Costochondritis
Table of Contents
Definition
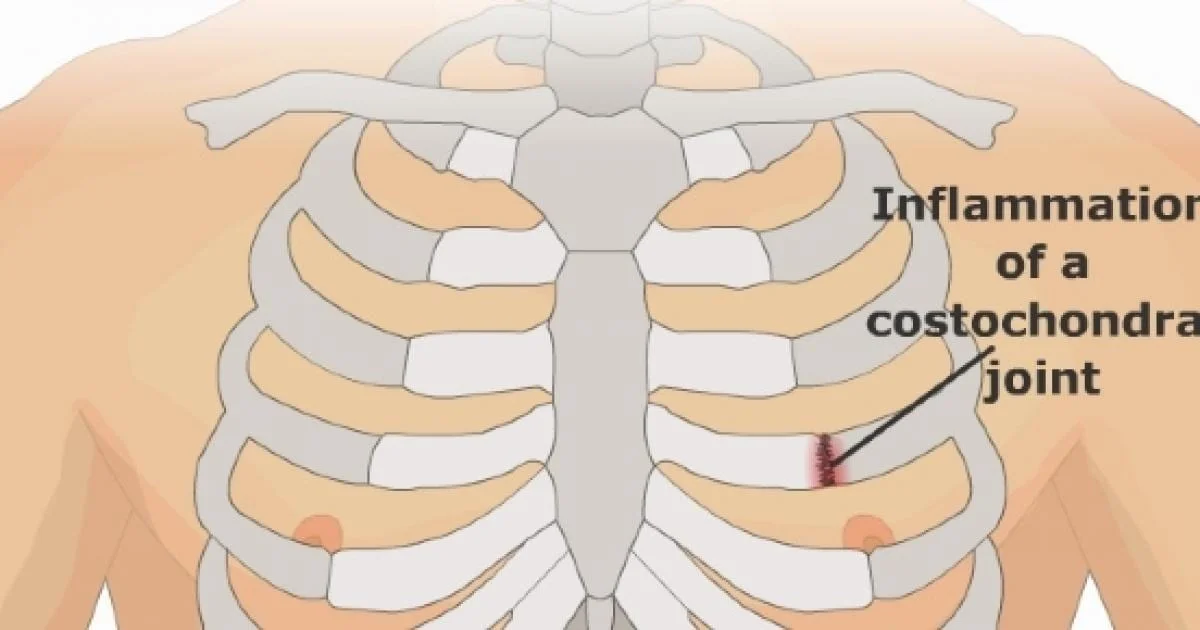
Costochondritis is a self-limiting condition known as painful chronic inflammation of the costochondral junctions of ribs or chondrosternal joints of the anterior chest wall. It is a clinical diagnosis and does not need any specific diagnostic testing in the absence of concomitant cardiopulmonary symptoms or risk factors.
Costochondritis is often confused with Tietze syndrome. Palpation of the involved chondrosternal joints of the chest wall elicits tenderness and pain is reproduced by palpation of involved cartilage segments which can radiate out into the chest wall.
Clinically Relevant Anatomy
The thoracic wall consists of the:
- Sternum anteriorly,
- 12 thoracic vertebrae posteriorly,
- Rib Cage 12 paired ribs and connected costal cartilages.
- Ribs are made up of bone and cartilage, with cartilage serving as an elastic bridge between the bony portion of the rib and the sternum.
- on the basis of their attachment to the sternum, the ribs are classified into 3 groups: true, false, and floating ribs.
True ribs
- These ribs are the ribs that directly articulate with the sternum with their costal cartilages – ribs 1-7.
- They are eloquent with the sternum by the sternocostal joints.
- The foremost rib is an exception to that rule; it is a synarthrosis and the first rib could eccentrically articulate with the clavicle by the costoclavicular joint.
The false ribs (8,9,10)
- These ribs are the ribs that indirectly articulate with the sternum, as their costal cartilages are associated with the seventh costal cartilage by the costochondral joint.
The floating ribs (11,12)
- These ribs do not articulate with the sternum at all (distal two ribs).
- The ribs proceed with respiration and with truncal motion or movement of the upper extremities.
What are the Causes of Costochondritis?
Costochondritis is inflammatory. It is the cause of inflammation of the costal cartilages and their sternal articulations, also identify as the costochondral junctions. Doctors do not know perfectly why costochondritis happens, but they do know that some things may lead to it:
- Repeated minor trauma to the chest wall
- Overuse of the arms
- Arthritis- Costochondritis may sometimes be a sign of osteoarthritis, rheumatoid arthritis, ankylosing spondylitis, or other conditions that affect the cartilage.
