Pronator Teres Syndrome:
Table of Contents
Description Of Pronator Teres Syndrome:
Pronator Teres Syndrome (PTS) is a compression of the median nerve at the elbow. It is not the same as compression at the wrist like Carpal Tunnel Syndrome (CTS). PTS and CTS both are similar, but a special test of CTS is negative in PTS, however, PTS may alter the sensation in the distribution of the palmar cutaneous branch of the median nerve.
It should also be noted that Anterior Interosseous Nerve Syndrome (AIN Syndrome) is another condition that can occur with nerve compression at the elbow, similar to PTS. However, AIN Syndrome mainly affects the motor function of some or all of the muscles innervated by the forearm’s median nerve, including the forearm’s flexor muscles. like, flexor digitorum profundus muscle of the index and middle fingers, flexor pollicis longus muscle, and pronator quadratus muscle.
It is rarely seen in people and the incidence rate is less than 1 per 100,000 annually. It is commonly seen in females compared to males person. Pronator teres syndrome (PTS) was described by Henrik Seyffarth in 1951.
Anatomy of the Median nerve:
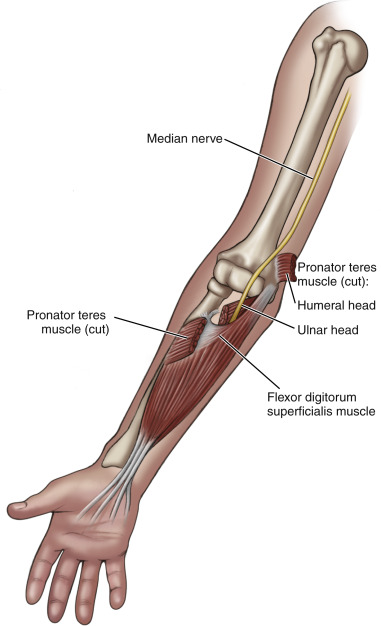
The median nerve arises from the C6, C7, C8, and T1of the spinal cord. It originates from the brachial plexus. Then runs down into the arm from the, then enter into the cubital fossa and passes between the two heads of pronator teres muscle into the forearm. Then it runs between the flexor digitorum superficialis muscle and flexor digitorum profundus muscles and enters the hand by the carpal tunnel.
It supplies most of the flexor muscles in the forearm and hand. It supplies the sensation of the palm, thumb, index, middle finger, and half the ring finger.
In the proximal region of the forearm it gives rise to the anterior interosseous nerve which supplies the flexor of the thumb (FPL), the flexor digitorum profundus muscle of the index finger (FDP IF), the pronator quadratus muscle, and terminates in a sensory branch to the wrist bone. Compression of the median nerve in a proximal part results in weakness of these three muscles and can cause pain in the wrist.
Symptoms of pronator teres syndrome:
Compression of the median nerve at the elbow or proximal part of the forearm can cause pain and numbness in the distribution of the distal median nerve, and weakness of the muscles supplied by the anterior interosseous nerve (the flexor pollicis longus (“FPL”) muscle, the flexor digitorum profundus of the index finger (“FDP IF”), and the pronator quadratus muscle(“PQ”)).
The weakness of the FPL and FDP IF is painless, but causes people to “leave the things” and also have sensation loss. People easily adapt to this weakness without any effort or self-awareness of this condition by using:
1) The next muscles down, which are innervated by another nerve,
2) Use ligaments to give resistance, pinching laterally against the index finger or the side of the end of the thumb.
3) The “tenodesis,” in this case the extension of the wrist joint, which tightens the muscles tendons on the palm side of the hand.
These adaptations on a different moment basis do not cause problems, but for a long time in loose-jointed patients, such as many women and people with collagen disorders like Ehlers Danlos Syndrome, the adaptations can affect the soft tissue that can become painful and particularly at the base of the thumb and in the proximal forearm (example, “Tennis Elbow” occur in a nontennis player).
Paresthesias in the thumb, index, middle finger, and radial half of the ring finger as seen in carpal tunnel syndrome but pronator syndrome paresthesias are made worse with repetitive pronation and supination movement.
This condition has some characteristics which differentiate it from carpal tunnel syndrome,
- Pain on the proximal volar forearm
- The sensation is present over the distribution of the palmar cutaneous branch of the median nerve (palm of hand)
- Symptoms arise 4 to 5 cm proximal to carpal tunnel
- In this condition have no night symptoms.
