Meralgia Paresthetica
Table of Contents
What is a Meralgia Paresthetica?
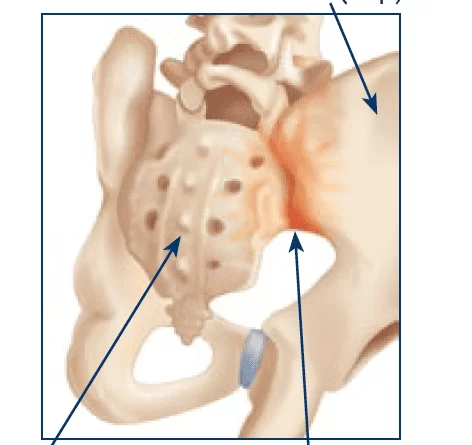
Meralgia paresthetica disease is a condition characterized by tingling, numbness, or burning pain in the outer thigh area. It occurs when the lateral femoral cutaneous nerve, which provides sensation to the thigh area, is pinched or irritated.
Causes of Meralgia Paresthetica
- Tight Clothing: Wearing tight belts, waistbands, or clothing that constricts the area can compress the nerve.
- Obesity: Excess weight can put pressure on the nerve as it passes through the pelvic region.
- Pregnancy: The increased pressure on the pelvic area during pregnancy can lead to nerve compression.
- Injury: Direct trauma or injury to the hip area can damage the nerve.
- Diabetes: People with diabetes may be more susceptible to nerve-related issues, including meralgia paresthetica.
- Weight Gain: Rapid weight gain or changes in body composition can contribute to nerve compression.
- Surgery: Certain surgical procedures in the hip or abdominal area can lead to nerve compression.
- Tumor or Mass: Rarely, a tumor or mass in the pelvic region can compress the nerve.
- Spinal Conditions: Conditions affecting the spine, such as herniated discs or spinal stenosis, may indirectly affect nerve function.
- Nerve Disorders: Other nerve-related conditions or disorders can increase the likelihood of developing meralgia paresthetica.
- Herniated Disc: A herniated disc occurs when the soft tissue between spinal vertebrae pushes out and irritates nearby nerves. This can lead to tingling, numbness, and pain in the buttocks and legs, similar to meralgia paresthetica.
- Peripheral Neuropathy: Peripheral neuropathy is a general term for nerve damage that can cause various symptoms, including tingling, numbness, and pain in different areas of the body, including the legs.
- Lumbar Spinal Stenosis: This is a narrowing of the spinal canal in the lower back area that can compress the spinal nerves. It can lead to similar symptoms as meralgia paresthetica.
- Diabetic Neuropathy: People with diabetes may develop nerve damage due to high blood sugar levels. This can result in similar symptoms to meralgia paresthetica.
- Iliotibial Band Syndrome: This is a common overuse injury that can cause pain and discomfort on the outer side of the thigh. It may have symptoms similar to meralgia paresthetica.
- Femoral Neuropathy: This condition involves damage or compression of the femoral nerve, which can lead to symptoms in the front of the thigh.
- Nerve Entrapment Syndromes: Various nerve entrapment syndromes, such as piriformis syndrome or tarsal tunnel syndrome, could also be considered
Symptoms of Meralgia Paresthetica
- Tingling or Numbness: You may experience tingling or numbness in the outer thigh, typically on one side of the body.
- Burning Sensation: A burning or stinging pain may be felt in the outer thigh.
- Sensitivity: The affected area might become more sensitive to touch or pressure.
- Pain: Pain can range from mild to severe and may worsen with certain activities or movements.
- Discomfort: You may feel discomfort or a sensation of pins and needles in the thigh.
- Worsening Symptoms: Symptoms might worsen after prolonged periods of standing, walking, or other activities that put pressure on the nerve.
- Relief with Rest: Symptoms might improve when you’re resting or lying down.
Diagnosis of Meralgia Paresthetica
- Medical History: Your doctor will ask about your symptoms when they started, any potential contributing factors (such as recent weight gain or tight clothing), and your medical history.
