Bulimia Nervosa
Table of Contents
Definition
Bulimia nervosa, usually called bulimia, is a serious, potentially life-threatening eating disorder. individuals with bulimia can secretly binge — eating greater amounts of food with a loss of control over the eating — and then purge, trying to get rid of the extra calories in an unhealthy way.
Criteria for Bulimia Nervosa
- Recurrent episodes of binge eating are distinguished by both:
- Eating, in a discrete period of time (for example within any two-hour period), a quantity of food that is definitely greater than most individuals would eat at that time a similar period of time and under common circumstances.
- A sense of lack of control over eating during the episode is defined by a feeling that one may not stop eating or control what or how much one is eating.
- Recurrent unsuitable compensatory behavior to prevent weight gain by:
- Self-induced vomiting
- Misapply laxatives, diuretics, enemas, or other medications
- Fasting
- Excessive exercise
- The binge eating and inappropriate compensatory behavior both happen, on average, at least twice a week for three months.
- Self-evaluation mostly depends on body shape and weight.
- The disturbance does not happen exclusively at the time of anorexia nervosa.
Types of Bulimia Nervosa
Purging type:
- At the time of the current episode of bulimia nervosa, an individual has regularly engaged in self-induced vomiting or the misuse of laxatives, diuretics, or enemas.
Nonpurging type:
At the time of the current episode of bulimia nervosa, an individual has used inappropriate compensatory behavior but has not daily engaged in self-induced vomiting or misused laxatives, diuretics, or enemas.
Prevalence
- The incidence of individuals suffering from bulimia has elevated over the last 30-40 years.
- Around one to two percent of women in late adolescence and adult females meet the diagnostic criteria for bulimia nervosa.
- About eighty percent of individuals with bulimia nervosa are women and 1.5% of American females suffer from bulimia nervosa in their lifetime.
- The Standard mortality ratio (SMR) for Bulimia Nervosa is 1.93.
Causes of Bulimia nervosa
- There have been no particular things proven to cause bulimia.
- Triggers to bulimia nervosa have been recommended, incorporating dieting, stress, emotions, and the need for control (to ease stress or anxiety in a person’s life).
- Factors that are recommended to contribute to bulimia involve culture, family history, stressful life events, personality, and biology.
- Infrequently it is one factor in causing bulimia, frequently it is found that genetics, psychological factors, family and societal pressures, and/or cultural influences.
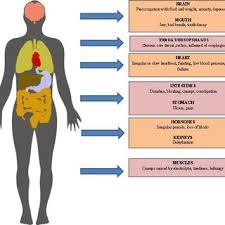
- Recent research reported that glucagon-like peptide 1 (GLP1) levels are low in people with bulimia nervosa. Systemic Involvement Complications from bulimia may involve:
- Tears in the esophagus
- Inflammation of the throat
- Enlarged glands near cheeks
- Pancreatitis
- Peptic ulcers
- Stomach damage
- Constipation and hemorrhoids
- Dental cavities and gum infections
- Dehydration and electrolyte imbalances
- Irregular heartbeat, heart failure, and death can occur secondary to the imbalances because of the loss of essential nutrients and electrolyte imbalances.”
Signs and symptoms of Bulimia nervosa

- Bulimia may affect anyone; men, women, young, old, and all races.
- These people may come up with normal weight or they can be underweight or overweight.
- The patient can use pills (diet pills, diuretics, or laxatives).
- They can frequently take trips to the bathroom after eating (recommend that they use this time to purge after a meal) and can exercise despite weather, injury, or energy levels to maintain their weight.
Signs of bingeing involve:
- The disappearance of greater amounts of food in a short time period.
- Finding wrappers/containers of eat-up food around the person’s living environment.
Signs of purging involve:
- Often trips to the bathroom after meals.
- Signs or smells of vomiting
- Proof of using laxatives/diuretics (wrappers, containers, etc.)