Both conditions may be occurred by repetitive activity. in PTS patients have tenderness over the pronator teres muscle. Medial elbow tenderness is common. Also, affect the sensation of grip clumsiness or a weak pincher grip.
Causes of Pronator Teres Syndrome:
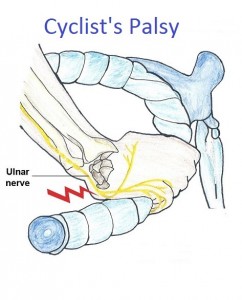
The most common cause is impingement of the median nerve between the two heads of the pronator teres muscle. Other causes are the compression of the nerve from the fibrous arch of the flexor superficialis muscle and the thickening of the bicipital aponeurosis.
Impingement and compression of the median nerve resulting swelling and inflammation of the structures situated around the median nerve as it passes through the elbow region.
Risk factors of Pronator Teres Syndrome:
- Hypothyroidism.
- Diabetes.
- Alcoholism.
- Any type of trauma at the elbow.
How can diagnose the condition?
The commonly patient chief complaint is intermittent pain in the wrist, related to sustained pronation, frequently it conclude the “tendonitis.” This is concluded by the symptoms of “hand weakness,” and “dropping things.”
The first doctor takes a careful history of the patient, by the physical examination that points to the confirmed diagnosis of pronator syndrome.
The physical findings:
- tenderness over the proximal median nerve.
- numbness in the forearm and hand, sometimes it is present at night. Weakness in the flexor pollicis longus muscle and FDP of the index finger, leading to impairment of pinched nerve. In this the involvement of the anterior interosseous nerve.
- The doctor examines symptoms reproduced when the do the elbow flexed to 120 degrees against resistance, this is strongly related to median nerve compression. Similarly, the doctor may compress the median nerve at the elbow by giving pressure on it. If numbness and tingling are reproduced within 30 seconds, that suggests pronator syndrome.
- Sensory changes are present in the first three fingers and the palm.
The clinical and electrophysiological diagnoses of pronator teres syndrome are different from patients with carpal tunnel syndrome or anterior interosseous syndrome.
An Electrodiagnosis test:
- NCV: The Conduction velocity of the median nerve in the proximal forearm may be affected but the distal latency and sensory nerve action potential at the wrist are normal.
- MRI: It shows denervation and atrophy of the affected muscles, by this report the evaluation of pronator teres syndrome is unclear. In the MRI shows the detail of the soft tissue affecting the median nerve.
- X- Ray: An x-ray of the elbow will be taken to confirm any bony abnormality which may be causing symptoms.
If the EMG or the MRI test results are abnormal for the pronator teres muscle and the flexor carpi radialis muscle the problem is at or proximal to the elbow.
Differential diagnosis:
- Anterior interosseous nerve entrapment.
- Carpal tunnel syndrome.
- Pronator teres strain.
- Cervical Radiculopathy.
- Thoracic Outlet Syndrome.
- Brachial Plexus Neuritis.
Treatment of Pronator Teres Syndrome:
Nonsurgical treatment:
- Injection of corticosteroids into the pronator teres muscle to relieve the symptoms.
- Massage therapy can also give relief to individuals experiencing this condition.
- Rest and ice are massages applied on the pronator muscle for early healing.
- Wearing a splint to avoid forearm rotation:
- Surgical decompression can given beneficial in selected cases.
One study reported that 50% of pronator syndrome patients recover within four months of initiating care. Surgical decompression technique of the median nerve is done when non-operative management fails.
Surgical Treatment:
If motor deficits such as weakness or paralysis are noted during the physical examination, or if the patient does not respond to conservative methods, surgery may be required to treat pronator syndrome.
- This surgery aims to decompress the nerve at the exact area of nerve entrapment.
- Postoperatively, the patient wears a long arm splint for Eight to ten days, after the splint is removed and sutures are also removed, the patient wears to a removable splint.
- The splint is worn at night and during the day for a minimum of two weeks. Then Physical therapy is taken to improve the strength and the back to normal active movement of the forearm and hand.
Physiotherapy treatment for pronator teres syndrome:
- Take a rest in between the activity.
- Apply Ice massage over the pain area.
- Stretching of the pronator teres muscle.
- Stretching of flexor muscles of the wrist.
- Nerve flossing exercise for the median nerve.
- Strengthening exercise of the supination muscles.
- Massage technique.
- Kinesio taping technique.
- Dry needling technique.
- Myofascial release of pronator teres.
- Electrical modalities like TENS, and the US, decrease the pain and spasm, and tingling sensation.
