Chronic Pain
Table of Contents
Definition
Chronic pain refers to persistent discomfort or pain that lasts for an extended period of time, typically beyond the expected healing period of time. It often lasts for three to six months or more and can result from various medical conditions or injuries. Unlike acute pain, which is a short-term response to injury, chronic pain can be more complex and may require long-term management and treatment.
Type Of Chronic Pain
Neuropathic Pain: Caused by damage or dysfunction of the nervous system, often described as shooting, burning, or tingling sensations.
Musculoskeletal Pain: Arises from the muscles, bones, ligaments, and tendons, often felt as aching, stiffness, or soreness.
Inflammatory Pain: This results from inflammation in the body, causing pain, swelling, and heat, as seen in conditions like arthritis.
Visceral Pain: Originates from internal organs and can be vague and deep, often associated with conditions like irritable bowel syndrome.
Mechanical Pain: Triggered by movement or activity, like joint pain or pain due to poor posture.
Central Pain Syndrome: A result of damage to the central nervous system, leading to persistent pain sensations.
Mixed Pain Syndrome: Involves a combination of different pain types and is often more complex to treat.
Classification Of Chronic Pain
Chronic pain is often classified based on its underlying causes and characteristics. Here are some common classifications of chronic pain:
Nociceptive Pain: Caused by activation of pain receptors (nociceptors) due to tissue damage or injury. It could be further divided into 2 subdivisions:
Somatic Nociceptive Pain: Arises from skin, muscles, bones, or joints. Examples include arthritis and musculoskeletal pain.
Visceral Nociceptive Pain: Originates from internal organs. Conditions like irritable bowel syndrome and endometriosis can lead to this type of pain.
Neuropathic Pain: Occurs due to damage or dysfunction of the nervous system. It is often described as burning, shooting, or electric shock-like sensations. Examples include diabetic neuropathy and post-herpetic neuralgia.
Mixed Pain Syndrome: Involves a combination of nociceptive and neuropathic components. Fibromyalgia is an example of a condition that can manifest as mixed pain.
Inflammatory Pain: Results from inflammation in the body, often seen in conditions like rheumatoid arthritis.
Central Sensitization Pain: Occurs when the central nervous system becomes overly sensitive to pain signals, amplifying pain sensations. Conditions like complex regional pain syndrome (CRPS) can involve central sensitization.
Psychogenic Pain: Arises from psychological factors, such as depression, anxiety, or somatization disorders.
Idiopathic Pain: Pain with an unknown or unclear cause.
Cancer Pain: Chronic pain associated with cancer, often due to tumor growth or treatment side effects.
Post-surgical Pain: Pain that persists after a surgical procedure, sometimes referred to as postoperative chronic pain.
Post-traumatic Pain: Chronic pain that develops following a traumatic injury or accident
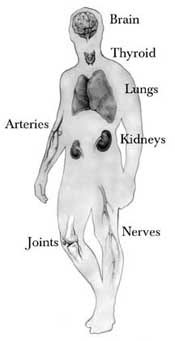
Causes Of Chronic Pain
Chronic pain could have a variety of causes, including:
Injury or Trauma: Previous injuries, surgeries, or trauma can lead to ongoing pain even after the initial healing.
Medical Conditions: Conditions like arthritis, fibromyalgia, multiple sclerosis, and neuropathy can result in chronic pain.
Nerve Damage: Nerve damage or dysfunction, such as in the case of diabetic neuropathy or post-herpetic neuralgia, can cause persistent pain.
Inflammation: Conditions with chronic inflammation, like rheumatoid arthritis or inflammatory bowel disease, can lead to ongoing pain.
Musculoskeletal Issues: Problems with muscles, bones, or joints can result in chronic pain, such as in the case of back pain or osteoarthritis.
Chronic Illnesses: Certain chronic illnesses like cancer or HIV can cause ongoing pain as a symptom of the disease or its treatment.
Psychological Factors: Mental health conditions like depression, anxiety, or stress can contribute to or amplify chronic pain.
Unknown Causes: In some cases, the exact cause of chronic pain may not be easily identifiable.
