Plica Syndrome
Table of Contents
What is Plica Syndrome?
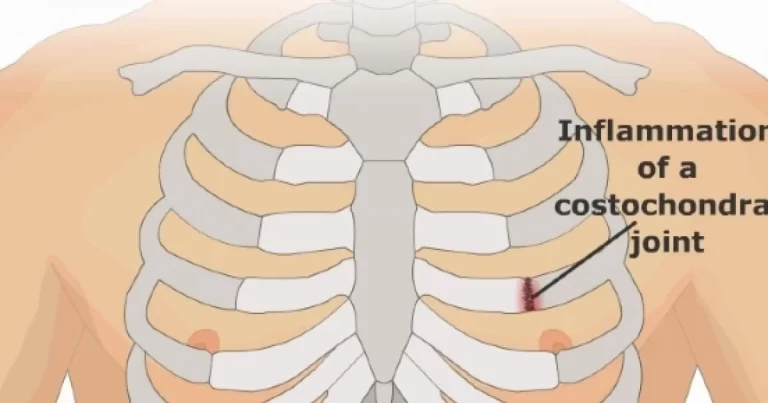
Plica syndrome is a condition where the plica, a fold of tissue in the knee joint, becomes irritated or inflamed, causing pain and discomfort. It’s typically due to overuse or repetitive motions and can lead to symptoms like knee pain, swelling, and a clicking sensation.
Treatment may involve rest, physical therapy, anti-inflammatory drugs, or in some cases, surgical intervention. If you’re experiencing symptoms, it’s important to consult a medical professional for an accurate diagnosis and appropriate treatment.
Causes of Plica Syndrome
Plica syndrome is typically caused by irritation or inflammation of the plica, which is a remnant of tissue that forms during fetal development. The exact cause of this irritation can vary, but it’s often associated with repetitive knee movements, overuse, or direct trauma to the knee.
Activities that involve frequent bending, squatting, or kneeling may increase the risk of developing plica syndrome. Additionally, structural issues in the knee joint or a history of previous knee injuries can also contribute to the condition.
- Repetitive Movements: Repeated activities that involve bending, straightening, or rotating the knee joint can lead to irritation and inflammation of the plica.
- Trauma: Direct impact or trauma to the knee can result in irritation of the plica, leading to its inflammation.
- Overuse: Engaging in activities that put excessive strain on the knee joint, especially without proper rest or recovery, can contribute to the development of plica syndrome.
- Muscle Imbalances: Weak or imbalanced muscles around the knee can affect the joint’s stability and mechanics, potentially leading to plica irritation.
- Infection or Inflammation: In some cases, infections or inflammatory conditions in the knee joint can lead to the formation of scar tissue and irritation of the plica.
Risk Factors
- Repetitive Movements: Activities that involve repetitive bending, squatting, or kneeling can irritate the plica and increase the risk.
- Overuse: Engaging in activities that strain the knee joint excessively, such as running or jumping,can contribute to plica irritation.
- Knee Injuries: A history of knee injuries, surgeries, or trauma can lead to structural changes in the knee joint, making it more susceptible to plica irritation.
- Muscle Imbalances: Imbalances in the muscles around the knee can alter the joint mechanics and contribute to plica syndrome.
- Anatomical Factors: Some individuals may have a naturally larger or more prominent plica, increasing the likelihood of irritation.
- Improper Biomechanics: Poor alignment or mechanics during movement can place extra stress on the knee joint and the plica.
- Age: Plica syndrome is seen in adolescents and young adults.
- Occupation: Occupations that involve repetitive knee movements or prolonged periods of kneeling can elevate the risk.
Symptoms of Plica Syndrome
- Pain with Activity: The pain may worsen during activities that involve bending the knee, such as walking, climbing stairs, or running.
- Localized Tenderness: There might be tenderness when pressing on the area around the plica or along the inner side of the knee joint.
- Knee Stiffness: Individuals with plica syndrome might experience stiffness in the knee joint, particularly after periods of rest or inactivity.
- Sensation of Locking: Some people might feel as though their knee “locks” or gets stuck in a certain position temporarily, due to the irritated plica getting caught in the joint.
- Sensation of Giving Way: The knee might feel unstable or as if it’s going to give way, especially during movements that cause the plica to catch or fold.
- Swelling: Inflammation of the plica can lead to localized swelling around the knee joint.
- Pain Along the Joint Line: Pain might be felt along the inner side of the knee, where the plica tissue is located.
- Limited Range of Motion: Some individuals might experience difficulty fully bending or straightening the knee due to the discomfort caused by the inflamed plica.
Diagnosis
Diagnosing plica syndrome typically involves a combination of medical history, physical examination, and sometimes imaging studies.