- Physical Examination: The doctor will perform a physical examination, focusing on the affected thigh and pelvic area. They may test for sensation, reflexes, and muscle strength.
- Tinel’s Sign Test: This involves gently tapping or pressing on the lateral femoral cutaneous nerve. If this elicits tingling or other abnormal sensations in the outer thigh, it could indicate meralgia paresthetica.
- Imaging: In some cases, imaging tests like ultrasound, MRI, or X-rays may be ordered to rule out other potential causes of your symptoms.
- Nerve Conduction Studies (NCS) and Electromyography (EMG): These tests measure the electrical activity of the nerves and muscles. They can help determine if there’s any nerve damage or compression.
- Blood Tests: Blood tests may be done to check for underlying medical conditions, such as diabetes, that could contribute to nerve issues.
Medical Treatment
- Pain Relievers: Over-the-counter pain relievers like ibuprofen or naproxen can help manage pain and inflammation.
- Topical Medications: Creams or patches containing lidocaine or capsaicin can provide localized decreased pain.
- Corticosteroid Injections: Corticosteroid injections can help reduce inflammation and alleviate symptoms.
- Rest and Activity Modification: Avoid activities that worsen symptoms and try to minimize pressure on the affected area.
- Weight Loss: If obesity is a contributing factor, losing weight can help relieve pressure on the nerve.
- Loose Clothing: Wearing loose-fitting clothing can reduce compression on the nerve.
- Physical Therapy: A physical therapist can provide exercises to improve posture, strengthen surrounding muscles, and alleviate nerve compression.
- Nerve Blocks: In some cases, a doctor may administer a nerve block injection containing a local anesthetic to temporarily relieve pain and reduce nerve irritation.
- Surgical Interventions: Surgery is rarely needed, but it may be considered if conservative treatments are ineffective and severe symptoms persist. Surgical options might involve decompressing the nerve or releasing tight structures.
Physiotherapy Treatment
- Posture Correction: A physiotherapist can assess your posture and provide exercises to improve alignment, reducing pressure on the affected nerve.
Stretching and Strengthening Exercises:
- Stretching tight muscles: Gentle stretches for muscles that may contribute to nerve compression, such as the hip flexors and iliotibial band.
- Strengthening exercises: Targeting muscles around the hip and thigh to improve stability and support the affected area.
- Soft tissue mobilization: Techniques like massage or myofascial release to address muscle tightness and improve blood flow.
- Joint mobilization: Gentle movements to improve joint mobility and alleviate nerve compression.
- Nerve Gliding Exercises: These exercises aim to improve nerve mobility and reduce irritation by gently moving and gliding the affected nervActivity Modification: Your physiotherapist can guide you in modifying activities to avoid exacerbating symptoms while promoting healing.
- Core Strengthening: Strengthening the core muscles can improve overall stability and posture, which may alleviate pressure on the affected nerve.
- Education: Learning proper body mechanics and techniques to avoid exacerbating symptoms during daily activities.
- Modalities: In some cases, physiotherapists may use modalities such as ultrasound, electrical stimulation, or cold therapy to reduce pain and inflammation.
Exercise
Hip Flexor Stretch:

- Kneel on one knee and lunge forward position, keeping your back straight.
- Gently push your hips forward until you feel a hip flexor muscle stretch in the front of your hip.
- Hold for 20-30 seconds on each side.
IT Band Stretch:
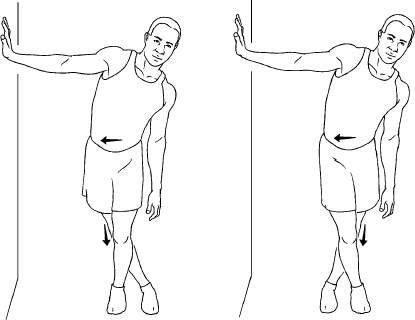
- Cross one leg over the other and lean to the side, stretching the outer thigh.