Managing chronic pain often requires a multidisciplinary approach, involving medical, physical, psychological, and lifestyle interventions. It’s important to work with healthcare professionals to identify the underlying cause and develop an effective pain management plan.
Symptoms of Chronic Pain
Symptoms of chronic pain can vary widely depending on the underlying cause and the individual’s experience, but they often include:
Persistent Pain: Pain that lasts for weeks, months, or even years.
Dull or Aching Pain: Often described as a constant, dull, or aching sensation.
Shooting or Burning Sensations: Some people experience sharp, shooting, or burning pain.
Sensitivity to Touch: Increased sensitivity to touch or pressure on the affected area.
Stiffness: Muscles or joints may feel stiff and difficult to move.
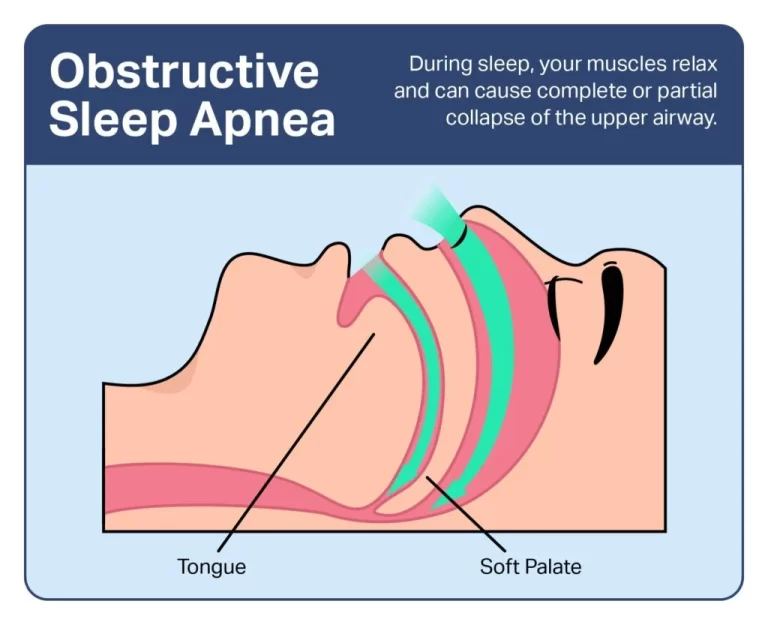
Fatigue: Chronic pain can lead to fatigue and low energy levels.
Sleep Disturbances: Pain can interfere with sleep patterns, leading to insomnia or poor sleep quality.
Mood Changes: Chronic pain can impact mood, leading to irritability, anxiety, or depression.
Decreased Mobility: Difficulty moving or performing everyday activities due to pain.
Limited Functionality: Reduced ability to perform tasks or engage in physical activities.
Weakness: Muscles around the painful area might weaken over time.
Cognitive Effects: Concentration difficulties and cognitive changes, often referred to as “brain fog.”
It’s important to note that chronic pain can affect various aspects of a person’s life and well-being. If you or someone you know is experiencing chronic pain, it’s advisable to seek medical advice for proper evaluation and management.
Diagnosis Of Chronic Pain
Diagnosing chronic pain involves a comprehensive evaluation by healthcare Doctors. The process may include:
Medical History: A detailed discussion about your symptoms, medical history, and any previous injuries or conditions.
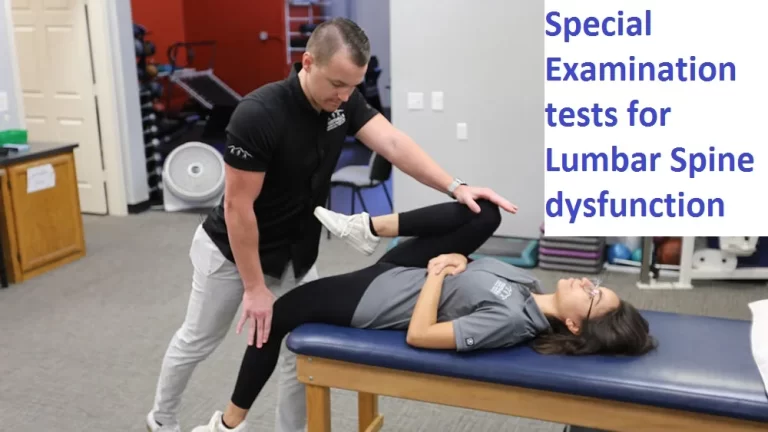
Physical Examination: A physical examination to assess the affected area and identify any signs of inflammation or other abnormalities.