- Medical History: Your healthcare provider will ask you about your symptoms, when they started, and any activities that might have triggered them. They will also inquire about any previous knee injuries or surgeries.
- Physical Examination: The doctor will examine your knee, looking for signs of swelling, tenderness, and any unusual sensations like clicking or catching. They may manipulate your knee joint to assess its range of motion and to identify any specific areas of discomfort.
- Imaging Studies: While not always necessary, imaging tests like X-rays or MRI scans may be used to rule out other conditions and get a better view of the knee’s internal structures. They can help confirm the diagnosis by visualizing any inflammation or structural issues with the plica.
- Diagnostic Injections: In some cases, a diagnostic injection of a local anesthetic into the area around the plica can help determine if the symptoms improve, which can further support the diagnosis.
Medical Treatment of Plica Syndrome
- Anti-Inflammatory Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) can help decrease pain and inflammation. However, these should be used under medical treatment supervision.
- Ice and Elevation: Applying ice and elevating your leg can help reduce swelling and provide relief.
- Corticosteroid Injections: In some cases, a corticosteroid injection into the knee joint may be recommended to reduce inflammation and alleviate symptoms.
- Pain Management: Over-the-counter pain reliever drugs may be recommended to manage discomfort.
- Rest and Activity Modification: Giving your knee time to rest and avoiding activities that worsen symptoms can help reduce irritation and inflammation of the plica.
Physiotherapy Treatment of Plica Syndrome
- Physiotherapy plays a crucial role in the treatment of plica syndrome by addressing pain, improving joint mobility, and strengthening the muscles around the knee. Here’s how physiotherapy treatment for plica syndrome might be approached:
- Assessment: A physiotherapist will assess your knee’s range of motion, strength, and overall function. They will also discuss your symptoms and medical history to tailor the treatment plan to your specific needs.
- Manual Therapy: Hands-on techniques such as joint mobilizations and soft tissue massage may be used to improve joint mobility and reduce muscle tension.
- Stretching: Gentle stretching exercises can help improve flexibility and reduce tightness in the muscles around the knee.
- Strengthening Exercises: Strengthening the muscles that support the knee joint is essential. Exercises may target the quadriceps, hamstrings, calf muscles, and hip muscles to promote better knee alignment and stability.
- Functional Training: Physiotherapists often work on activities that mimic your daily movements to improve functional strength and stability.
- Biomechanical Corrections: The therapist may identify and correct any abnormal movement patterns that contribute to plica irritation, helping you move more efficiently and reduce stress on the knee joint.
- Electrotherapy: Modalities such as ultrasound or electrical stimulation might be used to reduce pain and promote healing.
- Home Exercise Program: Your physiotherapist will likely provide you with a set of exercises to continue at home, which will help reinforce the progress made during sessions.
- Education: You’ll receive guidance on proper posture, movement mechanics, and strategies to manage symptoms on your own.
- Progress Monitoring: Your physiotherapist will track your progress over time, adjusting the treatment plan as needed to ensure optimal results.
- Bracing: Using a knee brace or support can help stabilize the joint and provide relief during activities.
- Activity Modification: Adjusting your activities to minimize movements that exacerbate symptoms can aid in recovery.
Exercise
Certainly, here are some exercises that a physiotherapist might recommend to help manage and alleviate symptoms of plica syndrome:
Quad Sets: Sit on the floor with the patient’s legs straight. Tighten your thigh muscles (quadriceps) and press the back of your knee into the floor. Hold for a few seconds and then relax position. Repeat for several repetitions.
Straight Leg Raises: Lie on the patient’s back with one leg straight and the other bent. Lift the straight leg a few inches off the ground, hold it for a few seconds, and lower it back down. This exercise strengthens the quadriceps.