- Hold for 20-30 seconds on each side.
Piriformis Stretch:
- Lie on the patient’s back and cross one ankle over the opposite knee.
- normally pull the uncrossed knee toward your chest side, feeling a stretch in the buttock area.
- Hold for 20-30 seconds on each side.
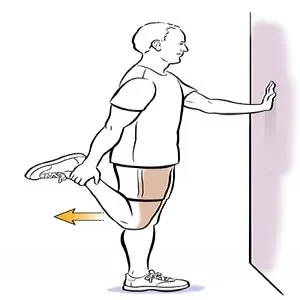
- Stand near a wall area or chair for support.
- Hold onto the wall or chair with one hand.
- Bend your knee and grasp your ankle behind you with the hand on the same side.
- Gently pull your ankle toward your buttocks to stretch the front of your thigh.
- Hold for 20-30 seconds on each leg, repeating a few times.

- Sit on the ground with one leg extended and the other leg bent so the sole of your foot is against your inner thigh.
- Reach forward toward your extended foot area, keeping your back straight.
- Feel the muscle stretch in the back of your thigh.
- Hold for 20-30 seconds on each leg, repeating 3 to 4 times.
Glute Bridge:

- Lie on the patient’s back with knees bent and feet flat on the floor.
- Lift your hip joint off the ground, squeezing your glutes muscle, and hold for a few seconds.
- Lower back down and repeat for ten-15 repetitions.
Wall Sitting:
- Stand against a wall area with your back flat against it.
- Slowly slide down the wall until the patient’s knees are bent at a 90-degree angle.
- Hold this position for 20-30 seconds, gradually increasing the time duration.
Clamshell Exercise:
- Lie on the patient’s side with your legs bent at a 90-degree angle.
- Place your feet together and extend your top knee as far as you can while staying comfortable.
- Lower back down and repeat for ten-15 repetitions on each side.
Hip Hinge Stretch:
- Standing position with patient’s feet shoulder-width apart.
- Place your hands on your hips and hinge at your hips, pushing your buttocks back.
- Keep your back straight and feel the muscle stretch in your hamstrings.
- Hold for 20-30 seconds, repeating a few times.
Nerve Gliding Exercise:
- Sit or stand comfortably.
- Gently extend your leg straight out, then flex your foot back toward your shin.
- Repeat this movement, ensuring it’s pain-free, for about 10 repetitions.
Foam Rolling:
- Gently roll a foam roller over your outer thigh area to help release tension in the muscles and improve circulation.
Core Strengthening:
- Plank exercises, bird dogs, and gentle Pilates exercises can help strengthen your core muscles, improving overall stability.
Bird Dog

Bird dog engages both abs and back muscles, making it an ideal core-strengthening move. It also challenges coordination, balance, and stability.
- Start on all fours, hands under shoulders joint and knees joint under hips. Tighten your core. Lift and extend your right leg to hip level. Simultaneously raise and extend your left arm to shoulder level, palm down. As you extend your arm and leg, maintain a neutral spine without arching your back. cancel Repeat with the left leg and right arm. Start with one session of 8-12 reps.
Bicycle crunch

This variation of the standard crunch works on the obliques, flat stomach, and hips.
- Start with your back on the floor with your left knee bent and pulled toward your chest. Keep your right leg straight and slightly off the floor. Place your hands behind the back of your head or the bottom of your head – be careful not to pull your neck when making this move.
- With your left knee flexed and your right leg straight, lift your right shoulder off the ground and bring your right elbow to your left knee joint. As you bring your right shoulder back to the floor, extend your left leg as you bend your right knee and bring it to your chest. As your right knee moves deeper, lift your left shoulder off the floor and move your left elbow toward your right knee. Start with 3 sets of 12 alternating repetitions.
Plank

The plank exercise is a full-body exercise that targets the core muscle. It also strengthens the arms, shoulders area, back area, buttocks, and legs.