- Tumors- These may move from joints and other parts of the body and settle in the chest.
- Respiratory infections caused by viruses
- Bacterial infections, specifically in people who use IV drugs or have had surgery near their upper chest
- Fungal infections (in rare cases)
Symptoms of Costochondritis
As with any chest pain, a history of current illness, past medical history, social history, family history, and a review of systems are very important. Too many deadly causes of chest pain should be ruled out prior to accepting a diagnosis of costochondritis. Possible findings include
- The person will give a history of the pain worsening with movement and a few positions.
- The pain will also usually be worse when the patient takes a deep breath.
- Pain quality is variable, but it can be described as a sharp or dull pain.
- The person reports a gradual or rapid onset of pain and swelling of the upper costal cartilage of the costochondral junction.
- Pain is generally reproducible by mild-to-moderate palpation.
- Frequently, there is point tenderness where one or two ribs meet the sternum (a pitfall of the typical physical exam findings is that pain because of the acute coronary syndrome may also be described as reproducible).
- Symptoms can happen slowly and may disappear spontaneously after some days, but equally, it can take years to disappear.
- Even after the symptoms have resolved, they can return at the same location or at another rib level.
- There can be hypomobility of the upper thoracic spine, costovertebral joints, and lateral ribs.
Differential Diagnosis
The differential diagnosis for costochondritis is rather long. Some of the diagnoses involved are connected with major morbidity and mortality. For example
- Acute Coronary Syndrome (ACS)
- Pneumothorax
- Pneumonia
- Pulmonary Embolism
- Tietze’s syndrome is much list common than costochondritis, and it tends to cause chest swelling in addition to the other symptoms,
- Xiphoidalgia: Unpleasant swelling and discomfort of the xiphoid process of the sternum.
- Slipping rib syndrome: Hypermobility of the anterior edge of the false rib costal cartilages.
Diagnosis
It includes evaluation,examination, and outcome measures, which help the physician to guide in the right direction for the diagnosis of costochondritis.
Evaluation
Costochondritis is generally self-limited and benign – should be characterized by other, more serious causes of chest pain.
- Coronary artery disease is existing in 3 to 6 percent of adult patients with chest pain and chest wall tenderness to palpation.
- History and physical examination of the chest that report reproducible pain by palpation over the costal cartilage are usually all that is required to make the diagnosis in children, adolescents, and young adults.
- A person older than 35 years, those with a prior history or risk of coronary artery disease, and any person with cardiopulmonary symptoms should have an electrocardiograph and possibly a chest radiograph.
- Think about further testing to find out cardiac causes if clinically indicated by age or cardiac risk status.
Examination
Patients with Costochondritis will present with:
- Chest pain is reproducible by palpation of the affected area, with ribs 2 to 5 generally affected.
- Aggravating factors may be slouching or exercise.
- Frequently happen after a recent illness with coughing or after intense exercise and it is mostly of unilateral origin.
- Can be connected restriction of the corresponding costovertebral and costotransverse on examination.
- Loss of normal spinal movement connected with chest pain.
- Palpation should be done with 1 digit, on the anterior, posterior, and lateral sides of the chest, the clavicle, and the cervical, and thoracic spine.
- When on the involved area it reveals a reproducible pain which might suggest Costochondritis, but it may not be entirely concluded.
- Movement palpation is a manual process of moving the joint into its maximal end range of motion, after which it is challenged with a light springing motion.
- This endpoint of joint movement creates the basis for determining normal or abnormal joint movement.
- When motion palpation is decreased, the joint is considered fixated or hypokinetic.
- Cardiac causes should find out in patients who present with high risk.
Outcome Measures
Patient-specific functional scale ( PSFS)
- Particular questionnaires for costochondritis have not yet been constructed, but the PSFS is a reasonable, reproducible, and responsive outcome measure for persons with neck pain, back pain, and upper quarter complaints.
The Global rating of change (GROC):
- To measure the person’s subjective rate of improvement.
Measurement of thoracic and cervical mobility:
Rotation of the thoracolumbar spine (TR):
- TR has high validity and sensitivity ranks and improvement of the measurement technology would generally result in a superior test for the follow-up.
Finger-to-floor distance (FFD):
- High reliability and sensitivity, but poor correlation with spinal changes.
Other measures
- The Schober test.
- Thoracolumbar flexion.
- Occiput to wall distance.