Hamstring Stretches: Lie on the patient’s back and gently pull one knee toward the patient’s chest. Straighten the leg as much as possible while keeping the opposite leg flat. You should feel a gentle stretch in the back of the thigh.

Calf Stretches: Stand facing a wall with the patient’s hands on the wall. Step one leg back and keep it straight. Bend the front knee while keeping the back heel on the ground, feeling a stretch in the calf muscle.

Inner Thigh Stretch: Sit on the floor and place the soles of your feet together. Gently press your knees toward the ground to feel a stretch in the inner thighs.
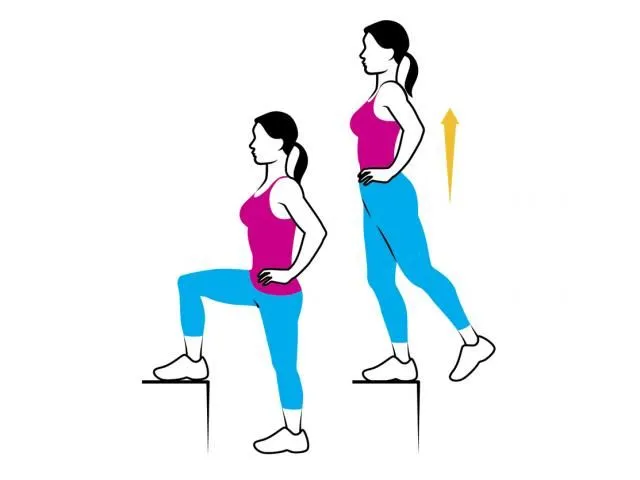
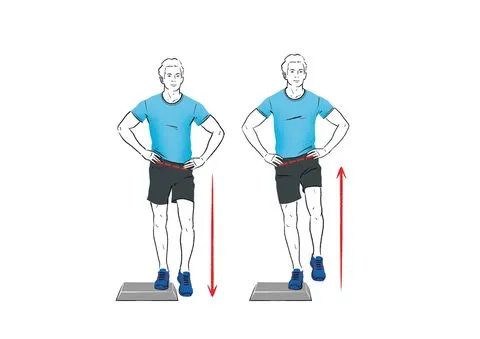
Step-Ups: Stand position in front of a step or low platform. Step up with one leg and then step down position. Repeat on the same leg for a set of repetitions before switching to the other leg.

Mini Squats: Stand with your feet hip-width apart. Bend your knees slightly, as if sitting back into a chair, and then straighten up. This mini squat exercise helps strengthen the muscles around the knee.

Lateral Leg Raises: Stand next to a wall or support for balance. raise one leg out to the side, keeping it straight, and then lower it back down. This leg raise exercise targets the hip abductor muscles.
Bridges: Lie on the patient’s back with your knees bent and feet flat on the floor. Squeezing your glutes, raise your hips off the ground, and then lower them back down.