- Main motive and concern on weight loss, dieting, and controlling their food (intake/outtake)
- Excessive and rigid exercise routines (continued despite weather, illness, injury, and energy levels)
- Rigid schedules that permit time for binge/purge cycles
- Withdrawal from normal activities
Signs of self-induced vomiting involve:
- Swelling of the people’s cheeks/jaws
- Calluses or scrapes on the knuckles
- Clear-looking teeth
- Broken blood vessels in the eyes
- Can also come up with other mental health problems like depression, anxiety, substance abuse, distorted body image (thoughts and verbal expressions of hating body, pictures of being fat despite thin appearance, and fear of gaining weight), and reports from family and friends on activity not “normal” for the person (in the essence of moody, sad, unsociable)
Physical Signs and Symptoms may involve:
- Weight loss/gain
- Muscle weakness and/or myopathy
- Chronic fatigue
- Dehydration or rebound water retention
- Pitting edema
- Discoloration of teeth
- Broken blood vessels in eyes
- Enlarged salivary glands
- Scrapes/calluses on the dorsum of hands/fingers
- Inability to tolerate cold
- Irregular or absent menstrual cycles
- Delay in menses in young girls
- Dry skin and hair
- Hair loss
- Lanugo growth over the entire body
- Brittle nails
- Reports of heartburn, gas, constipation, or diarrhea
- Slow heart rate and low blood pressure
Behavioral signs and symptoms may involve:
- concentration Learn to pronounce weight, food, calories, fat grams, dieting, clothing size, and body shape
- Personality changes (in the essence of mood swings and irritability that can not have been present before)
- Binging and purging behaviors or food restriction behaviors
- Often trips to the bathroom after meals
- Distorted body pictures (both thoughts and verbal expressions of dissatisfaction, despite thin body)
- Excessive and rigid exercise routine
- Use of pills or other drugs to maintain weight (in the essence of diuretics, laxatives, enemas, etc.)
Associated Co-morbidities
- Frequent times bulimia nervosa is also connected with mental health disorders, like Depression, Anxiety, and Substance Abuse.
- Nearly half of the bulimia people have a comorbid mood disorder, more than half of bulimia people have comorbid anxiety disorders and nearly one in ten bulimia patients have a comorbid substance abuse disorder, generally alcohol use.
Diagnostic Tests
- In diagnosing bulimia nervosa, people must meet specific criteria.
- Patients may not simultaneously meet the diagnostic criteria for anorexia nervosa.
- To meet the bulimia nervosa standard, a patient binges and then engages in “inappropriate compensatory behavior at least twice weekly for at least 3 months.”
- Other exams, like dental exams, may help with identifying signs of excessive vomiting.
- Dental exams can reveal reduce enamel, cavities, and gum infection.
- Metabolic panels may show electrolyte imbalances (in essence hypokalemia) and help identify dehydration.
Differential Diagnosis
- Central Nervous System pathologies (in the essence of brain tumors) may stimulate bulimia.
- Kluver-Bucy Syndrome (symptoms involve hyperphagia, hypersexuality, and compulsive licking and biting) and Klein-Levin Syndrome (more usual in males; symptoms involve hyperphagia and period hypersomnia) should be ruled out.
- Patients must be screened carefully to correctly diagnose bulimia, versus the purging subtype of anorexia nervosa.
- Patients with borderline personality disorder can come up with binge eating tendencies; however, these patients will not meet the other diagnostic criteria for bulimia.
Treatment of Bulimia nervosa
Medications
- Anti-depressant medications have been found to be effective, specifically when merged with Cognitive Behavior Therapy, versus medication only or therapy only.
- SSRIs tend to be used primarily, as they tend to be both effective and safe. Fluoxetine (Prozac) is the only FDA-accepted anti-depressant medication for the treatment of bulimia.
- Bupropion (Wellbutrin) has been proven to be effective, however, contraindicated because of its connection with seizures in patients who purge.
- Anti-depressants are frequently used due to accompanying psychological symptoms (in the essence of anxiety, depression, etc.); however, studies have found these medications to be effective in people who do not have anxiety and/or depression co-morbidities.
- This recommends that anti-depressants may especially treat symptoms of bulimia (in the essence of binges, purging, and preoccupation with body image).
- Other medications that are gaining identification for effectiveness involve topiramate and ondansetron (Zofran).
- Topiramate is an anti-convulsant that has been found to be effective in reducing the frequency of bingeing and purging, as well as increasing the connected psychological co-morbidities.
- Mild to moderate adverse side effects have been found with using topiramate in people with bulimia; however, this finding was based on a little study and would need further research.