- Start on all fours with the patient’s hands on your shoulders and the knee area under your hips. Extend your legs behind you, keeping your feet wide apart. Tighten your core. Hold for 10-30 seconds. Repeat 3-5 times. To make this exercise easier, keep your knees on the floor, and weights on your hands. Keep a straight line from your knee joint to your shoulders.
Bird dog with elbow-to-knee
This variation of the basic bird dog includes smooth movements to activate the abdominals and back while improving core movements.
- Start on all fours, hands under shoulders, and knee joint under hip area. Tighten your core. Lift and extend your right leg to hip level. Simultaneously raise and extend your left arm to shoulder level, palm down. Bring your right knee joint and left elbow toward each other. Return to the starting position. Start with 1 set of 8-12 reps. Repeat on the other side.
Crunch

Crunches are a classic core-strengthening movement. When lifting the upper body, the abdominal muscles work. If you have occasional lower back area pain, do crunches with care – go slow and start with a few reps.
- Bend your knees and place your feet hip-width apart on the floor. Align your head and back. Cross your arms over your chest. Tighten the heart and relax the neck and shoulders. Tuck your chin in and lift your upper back while keeping your lower back, hips, and feet on the floor. cancel Slowly lower your upper back to return to the starting position. Start with 1 session of 8-12 reps.
Supine toe tap
This is a basic Pilates exercise. It contracts your core muscles, glutes, hips, and legs.
The toes also put pressure on the spine. If you have back pain, foot tapping can be the perfect alternative to crunches.
- Start at the back. Raise your legs so that your knees are at a 90-degree angle. Place the patient’s arms at your sides, palms down. Tighten your core. Lower your right leg and gently tap the floor, keeping your left leg in place and your back straight. Raise your right leg to return to the back position. Repeat with the left leg. Start with 1 session of 8-12 reps.
SUPERMAN PUll
MUSCLES WORK
Erector spinae
glutes
Hamstrings
Latissimus dorsi
Shoulders
Core muscles
- Lie on your stomach with your legs straight and your arms above your head. Lift your arms and legs off the ground and brace your back and glutes. Pull your elbows back and down in a W shape to activate your back and shoulder muscles. Return to the starting position in reverse order. 20 repetitions and Rest 20 seconds between sessions.
The Leg Raises
MUSCLES WORK
Transverse abdominal muscle
Rectus abdominis
Hip flexors
obliques
- Lying on your back, start with your legs in the air (90 degrees) and your feet together. Your arms will remain flat at your sides. Keep your chin up, Core dedicated and strong, and Stay on level ground. You should not put your hand behind your back, Slowly lower your legs off the floor, Return to the starting position,20 repetitions in a set, and Rest 20 seconds between sets.
- Low-Impact Cardio: Engage in activities like swimming stationary cycling or walking to maintain cardiovascular fitness without putting excessive muscle strain on the affected area.
- Home Exercise Program: Your physiotherapist will likely provide you with a personalized home exercise program to continue your progress between sessions.
- Progress Monitoring: Regular follow-up appointments to assess your progress, make adjustments to the treatment plan, and ensure you’re achieving your goals.
Surgery
Surgery is rarely needed, but it may be considered if conservative treatments are ineffective and severe symptoms persist. Surgical options might involve decompressing the nerve or releasing tight structures.
Nerve Decompression Surgery:
- In this procedure, the surgeon releases pressure on the lateral femoral cutaneous nerve by cutting or releasing any tight structures that might be compressing the nerve. This could involve removing a portion of the inguinal ligament (a ligament in the groin area) or other structures that are impinging on the nerve.
Nerve Relocation Surgery:
- In some cases, the nerve might be relocated to a different area where it is less likely to be compressed. This can involve tunneling the nerve through a new path to reduce irritation.
Prevention
- Avoid Tight Clothing: Wearing loose-fitting clothing can help reduce pressure on the lateral femoral cutaneous nerve.
- Weight Management: Maintaining a healthy weight can reduce the risk of excessive pressure on the nerve, especially in the abdominal and hip areas.