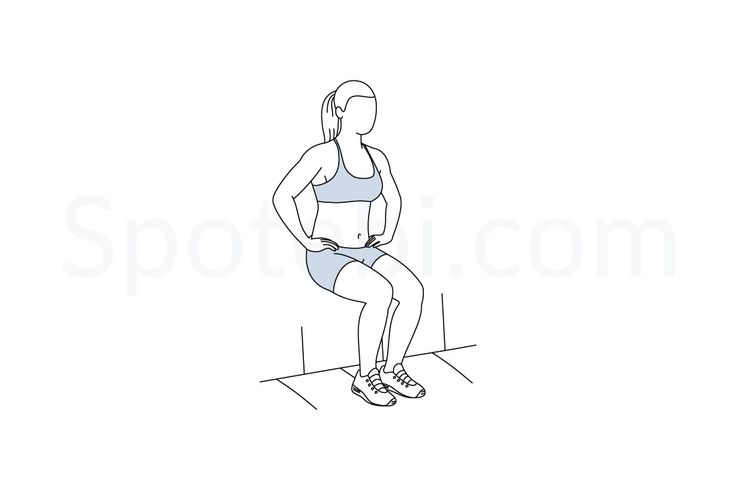
Wall Slides: Lean your back against a wall and slide down into a squatting position. Keep the patient’s back against the wall and your knees aligned with your feet. Hold the position for 10 to 15 seconds before sliding back up.
Clamshells: Lie on the patient’s side with your knees bent and your feet together. Keeping the patient’s feet touching, lift your top knee as high as the patient can without moving your pelvis. Lower it back down. This clamshell exercise targets the hip abductor muscles.
Seated Knee Extension: Sit in a chair with your knees bent at 90 degrees. Slowly extend one leg out in front of the patient, straightening the knee. After a brief period of holding, lower the leg back down.
Heel Slides: Lie on the patient’s back with your legs straight. Slide one heel up toward your buttocks by bending the knee, and then slide it back down. This exercise helps with knee mobility.

Hamstring Curls: If you have access to a resistance band, attach it around your ankle and lie on your stomach. Bend your knee to bring your heel toward your buttocks, resisting the band’s pull. Slowly straighten your leg back out.
IT Band Stretch: Cross one leg in front of the other and reach your arm over your head to the opposite side. Lean your upper body to the side, feeling a stretch along the outer part of the leg.

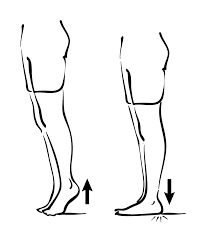
Standing Calf Raises: Stand with your feet flat on the ground. Rise up onto the patient’s toes, lifting your heels off the floor. Lower the patient’s heels back down to the floor.
Isometric Quad Contractions: Sit on the edge of a chair with your knees bent at a 90-degree angle. Press your knee down into the chair, engaging your quadriceps. Hold the contraction for 10 to 15 seconds and then relax.
Step-Ups with Knee Lift: Similar to regular step-ups, but after stepping onto the platform, lift the opposite knee up toward your chest before stepping down.
Resistance Band Leg Abduction: Place a resistance band around your ankles and stand with your feet hip-width apart. Keeping your legs straight, lift one leg out to the side against the resistance of the band.
Foam Roller Exercises: Gently roll a foam roller along the outside of your thigh and calf muscles to help release tension and improve blood flow.
Ankle Pumps: Lie on your back and gently move your ankles up and down in a pumping motion. This helps improve circulation and reduce stiffness.