- Wearing splint.
- Patient education and advice on Modified activity/sport.
Resting:
It is essential to stop overusing the affected arm for the repetitive activity of grasping and forearm rotation movement. Therefore, an elbow orthosis is helpful to rest the elbow in a bending position, and the forearm in a neutral position. patient wear it the whole day for at least 2 to 4 weeks.
For heavy computer users, therapists should advise using an ergonomic split keyboard and vertical mouse, which help to reduce full pronation of the forearm when typing and mousing.
Therapeutic exercises:
1. Median Nerve flossing Exercise:
- Sit on the table and reach the affected arm out to the side, and bring with your shoulder, the hand facing the floor.
- Flex the hand and pull the fingers up toward the ceiling.
- Bend the arm and bring the hand toward the shoulders.
- Repeat it 5 times
2. Pronators Stretching:
- Standing with the back facing the door.
- Raise your to arm backward (shoulder extension) as much as possible, and keep the elbow straight.
- Grasping the doorframe with your thumb pointing down.
- Rotate the arm externally.
3. Myofascial Release:
- First Keep the elbow bend, palm facing up. Put the thumb over the affected forearm, near the elbow
- Rotate the palm facing down, so that palpate the pronator teres muscle be
- After the palpation of the tender point, press for 5 seconds without triggering any symptoms like tingling or numbness sensation.
- Rotate your forearm repeatedly. (turning your palm up and down) this movement repeats 10 times while the thumb is still on the belly point.
4. Standing palm press (Flexor and Extensors muscles stretching):
- The forearm muscles and hand muscles will be stretched along with the nerves in the arm.
- Stand affected side of the body facing the wall side. the feet should be slightly apart.
- Press that hand into the wall, while keeping the torso upright position and the arm should be straight.
- Fingers should be pointed up.
- Pull shoulder or body back and hold the stretch for five deep breaths.
- Change finger’s position is pointed downward without hunching the shoulder and another position will be the same.
- Hold the stretch for five deep breaths.
6. Standing curl Exercise:
- First, stabilize the pelvis and torso and it helps to work all the muscles in the shoulders and arms.
- Rotating movements of the arms improve muscle strength and movement in the forearm.
- Stand with legs and shoulder-width apart, hold the dumbbell in one hand which hands facing toward the legs.
- Curl or flex the arms to the shoulders and rotate the hands that face the shoulders.
- Rotate the arms and hands so that the knuckles are facing toward the body. then back to starting position.
- Repeat this movement 10 times.
7. Massage Techniques:
- Massage techniques can help to decrease tension in the pronator teres muscle so that decreases compression on the median nerve. Called “releasing” the pronator teres.
- These techniques performed by a trained professional can lengthen the muscle.
- The practitioner performs contact inhibition and drained the tension which areas are tight.
- This technique helps to work stubborn tension out of the muscle and relieves compression of the underlying nerve.
8. Kinesio Taping:
- Attach the tape over the outside of the mid forearm, then stretch it diagonally to the inside of the forearm.
- Apply the Kinesio tape over the pinky side of the wrist and stretch it towards the inside of the elbow.
- This tape is applied for 2 or 3 days and then it removes.
9. Dry needling:
- The dry needling technique is used to reduce pain, reduce activation of resting muscle and reduce muscular tension.
- In this technique used different size needles and apply them to the pain area.
10. Patient Education:
During conservative treatment, patients should be advised to minimize their related activities that involve frequently forearm pronation movement.
These activities include:
- Hammering.
- Ladling food.
- washing dishes.
- Playing table-tennis.
- Pouring drinks, activity performed by waitresses.
- Carry the books frequently performed by librarians.
- Twisting the clothes.
What is the Prognosis of Pronator Teres Syndrome?
Pronator teres syndrome needed PT muscle release has a good recovery in most cases, and patients return to light duty in around 3 weeks and regular duty in 6 weeks.
Patients who have done tendon transfers or have some residual weakness. In that cases, patients return to light-duty work in around 6 to 8 weeks and regular duty in 10 to 12 weeks.
What is the complication of pronator teres syndrome?
After the surgical treatment complication is very rare. In one research study, 72 patients were treated with pronator teres syndrome, and no complications were recorded during the operations. And after the postoperative treatment satisfaction rate is 59%.
Theory basis complications of surgery include:
- Any Infection.
- Any type of hematoma formation.
- Nerve injury.
- Scar tissue formation.




3 Comments