crucial to avoiding bed sores as a result of being confined to a bed.
- Moving patients through the use of physical exercise also aids in preventing contractures, and another orthopedic deformities that would interfere with a coma patient’s recovery.
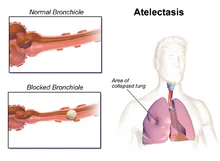
- Pneumonia is common in coma patients due to their inability to swallow which can then lead to aspiration.
- A coma patient’s lack of a gag reflex and use of a feeding tube can result in food, drink, or another solid organic matter being lodged within their lower respiratory tract.
- This trapping of matter in their lower respiratory tract can eventually lead to infection, resulting in aspiration pneumonia.
- Coma patients may also deal with restlessness or seizures. Still, soft cloth restraints may be used to prevent them from pulling on tubes or dressings and side rails on the bed should be kept up to prevent patients from falling.
Caregivers
- Coma has a wide variety of emotional responses from the family members of the affected patients, as well as the primary caregivers taking care of the patients.
- Research has shown that the inflexibility of injury-causing coma was set up to have no significant impact compared to how much time has passed since the injury occurred.
- Common responses, such as desperation, wrathfulness, frustration, and denial are possible.
- The focus of patient care should be on creating an agreeable relationship with the family members or dependents of a comatose patient as well as creating a fellowship with the medical staff.
- Although there is heavy importance on a primary caretaker, secondary caretakers can play a supporting role to temporarily relieve the primary caretaker’s burden of tasks.
Physiotherapy Rehabilitation in ICU
- Physiotherapy is an important intervention that helps and mitigates the adverse effects of prolonged bed rest and mechanical ventilation during critical illness. Rehabilitation delivered by the physiotherapist is tailored to the patient’s requirements and depends on the conscious state, psychological status, and physical strength of the case. It incorporates any passive and active exercise that promotes movement and includes mobilization. Early progressive physiotherapy, with a focus on walking and mobility whilst ventilated, is necessary for minimizing functional decline.
Adverse effects of ICU stay:
- Physical Inactivity leads to muscular atrophy and generalized weakness
- compromised cardiac and respiratory function
- Diaphragmatic weakness due to prolonged mechanical ventilation
- Pressure Ulcers
- deep vein thrombosis
- infections
- The physiotherapist works to maintain and improve respiration and cardiac functions and later on aid in rehabilitation.
Short-term Goals:
- Early activity – Both passive and active to maintain the integrity of the musculoskeletal system
- Positioning patients: To allow gravity to prevent sputum drain from the lungs.
- Manual techniques such as shaking and vibrations: Are applied to the ribs to try to loosen and clear the sputum.
- Suction: By placing a small tube into the lungs to suck out the extra sputum.
- They play a vital role in weaning a case off ventilation.
Long-term Goals:
- Plan an extensive rehabilitation program to unify and re-initiate the patient into society.
- Set goals in the compound with the medical team to rehabilitate the patient.
- Rehabilitation goals are set in communication with the patient, the patient’s family, and the medical team and are divided into short, medium, or long-term and change throughout the patient’s recovery from critical illness. It can be physical as well as psychological but is concerned with the functional needs of the patient. Goals will need to be achievable and grounded on a regular patient assessment of physical and non-physical consequences of the critical illness throughout their recovery and change according to the progress.
Physiotherapy Techniques in ICU
Respiratory Physiotherapy:
- The role of the respiratory physiotherapist is to help in clearing the airways of the patients and maintaining and improving the integrity of the respiratory system.
Treatment interventions include:
- Positioning,
- Education,
- Manual and ventilator hyperinflation,
- Weaning from mechanical ventilation,
- Non-invasive ventilation,
- Chest Physiotherapy treatment – Percussion, vibration, suctioning,
- Respiratory muscle strengthening,
- Breathing exercises and mobilization
Impact of Physiotherapy
- Early intervention by physiotherapists in the ICU prevents:
- Reduce the patient’s stay in the ICU and generally stay in the hospital.
- Prevent ICU-related complications
- To improve quality of life in the short and long term
Recovery
- Few People may emerge from a coma with a combination of intellectual, physical, and psychological difficulties that need special attention. It is common for coma cases to awaken in a profound state of confusion and experience dysarthria, the incapability to articulate any speech. Recovery is usually gradual. In the first days, the patient may only awaken for some minutes, with an increased duration of wakefulness as their recovery progresses, and they may eventually recover full awareness. That said, few patients may ever progress beyond very basic responses.
- There are reports of few people coming out of a coma after long periods of time. After 19 years in a minimally conscious state, spontaneously began speaking and regained awareness of his surroundings.
- A man with brain damage trapped in a coma-like state for six years was brought back to consciousness and planted electrodes deep inside his brain. The method, called deep brain stimulation (DBS), successfully roused communication, complex movement, and eating ability in a 38-year-old American man with a traumatic brain injury. His injuries quit him in a minimally conscious state, a condition akin to a coma but characterized by occasional, but brief, substantiation of environmental and self-awareness that coma patients lack.
FAQ
Someone who is in a coma is unconscious and has minimum brain activity. They’re alive but can’t be woken up and show no signs of attention. The person’s eyes will exist closed and they’ll appear to be unresponsive to their environment.
Generally, coma cases have their eyes closed and cannot see what happens around them. But their ears keep taking sounds from the environment.
Generally, a coma does not last more than some days or a couple of weeks. In some rare cases, a person might stay in a coma for several weeks, months, or indeed years. Depending on what caused the person to go into a coma, some cases are suitable to return to their normal lives after leaving the hospital.
The chances of someone recovering from a coma largely depend on the inflexibility and cause of their brain injury, their age, and how long they’ve been in a coma. It’s impossible to exactly predict whether the person will eventually recover, how long the coma will last, and whether they’ll have any long-term problems.
Lack of oxygen for a few minutes causes cell death in brain tissues. Anoxic brain injury may result from a cardiac arrest (heart attack), head injury or trauma, drowning, drug overdose, or poisoning.
Brain death is not equal to a coma, because someone in a coma is unconscious but still alive. Brain death occurs when a critically ill case dies sometime after being placed on life support.
People in a coma will not age like aware people living life. Muscles weaken & emaciate. The damaged part of the brain might worsen as a result of inflammation in the area.
The brain is still working, still, and the degree of brain activity varies from patient to patient. New tools for mapping brain activity have assisted doctors to illuminate what is happening inside the brain, which informs their treatment and care.
Once out of a coma, which generally lasts for around 1-4 weeks (in severe cases months or indeed years) patients need to act quickly to recover from this devastating experience. Physical therapy is a key way for individuals who have gone through a coma to improve their motor skills and stimulate brain function.




10 Comments