Quadruped Hip Circles: Get on your hands and knees. Keeping your back flat, draw circles with your knee of the affected leg while maintaining stability in the core.
Prone Hangs: Lie on your stomach and let your legs hang off the edge of a bed or table. This can help gently stretch the front of the thigh.
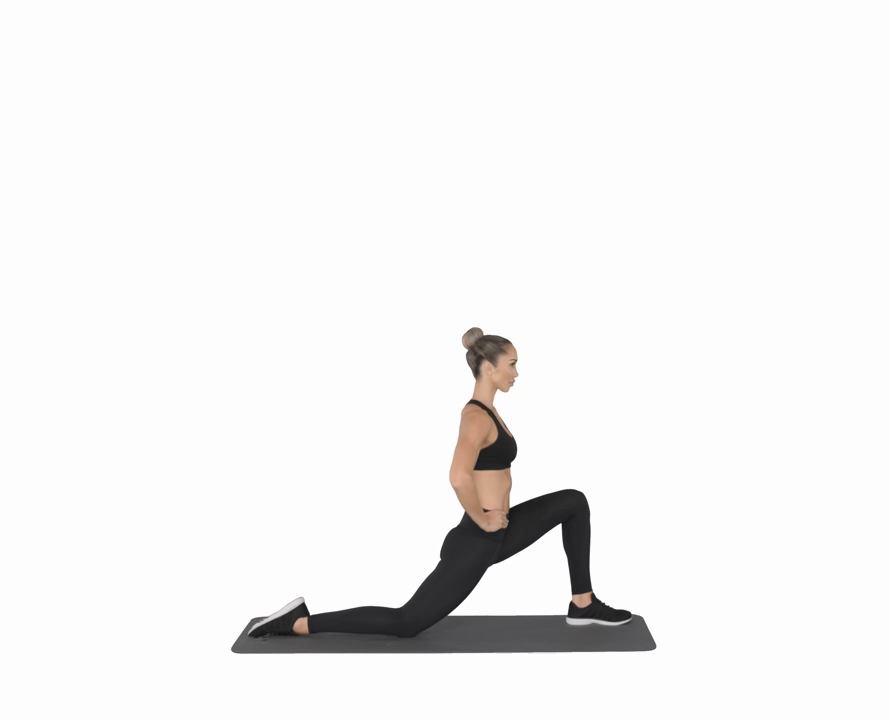
Hip Flexor Stretch: Kneel position on one knee with the other foot in front. To feel a stretch near the front of the kneeling leg’s hip, lean forward.
Seated Wall Slides: Sit against a wall with your normal knees bent. Slowly slide your feet away from the wall, straightening your knees. Then slide your feet back up to a bent position.

Quad Foam Rolling: Lie on your stomach and place a foam roller under your thighs. Gently roll back and forth to massage the front of your thighs.

Dynamic Hamstring Stretch: While standing, extend one leg in front of you and reach for your toes. Then swing the leg behind you while bending at the waist, stretching the hamstrings.
Seated Leg Extension with Resistance Band: Sit on the edge of a chair with a resistance band around your ankle. Extend your leg out in front of you against the resistance of the band.
Single-Leg Balance: Stand on one leg and try to maintain the patient’s balance. This helps improve stability and engages the muscles around the knee.

Stationary Bike: Gentle cycling on a stationary bike can provide low-impact movement to improve circulation and knee mobility.
Side-Lying Leg Lifts: Lie on the patient’s side with your legs straight. Lift your top leg a few inches off the ground and lower it back down. This side lying leg lift exercise targets the hip abductor muscles.
Wall Sit: Lean against a wall and slide down into a seated position with your knees bent at a 90-degree angle. Hold the position for a set amount of time before standing back up.
Hip Hikes: Stand on one leg and lift the opposite hip upward. Lower it back down and repeat. This hip hike exercise helps strengthen the muscles around the hip.
Active Knee Extension: Sit on the edge of a table or a high surface with your legs hanging down. Gently straighten and extend your knees, then lower them back down.
Isometric Hip Adduction: Place a small ball or pillow between your knees while seated. Squeeze your knees together and hold for a few seconds before releasing.
Toe Taps: Sit on a chair with your feet on the floor. Alternate tapping your toes on the ground in front of you, one foot at a time.
Seated Heel Raises: Sit in a chair and lift your heels off the ground, keeping the balls of your feet on the floor. Lower your heels back down.