Imaging Tests: X-rays, MRIs, CT scans, or other imaging tests may be conducted to visualize the affected area and detect any structural issues.
Laboratory Tests: Blood tests or other laboratory tests may be done to rule out certain underlying medical conditions.
Pain Assessment: Healthcare providers may use pain scales or questionnaires to understand the nature, severity, and impact of your pain.
Diagnostic Injections: In some cases, diagnostic injections (such as nerve blocks) may be used to help identify the source of pain.
Consultations: You might be referred to specialists such as orthopedists, neurologists, rheumatologists, or pain management experts for further evaluation.
Psychological Assessment: Since psychological factors can influence chronic pain, a psychological assessment may also be conducted.
Medical Imaging: Techniques like MRI or CT scans can provide detailed images of the affected area, helping to pinpoint potential causes of pain.
It’s important to communicate openly with your healthcare provider about your symptoms and concerns, as an accurate diagnosis is essential for developing an effective treatment plan
Medical Treatment For Chronic Pain
Medical treatment for chronic pain can vary based on the underlying cause and individual circumstances. Here are some common approaches:
Medications: Over-the-counter pain relievers (like acetaminophen, ibuprofen) or prescription medications (such as opioids, muscle relaxants, or nerve pain medications) may be used to manage pain. However, opioids are usually reserved for severe cases and closely monitored due to their potential for addiction.
Physical Therapy: Physical therapists can design exercises and techniques to improve mobility, strength, and flexibility, which can help alleviate pain.
Injections: Corticosteroid or nerve-blocking injections can provide temporary relief by reducing inflammation or blocking pain signals.
Surgery: In some cases, surgery may be considered to address the underlying cause of chronic pain, such as repairing damaged tissue or correcting structural issues.
Implantable Devices: Devices like spinal cord stimulators or intrathecal pumps may be implanted to manage chronic pain by altering pain signals.
Acupuncture: This alternative therapy involves inserting thin needles into specific points on the body to stimulate healing and alleviate pain.
Chiropractic Care: Chiropractors use manual adjustments and other techniques to improve musculoskeletal alignment and reduce pain.
Psychological Therapies: Techniques like cognitive-behavioral therapy (CBT) can help manage the emotional and psychological aspects of chronic pain.
Complementary and Alternative Therapies: These might include massage, yoga, meditation, and relaxation techniques to help manage pain and improve well-being.
Multidisciplinary Pain Programs: These programs offer a combination of medical, physical, psychological, and lifestyle interventions for comprehensive pain management.
FAQ
How do people deal with chronic pain?
Tips for dealing with chronic pain
Eating well, getting plenty of sleep, and being physically active are all positive ways to manage stress and pain. Talk to yourself constructively. Positive thinking is a powerful tool.Can I live a normal life with chronic pain?
The picture of pain: What life is really like with chronic pain… Regardless of its source, chronic pain can interfere with almost every aspect of a person’s life—in addition to physical pain, it can interfere with their ability to work and participate. . in social and other activities as before, affect their relationships, and lead to feelings of isolation, frustration, and anxiety
Can chronic pain go away?
Pain is not always treatable. Medical professionals don’t have all the answers, and they don’t always have a cure. There is no magic pill or intervention that will make chronic pain go away. Unfortunately, many people with chronic pain might never be pain-free.
How does chronic pain affect mental health?
People with chronic pain are at greater risk for mental health problems, including depression, anxiety, and substance use disorders. Chronic pain can affect sleep, increase stress and contribute to depression. About 35-45% of people with chronic pain suffer from depression





12 Comments