- Ondansetron is an anti-emetic utilized in cancer patients to help prevent nausea and vomiting.
- Findings are dependent on small studies, further research is required to address all aspects of how this anti-emetic could effectively treat bulimia.
Medical Treatment
- Typical treatment for people with bulimia nervosa includes a multi-disciplinary approach; a treatment team generally includes a primary care physician, a dietitian/nutritionist, a mental health doctor, as well as nurses and other supportive medical personnel.
- The treatment process: the primary assessment addresses the patient’s past medical history, current symptoms, current physical and mental status, the way the people control their weight, and any psychiatric issues/disorders (in essence depression, anxiety, etc.).
- A physician and dietitian are asked, to develop a diagnosis and place of care for the patient.
- Most individuals with bulimia are treated on an outpatient basis; although their treatment is coordinated between their physician, psychotherapist, and dietitian.
- Some people choose to be treated without mental health professionals, while others only receive treatment from mental health professionals. Psychotherapy includes cognitive-behavioral therapy, behavior therapy, family therapy, and interpersonal psychotherapy.
- Some patients are successful with short-term treatments like these, while others require long-term.
- Some people are treated with psychopharmacology.
- Psychiatric medications have been found to be successful in treating people with bulimia; these medications frequently involve anti-depressants.
- Nutritional counseling is also a treatment option and a vital component for people diagnosed with an eating disorder.
- Dietitians serve as educators to both the patient and their families.
- Dietitians help people with bulimia to normalize their eating behaviors.
- Some people diagnosed with bulimia have complications secondary to their disorder, thus requiring treatment beyond that for
- their eating disorder.
- These treatments vary according to the severity of systemic involvement and complications.
Indications for Hospitalization:
- Weight <75% of individually estimated healthy weight
- The quick, persistent decline in oral intake or weight despite maximally intensive outpatient interventions.
- Initial knowledge of the weight at which physical instability is likely to happen in the particular patient.
Serious physical abnormalities:
- Electrolyte or metabolic abnormalities
- Hematemesis
- Vital sign changes involving orthostatic hypotension and heart rate <40 bpm or >110 bpm
- Inability to sustain body core temperature
- Comorbid psychiatric illness (suicidal, depressed, unable to care for self)”
- In severe cases of bulimia, people need in-patient treatment.
- This treatment gives the patient a more structured environment, giving treatment and monitoring 24 hours a day, every day of the week.
- These programs are frequently arranged in “step up” and “step down” levels allowing people to progress (or for some, regress) in their treatment accordingly.
- For patients that require it, long-term in-patient programs are also available (in the essence of residential treatment programs).
Cognitive behavior therapy (CBT)
CBT for bulimia nervosa (CBT-BN), a specially adapted form of CBT, should be offered to adults with bulimia nervosa. This course of treatment should be for 10 to 15 sessions over 3 to 6 months.
(Grade A)
- When people with bulimia nervosa have not responded to or do not want CBT, other psychological treatments should be included.
(Grade B)
- Interpersonal psychotherapy should be included as an alternative to CBT, but people should be informed it takes eight to twelve months to achieve results comparable to CBT.
- (Level B) People should be informed that antidepressant drugs may decrease the frequency of binge eating and purging, but the long-term effects are unknown.
- (Grade B) SRIs, especially fluoxetine are the drugs of first choice for the treatment of bulimia nervosa in terms of acceptability, tolerability, and declination of symptoms.
- (Grade B) The compound of CBT with antidepressant drugs is superior to antidepressant drugs on their own.
Physical Therapy Treatment
- Physiotherapists working under the practice patterns of “4A Primary Prevention/Risk.
- Reduction for Skeletal Demineralization, 4B Impaired Posture, 4C Impaired Muscle Performance (specifically with malnutrition and fluid/electrolyte disturbances), 6A Primary Prevention/Risk.
- Declination for Cardiovascular/Pulmonary Disorders, 6B Impaired Aerobic Capacity/Endurance.
- Connected with De-conditioning, 7A Primary Prevention/Risk Reduction for Integumentary Disorders (malnutrition)” may help in the treatment of patients with bulimia nervosa.