Side-Lying Hip Abduction with Resistance Band: Lie on your side with a resistance band around your ankles. Lift the patient’s top leg against the resistance of the band.
Resisted Knee Flexion with Resistance Band: Sit on a chair with a resistance band wrapped around your ankle. Bend your knee to lift your foot off the ground against the resistance of the band.
Water Exercises: If you have access to a pool, water exercises like water walking, leg swings, and gentle kicking can provide low-impact movement and support for the joints.
Surgery
Surgery is typically considered for plica syndrome when conservative treatments like rest, physical therapy, and medications have not provided sufficient relief from symptoms, and the condition significantly impairs your daily activities and quality of life.
Surgical intervention for plica syndrome involves removing the irritated or inflamed plica tissue from the knee joint. This procedure is known as a “plica resection” or “plica excision.” Here’s what you should know about plica syndrome surgery:
Plica resection: Plica resection is a surgical procedure used to treat plica syndrome. It involves the removal or trimming of the irritated or inflamed plica, which is a fold of synovial tissue in the knee joint. The surgery is often performed arthroscopically, using a minimally invasive approach with small incisions and a tiny camera (arthroscope) to guide the surgeon’s instruments. During the procedure, the surgeon identifies the problematic plica and then carefully removes or trim it to alleviate irritation and reduce inflammation. This can help improve knee function and alleviate the pain that was caused by the irritated plica.
- Indications: Surgery is generally considered a last resort when non-surgical treatments have been ineffective. Your healthcare provider will assess your case and determine if surgery is appropriate based on the severity of your symptoms and your response to conservative treatments.
- Procedure: During the surgery, the surgeon will make a small incision near the affected area of the knee and carefully remove the irritated plica tissue. Typically, this operation is carried out with minimally invasive methods.
- Recovery: Recovery time varies, but it often involves a period of rest and rehabilitation. Physical therapy is commonly recommended post-surgery to help regain strength, flexibility, and mobility in the knee.
- Success Rates: Plica syndrome surgery tends to have a good success rate in relieving symptoms. However, like any type of surgery, there are potential risks and complications that the patient’s healthcare provider will discuss with you beforehand.
- Preparation: Before the surgery, the patient’s healthcare provider will provide you with instructions on how to prepare. This might involve fasting before the procedure and making arrangements for transportation and post-operative care.
- Post-Surgery Care: Following surgery, you’ll need to follow your surgeon’s instructions for wound care, pain management, and physical therapy. You may be advised to use crutches for a period of time to avoid putting excessive weight on the operated leg.
- Consultation: If surgery is being considered, it’s important to have an in-depth consultation with a specialist who can explain the procedure, potential risks, expected outcomes, and the recovery process.
Complication
While plica syndrome itself is generally considered a benign condition, complications can arise if the symptoms are not managed properly or if the condition goes untreated. Some potential complications of plica syndrome include:
- Chronic Pain and Discomfort: If plica syndrome is left untreated, chronic pain and discomfort can develop, impacting daily activities and quality of life.
- Knee Instability: Irritation of the plica can lead to sensations of instability or “giving way” in the knee joint, potentially increasing the risk of falls or injuries.
- Secondary Issues: Compensatory movements due to pain can lead to muscle imbalances and altered movement patterns, which might contribute to other musculoskeletal issues over time.
- Inflammation: Persistent irritation of the plica tissue can lead to ongoing inflammation in the knee joint.
- Reduced Range of Motion: Untreated plica syndrome can potentially lead to limited knee joint mobility and difficulty fully extending or bending the knee.
- Functional Limitations: As symptoms worsen, individuals might find it challenging to participate in physical activities, sports, or even everyday tasks.
- Development of Scar Tissue: Chronic inflammation and irritation can result in the formation of scar tissue around the plica, further exacerbating symptoms and limiting joint function.
Prevention
While plica syndrome can sometimes be challenging to prevent entirely, there are steps you can take to reduce your risk of developing the condition or experiencing recurrent episodes:
- Warming up properly is important before performing any physical activity or workouts. Gentle dynamic stretches and movements can help prepare your muscles and joints for the activity.
- Gradual Progression: Start a new fitness regimen or up the ante on the difficulty of your workouts gradually. Avoid sudden spikes in activity that can strain your knee joint.