- Posture Correction: Improving your posture can help relieve pressure on the nerve. Avoid sitting or standing for prolonged periods in ways that compress the nerve.
- Exercise: Engage in regular physical activity to strengthen core muscles and maintain a healthy weight. However, be cautious with exercises that involve repetitive hip movements.
- Avoid Tight Belts: If you wear belts, avoid tightening them excessively, especially around the waist.
- Cushioned Seats: Use cushions or padding when sitting on hard surfaces to reduce pressure on the outer thigh.
- Healthy Lifestyle: Conditions like obesity and diabetes can contribute to nerve compression. Managing these conditions through a healthy diet and lifestyle can help prevent meralgia paresthetica.
Home Advice
- Wear Comfortable Clothing: Opt for loose-fitting clothing that doesn’t constrict the waist or hip area. This can help decrease pressure on the affected nerve.
- Posture Awareness: Maintain good posture when sitting, standing, and walking. Avoid prolonged positions that might compress the nerve.
- Cushioned Seats: Use cushions or padded seats when sitting on hard surfaces to reduce pressure on the outer thigh.
- Weight Management: If you’re overweight, consider working towards a healthy weight to reduce pressure on the nerve.
- Regular Movement: Avoid staying in one position for too time long. Take breaks to stand, stretch muscle, or walk around, especially if you have a sedentary job.
- Gentle Stretching: Incorporate gentle stretches into your routine, focusing on the muscles around the hips and thighs. However, avoid aggressive stretching that might worsen symptoms.
- Low-Impact Exercise: Engage in low-impact exercises that don’t put excessive strain on the affected area, such as swimming, stationary biking, or gentle walking.
- Ice or Heat: Applying ice or heat to the affected area might help alleviate discomfort. Experiment with both to see which provides better relief.
- Pain Relief Measures: Over-the-counter pain medications (under medical guidance) or topical pain creams might provide temporary relief.
- Elevate Legs: Elevating your legs slightly when lying down can help reduce pressure on the nerve.
- Avoid Tight Belts: If you wear belts, avoid tightening them excessively around the waist.
- Avoid High Heels: Wearing high heels can alter your posture and put additional strain on the hips and thighs.
- Stay Hydrated: Proper hydration can support overall nerve health and reduce the risk of muscle cramps.
- Stress Reduction: Stress can exacerbate certain nerve-related conditions. Engage in relaxation methods like deep breathing, meditation, or yoga.
FAQ
Tight Clothing: Wearing tight belts, waistbands, or clothing that constricts the area can compress the nerve.
Obesity: Excess weight can put pressure on the nerve as it passes through the pelvic region.
Pregnancy: The increased pressure on the pelvic area during pregnancy can lead to nerve compression.
Injury: Direct trauma or injury to the hip area can damage the nerve.
Diabetes: People with diabetes may be more susceptible to nerve-related issues, including meralgia paresthetica.
Weight Gain: Rapid weight gain or changes in body composition can contribute to nerve compression.
Take heat, ice, or over-the-counter pain relievers such as aspirin, acetaminophen, naproxen, or ibuprofen for a few days. Weight loss. Wear loose clothing, especially in the upper part of the hips.
Wear looser clothing. Lose excess weight. Taking medicine for pain relievers such as acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others), or aspirin.
Tingling and numbness. Burning pain. Decreased sensation. Increased sensitivity and pain even to light touch.
Avoid Tight Clothing:* Wearing loose-fitting clothing can help reduce pressure on the lateral femoral cutaneous nerve.
Weight Management: Maintaining a healthy weight can reduce the risk of excessive pressure on the nerve, especially in the abdominal and hip areas.
Posture Correction: Improving your posture can help relieve pressure on the nerve. Avoid sitting or standing for prolonged periods in ways that compress the nerve.
Exercise: Engage in regular physical activity to strengthen core muscles and maintain a healthy weight. However, be cautious with exercises that involve repetitive hip movements



One Comment