- On the basis of the Guide for Physical Therapist Practice, physical therapists work preventatively or retrospectively with people suffering from complications secondary to eating disorders.
- Some physical therapists may rehabilitate a person, who in addition to having an orthopedic problem for example, also has an eating disorder (whether identified to the therapist or not).
- Physiotherapists may help with the initial screening and detection of and for eating disorders.
- The more informed a therapist may be, the more they are able to give the appropriate evaluations and interventions for their patients, helping to reduce the consequences and complications of the eating disorder.
- Identifying at-risk patient populations may also help with early detection; in the essence young, women athletes are at a higher risk for the female athlete triad.
- At-risk patient populations may involve women, those with a perfectionist personality, Caucasians, personal and/or family history of eating disorders or obesity, athletes, and patients with a history of trauma or sexual abuse.
- As a physiotherapist, identifying and being aware of patients with distorted body images or distorted eating habits is also necessary.
- In some sports individuals who compete in underweight classes or must build up their bodies for competition may be at risk for developing eating disorders.
Some questions to review as physical therapists screening for eating disorders involve:
- Are you satisfied with your eating patterns?
- Do a person force themselves to exercise, even when a person does not feel well?
- Does a person exercise more when they eat more?
- Does a person think he will gain weight if he stops exercising for a day or two?
- Does a person exercise more than once a day?
- Does a person take laxatives/diuretics/any other pills as a way to control weight or shape?
- Does a person ever eat in secret (in the essence of in closets or bathrooms to avoid being seen eating)?
- Are there days when a person does not eat anything?
- Does a person ever make himself throw up after eating as a way to control the weight?
The SCOFF Questionaire:
- Does a person ever make herself Sick because she feels uncomfortably full?
- Does a person worry have lost Control over how much he eats?
- Have people recently lost more than One stone in a three-month period?
- Do people believe themself to be Fat when others say they are too thin?
- Would people say that Food dominates life?
- One point is given for every ‘yes’ answer. A score of 2 or more indicates possible anorexia nervosa or bulimia nervosa.
- *Note: 1 stone is approximately 6.35 kg”
- Bulimia collision a patient’s fluid and electrolyte balance, putting them at risk for fluid depletion and ineffective temperature regulation.
- These, in addition to the use of self-induced vomiting or laxatives, may put the patient at very high risk for dehydration and loss of potassium. Patients with these complications can primarily come up with muscle cramping, fatigue, as well as orthostatic hypotension.
- A physical therapist can have to stop treatment of their patient until fluid and electrolyte imbalances are normalized.
- It is necessary that the physical therapist motivate their patient to drink a handsome amount of fluids and decrease their activity until levels are normalized.
- Patients with severe dehydration and electrolyte imbalances can come up with confusion, disorientation, and uncoordinated movements.
- These patients should be sent for quick medical attention.
- Another deliberation for physical therapists is the effects bulimia may have on bone; patients presenting with an orthopedic problem can also have bulimia.
- Frequent times, bone integrity is weakened, which is something a therapist should be aware of if thrust manipulations are being considered in the treatment plan.
FAQ
Episodes of binge eating.
Self-induced vomiting.
Smelling like vomit.
Misuse of laxatives and diuretics.
Complaining about body image.
Expressing guilt or shame about eating.
Depression.
Irritability.
Persistent acid reflux.
Erosion of dentin and enamel on teeth.
Hoarse voice (damage to vocal cords)
Cardiac arrhythmia.
Adverse gastrointestinal effects.
Risk of cathartic colon syndrome (due to laxative abuse)
Bulimia may permanently damage the stomach and intestines, causing other problems such as constipation, diarrhea, and irritable bowel syndrome. Hormonal problems. Reproductive issues, involving irregular periods, missed periods, and fertility problems are usual side effects when people have bulimia.
Another study of 246 females diagnosed with anorexia or bulimia reported 11 (4.5%) died from their illness over the period of time. Of these women, ten had intake diagnoses of anorexia and one had bulimia. This research reinforces the aforementioned one, finding anorexia more lethal than bulimia.
Research shows that the frequency of binge eating episodes among bulimics varies from one per week to forty-six times. The average is once daily, with the number of calories consumed in the binge ranging from 1,200 to 11,500 for individuals with typical bulimia.