- Cross-Training: Incorporate a variety of exercises and activities into your routine to avoid overusing the same muscle groups and joints repeatedly.
- Proper Technique: When exercising, ensure you’re using proper form and alignment to avoid placing unnecessary stress on the knee joint.
- Listen to Your Body: Pay attention to any discomfort or ache in the patient’s knees. If you notice unusual sensations, it’s best to address them early rather than pushing through.
- Maintain a Healthy Weight: Excess body weight can place additional stress on the knee joint. Maintaining a healthy weight can reduce the risk of joint strain and irritation.
- Proper Footwear: Choose shoes that provide adequate support and cushioning for your feet and knees, especially during physical activities.
- Stay Hydrated: Proper hydration supports joint health and can help prevent stiffness.
- Balanced Muscles: Incorporate strength training exercises that target all major muscle groups, promoting balanced muscle development and joint stability.
- Flexibility and Mobility: Regular stretching and mobility exercises can help maintain proper joint range of motion and reduce the risk of stiffness.
- Rest and Recovery: Give your body enough time between workouts to heal. Overtraining can increase the risk of injuries, including plica irritation.
- Listen to Professionals: If you’ve had a previous knee injury, or surgery, or are prone to knee issues, work closely with a physiotherapist or healthcare provider to develop a safe exercise plan.
Home Advice
Certainly, here are some home advice and self-care tips to help manage plica syndrome symptoms and support your recovery:
- Rest: Allow your knee sufficient rest, especially when symptoms are flaring up. Avoid activities that worsen your pain.
- Ice: Applying ice to the affected area for about 15-20 minutes several times a day can help reduce inflammation and provide pain relief.
- Elevation: Elevate your leg when resting to help minimize swelling and promote blood circulation.
- Over-the-counter Pain Relief: If approved by your healthcare provider, you can consider using over-the-counter pain relievers (such as ibuprofen or acetaminophen) to manage pain and inflammation.
- Compression: Using a knee compression sleeve or bandage can help support the joint and minimize swelling.
- Gentle Movement: Engage in gentle range-of-motion exercises to prevent stiffness. Avoid movements that cause aches or discomfort.
- Low-Impact Activities: Choose activities that put less stress on the knee joint, such as swimming or cycling, if approved by your healthcare provider.
- Shoe Selection: Opt for shoes with good arch support and cushioning to reduce impact on your knees.
- Proper Footwear: Avoid high heels and shoes with inadequate support, as they can contribute to poor knee alignment.
- Healthy Diet: Consume a balanced diet rich in nutrients to support overall joint health.
- Hydration: Drink plenty of water to keep your body well-hydrated and support joint function.
- Weight Management: If necessary, maintain a healthy weight to reduce excess stress on the knee joint.
- Posture Awareness: Maintain good posture to distribute weight evenly and prevent unnecessary strain on the knees.
- Supportive Seating: Use a cushion or support under your knees when sitting for extended periods.
- Orthopedic Supports: Consider using orthopedic pillows or cushions to support your knee while sleeping.
- Pain Diary: Keep a journal of your symptoms and activities to identify triggers and patterns that exacerbate or alleviate your symptoms.
- Stress Reduction: Practicing relaxation techniques, such as deep breathing and meditation, can help manage pain and stress.
- Gradual Return to Activity: As your symptoms improve, gradually reintroduce activities, exercises, and movements while paying attention to how your knee responds.
FAQ
Plica syndrome is a condition where the plica, a fold of synovial tissue within the knee joint, becomes irritated or inflamed, leading to symptoms such as knee pain, swelling, and clicking sensations.
Plica syndrome is often caused by overuse or repetitive knee movements, such as bending, squatting, or kneeling. Previous knee injuries, surgeries, or anatomical factors can also contribute.
Common symptoms include knee pain, swelling, clicking or catching sensations during movement,
stiffness, and occasionally limited range of motion
Diagnosis involves a combination of medical history, physical examination, and sometimes imaging studies like X-rays or MRI scans. In some cases, diagnostic injections may also be used to confirm the diagnosis
Treatment options include rest, physical therapy, anti-inflammatory medications, ice, and in some cases, corticosteroid injections. Surgical intervention might be considered if conservative treatments are ineffective.
Complications can include chronic pain, knee instability, altered movement patterns, inflammation, reduced range of motion, and functional limitations.
At home, you can rest, apply ice, elevate your leg, use over-the-counter pain relievers (if approved), practice gentle movements, choose proper footwear, and maintain a healthy weight.
Complications can include chronic pain, knee instability, altered movement patterns, inflammation, reduced range of motion, and functional limitations.