Multiple Sclerosis (MS)
Table of Contents
What is multiple sclerosis?
Multiple sclerosis is an autoimmune disease of the nervous system characterized by inflammation, selective demyelination, and gliosis. Multiple sclerosis is a chronic disease that affects mostly the central nervous system, which is the brain, spinal cord, or optic nerves. it can lead to a wide range of symptoms throughout the body.
- The most widely accepted theory is that MS is an autoimmune disease induced by a viral or another infectious agent. Herpes and chlamydial pneumonia virus are infectious agents.
- The presence of increased immunoglobulin (in G) and in CSF of M.S patients provides evidence of precipitating infection eliciting an autoimmune response resulting in pathological changes. Viral infection precipitates relapse in M.S.
What are the causes of Multiple sclerosis?
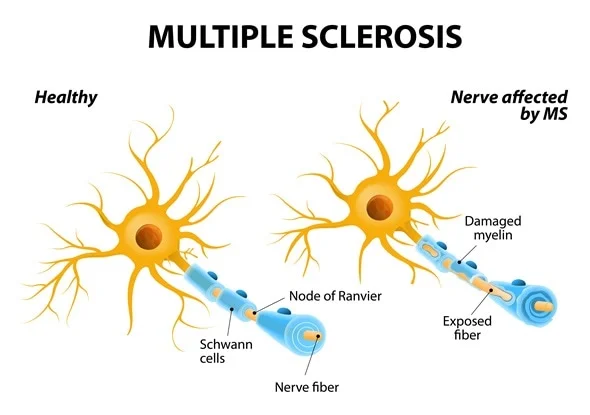
- The causes of multiple sclerosis are unknown. It is considered an autoimmune disease also in which the body’s immune system attacks its own tissues. In the cases of MS, this immune system malfunction destroys the fatty substance that coats or protects nerve fibers in the brain or spinal cord (myelin) and mostly Myelin can be compared to the insulation coating on the electrical wires.
- When the protective myelin is damaged or the nerve fiber is exposed, the messages that travel along that nerve fiber may be slowed or blocked. It isn’t clear why MS develops in many people and not others. A combination of genetics or environmental factors appears to be responsible.
Pathophysiology:
- In patients with M.S., the immune response triggers the production of t-lymphocytes, macrophages, and immunoglobulins(antibodies), which produce an autoimmune cytotoxic effect within the CNS. The blood-brain barrier fails and myelin-sensitized t-lymphocyte cells enter and attack the myelin sheath that surrounds the nerve.
- Myelin serves as an insulator, speeding up the conduction along the nerve fibers from one node of Ranvier to another(saltatory conduction). It also serves to conserve energy for the nerve because mainly depolarization occurs only at the nodes. Disruption of myelin sheath produces active demyelination, slowing neural transmission, and causing the nerves to fatigue With severe disruption, conduction block occurs with resulting disruption of the function. Local inflammation, edema, and infiltrates surround the acute lesion and can cause a mass effect, further interfering with the conductivity of nerve fibers.
- This inflammation gradually subsides which accounts for the pattern of fluctuations in the function that characterize this disease. During the early stages of MS, oligodendrocytes survive initial insult and can produce remyelination. This process is often incomplete and as the disease becomes chronic, stalls altogether. the oligodendrocytes become involved and myelin repair can not occur. Demyelinated areas eventually become filled with fibrous astrocytes or undergo a process also called gliosis.
- Gliosis refers to the proliferation of neuroglial tissue within the CNS or results in glial scars(plaques). this stage, the axon itself becomes mainly interrupted and undergoes retrograde degeneration. Axonal loss varies from 10-20% in milder forms of disease to as much as 80% in severe MS.
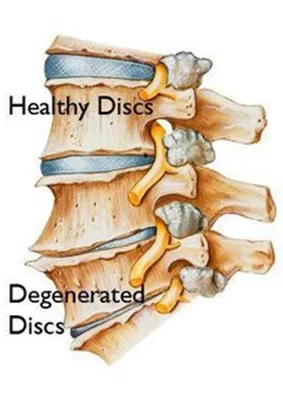
- In advanced cases, there are both acute and chronic lesions of varying sizes scattered throughout the CNS(brainstem, brain, cerebellum, and spinal cord.) They primarily affect the white matter early, with lesions of gray matter evident in more advanced diseases. There are certain areas of predilection such as optic nerves, spinal cord(corticospinal tracts, posterior white columns), and cerebellar peduncles.
Types of Multiple sclerosis:
Relapsing-remitting MS:
- characterized by discrete attacks of neurological deficits(relapse) with either full or partial recovery (remission) in subsequent weeks or months. The period between relapses is characterized by a lack of disease progression. Affects approximately 85% of patients with M.S.
Primary progressive MS:
- Affects 10% of patients with M.S. It is characterized by disease progression and steady functional decline from the onset, patients may experience modest fluctuations in neurological ability.
Secondary progressive MS:
- Characterized by an initial relapsing-remitting course, followed by a change in the clinical course with progression to steady and irreversible decline with or without continued attacks.
Progressive relapsing MS:
- Characterized by a steady deterioration in disease from the onset but with occasional acute attacks. Intervals between attacks are characterized by continuing disease progression and Affect approximately 5% of patients with m.S.