Medical Management
Treatment included conservative management and is generally symptomatic, Management includes:
Topical or oral analgesics
- Local injections with a steroid into the joint, tendon sheath, or around the nerve, inhibits inflammation and decrease swelling and pain to upgrade movement.
- If the person has severe or refractory costochondritis, refer for outpatient follow-up. Physiotherapy is a treatment choice for refractory costochondritis
- Some alternative treatments can also involve ice, acupuncture, manual therapy, exercise, and other medications like sulfasalazine which can have an additional long-term benefit in the management of costochondritis.
Costochondritis Physical Therapy
- Physical therapy for costochondritis includes helping the patient to manage their pain, reducing inflammation, and improving the way the patient move to decrease the pressure off inflamed rib cartilage.
- Most individuals with costochondritis well-being from working with an orthopedic physical therapist, an expert in the treatment of musculoskeletal conditions.
An Overview of Orthopedic Physical Therapy
Different modalities and maneuvers can be used to upgrade the way you move. These may include:
- Rib mobilizations help upgrade the way your ribs move up and down during normal respiration.
- Spinal joint mobilizations to upgrade the way your thoracic spinal joints glide and slide together.
- Range of motion and stretching exercises that may take pressure off inflamed rib cartilage and permit improved freedom of movement.
- Postural strengthening exercises to help maintain proper positions that keep pressure off the rib cartilage.
- Breathing exercises improve the way ribs move while a person is taking deep breaths.
- Other treatments can be utilized to help to reduce pain and inflammation.
- These can incorporate heat to upgrade circulation and ice to reduce pain and swelling nearby the inflamed tissues.
- Other treatments, like ultrasound or electrical stimulation, are not used, as the cartilage involved is close to the heart.
- Performing these procedures near the cardiac structures is not suggested.
- Active involvement in the therapy is key.
- The therapist will likely prescribe exercises to help their ribs and thorax (chest) move better.
Costochondritis Exercises
Exercises for costochondritis are designed to upgrade overall chest wall and rib mobility. This may help reduce the pain and upgrade the way the ribs and thorax move. Postural exercises may relieve the pressure of inflamed cartilage. prior to starting any exercise program for costochondritis, check in with the doctor to ensure that exercise is safe for you to do.
Breathing exercise
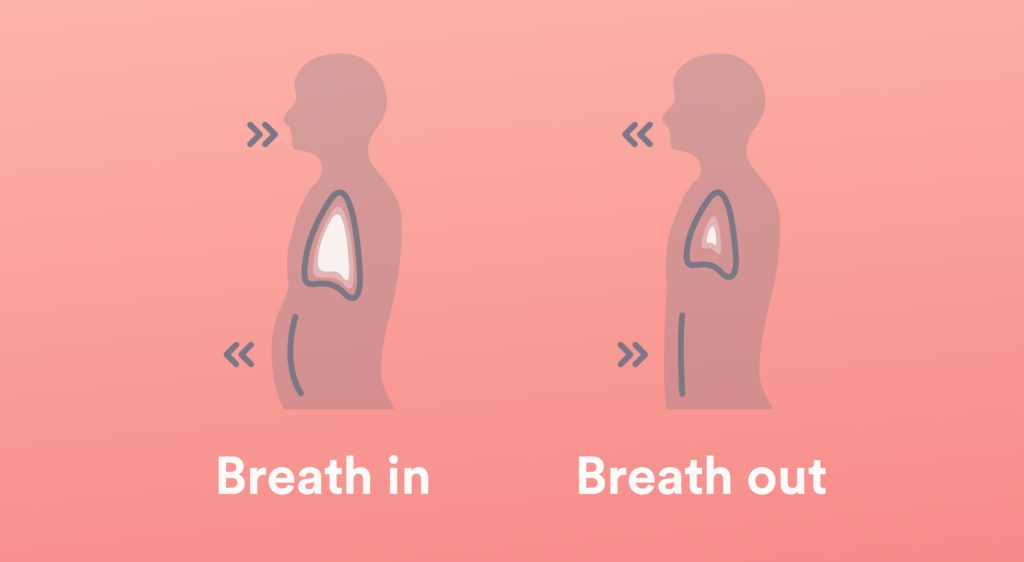
- To do Deep breathing exercises – Sit upright in a comfortable chair with the feet placed side by side on the floor.
- Close your eyes.
- Place one hand on the belly, with the pinky finger just above the belly button.
- Initiate paying attention to the rise and fall of the belly. What you are feeling is the diaphragm, working to draw air in and out of the lungs.
- Notice that as you breathe in, it feels like a balloon is being filled with the hand.
- As the person breathes out it should experience like the balloon is deflating.
- Place the other hand on the chest.
- The person will want to try to keep up this hand as still as possible and to just let the diaphragm do all of the work of breathing.
- While you are at it, keep the shoulders relaxed — the person does not need the shoulders to breathe! Inhale calmly to the count of three.
- Then exhale gently to the count of three, thinking the word “relax” as you do so.
- Stay focused on the action of the diaphragm.
- The bottom hand should move outward as the person fills their lungs with air and move inward as you exhale.
Pectoral Corner Stretch

- The pectoral corner stretch is meant to improve the flexibility of the pectoral, or chest, muscles.
- To do the stretch, start by standing facing a corner about two feet away from the wall.
- Put both arms up, with the forearms resting against the wall on each side of the corner.
- The hands, forearms, and elbows, all should be in contact with the wall.
- Slowly lean into the corner, stretching the muscles in the front of the chest.
- Hold the stretch for ten to twenty seconds, and then relax.
- Repeat the stretch 4 to 5 times.
Pectoral Doorway Stretch

- The patient can stretch the pecs using a doorway opening, too.
- To perform this stretch, stand in a doorway, and put both elbows and forearms up against the doorjamb on either side of the person.
- While keeping up the elbows against the doorjamb, slowly lean forward, stretching the muscles in the front of the chest.
- Hold the stretch for twenty to thirty seconds, and repeat 3 to 5 times.
Scapula Squeeze
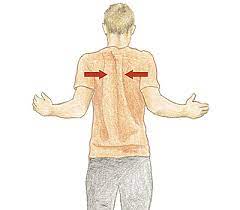
- The scapula squeeze may be done to improve posture and muscular control of the thorax.
- To do this exercise, sit comfortably in a chair, and slowly squeeze the shoulder blades together in the back.
- Pretend that you are trying to squeeze a pencil between the shoulder blades, and hold the position for 3 seconds.
- Slowly release, and return to the starting position.
- Repeat 15 to 20 times.
The scapula squeeze exercise may be more challenging with a resistance band. Loop the band around something stable, and grasp each end. Bend the elbows back, as if rowing a boat, while pinching the scapulae together. Then gently release, and repeat the exercise 15 to 20 times.
Stability Ball Lying Chest Stretch

- Another great way to open up the chest wall and stretch the pectorals and chest muscles is to use a stability ball.
- To perform this stretch, lie on the back over a 65-centimeter stability ball.
- Hold both arms up in front of you, and then gently open up the arms as if you were going to give someone a big hug.
- Relax the back as you open the arms, and allow the arms to move toward the floor, opening up the chest.
- The person should experience a slight pulling sensation in the chest when you perform the exercise.
- Hold the stretch for 20 to 30 seconds, and then bring the arms back to the midline.
- Repeat 3 to 5 times. If any exercise gives you lasting pain in the chest or ribs, stop it and check in with the physical therapist.
- Frequent, alterations may be made to make the exercises more comfortable.
Prevention
One important component of any good physical therapy program is learning to prevent future problems with the condition. Prevention of costochondritis may involve:
- Attaining and maintaining appropriate posture.
- Do regular stretching a few times each week.
- Working on strengthening back and abdominal muscles.
- Engaging in regular physical exercise.
- If you start to feel the symptoms of costochondritis creeping on again, performing the home exercise program for stretching, breathing, and postural exercises can help keep symptoms under control.
FAQ
Costochondritis is the medical term for inflammation of the cartilage that joins the ribs to the breastbone (sternum). This area is identified as the costochondral joint. Cartilage is a tough but flexible connective tissue found throughout the body, involving the joints between bones.
Costochondritis typically has no clear cause. Although, costochondritis might be connected with trauma, illness, or physical strain, like severe coughing.
Costochondritis is inflammation where the ribs connect the bone in the middle of the chest (breastbone). It may cause sharp chest pain, specifically when moving or breathing. It generally gets better on its own over time.
Other medical conditions that can closely resemble costochondritis involve:
Arthritis of the shoulder or surrounding joints.
Chest wall infections or cancer.
Fibromyalgia is a condition that causes nerve pain.
Slipping rib syndrome, when there is redundant mobility in the cartilage supporting the ribs.
A chest x-ray should be considered in all patients with chest wall pain or chest pain to find out pneumonia, spontaneous pneumothorax, and lung mass, among others. A usual chest x-ray will be seen with costochondritis.





3 Comments