Symptoms of Multiple sclerosis:
- Pain: Headache, chronic neuropathic pain, and paroxysmal limb pain.
- Cognitive symptoms: Short-term memory deficits, diminished executive function, and diminished attention/concentration.
- Affective Symptoms: Depression or anxiety.
- Motor symptoms: spasticity, spasms, ataxia, impaired balance, or gait.
- Speech and swallowing: dysarthria, dysphonia, and dysphagia.
- Bladder/Bowel symptoms: spastic or flaccid bladder, constipation, diarrhea, or incontinence.
- Sexual Symptoms: impotence, decreased libido, decreased ability to achieve orgasm.
- The pattern of symptoms will be different from the person.
Diagnosis of MS:
- MRI: a sensitive tool for confirming disease along with clinical features and CSF analysis. MRI detects both acute and chronic lesions, small and large with high resolution. Gadolinium is the main chemical compound given during MRI. These scans are used to distinguish new lesions with active inflammation that occur during the preceding 6 weeks or so. Lesions are seen as areas of improved signal intensity,” bright spots”.
- T2 scans are used to detect more long-term disease activity These lesions are seen with black holes on MRI, the darker the lesion, the more extensive the tissue damage. Lesions of M.S. are scattered in time or place. Lesions revealed on MRI reports do not always correlate with clinical disability. Current guidelines suggest that MRI should be performed at predefined intervals to document disease progression and response to disease-altering medications.
- Evoked potentials. These test record the brain’s electrical response to visual, auditory, or sensory stimuli. These tests if you have a slowing of messages in the different parts of the brain.
- Cerebral spinal fluid is analyzed. it is also called a spinal tap or lumbar puncture. It looks at the fluid taken from the spinal column to make an evaluation and diagnosis. The test checks for cellular and chemical abnormalities seen with MS.
- Blood tests. These are done to rule out other causes of various neurological symptoms.
What is the complication of Multiple Sclerosis?
- The complication of MS range from mild to severe. this is range from fatigue to the inability to walk. many problems include loss of vision, balance, and bowel or bladder control. Depression can result from the difficulty of living with chronic conditions.
How is Multiple Sclerosis treated?
Sensory deficits and skin care:
- Strategies should be instituted to improve awareness of sensory deficits compensate for sensory loss and promote safety.
Compensatory training strategies:
- E.g: Visual compensation techniques can be instituted when deficits in proprioception produce imbalance and place the patient at risk of fall. Proprioceptive loading through exercise, resistance bands, or weights and the use of a pool may heighten residual proprioceptive function and improve movement awareness.
Skincare:
- The skin should be kept clean and dry. It should be inspected regularly Clothing should be comfortable and breathable, Change of position: every 2 hours in bed and every 15 minutes in a wheelchair. Wheelchair pushups or repositioning maneuvers to relieve pressure.
Other:
- Aquatic exercise programs have a positive effect on people with progressive multiple sclerosis. It promotes general health, increased energy levels, and mental health, and aids social interaction in the presence of a physical disability. Because of the reduced impact of gravity, aquatic training allows patients with even severe paresis of the lower extremities to perform standing or moving exercises. A systematic review or Meta-Analysis recommends combining aquatic therapy with conventional physical.
- Specific balance exercises can increase balance. Poor postural control improves the risk of falls. MS patients have improved sway in quiet stance, delayed postural perturbations, and reduced ability to move towards limits of stability. These impairments are causes of falls. Reduced gait speed, decreased stride length, cadence, or joint movement are observed in most studies of gait in MS therapy for MS patients.
- Motor Imagery is increasing use in neurorehabilitation in order to facilitate motor performance. Motor imagery and rhythmic auditory stimulation can be used for walking rehabilitation in MS patients and Randomized controlled trials studying the effects of motor imagery shows significant improvement in walking speed, walking distance, perception, or quality of living.
- Gait rehabilitation forms a large part of neuro-rehabilitation for people living with MS disease. A systematic review published in Diagnostics describing the gait patterns in people with multiple sclerosis (MS) shows a decrease in speed or stride and step length, an improvement in the step width, no improvement in hip extension during the stance period, a reduction in knee flexion in the swing period, a decrease in ankle dorsiflexion in the initial contact, or a decrease in ankle plantarflexion during the pre-swing phases; thus concluding that rehabilitation should focus on the combating asymmetrical gait characteristics.
For precaution against bed sore development:
- Patients with deficits in superficial sensations, risk damage to insensitive areas of skin.The development of decubitus ulcers major concern with chronic progressive disease. Changes in skin turgor, static posturing, or prolonged pressure over bony prominences increase the likelihood of skin breakdown.
- The patient may not feel the discomfort of prolonged positioning or may be unable to shift position because of weakness or spasticity. Spasticity and spasms may cause friction effects between the skin and supporting surfaces. Awareness, protection, and care of desensitized parts: taught to the patient.
FAQ
The cause of multiple sclerosis is unknown. It is an autoimmune disease where the body’s immune system damage its own tissues. In the case of MS, this is an immune system malfunction that destroys the fatty substance that coats or protects nerve fibers in the brain and spinal cord injury.
fatigue.
numbness or tingling.
loss of balance or dizziness.
stiffness and spasms.
tremor.
pain.
bladder problems.
bowel trouble.
Feelings of shock, denial, fear, anger, anxiety, loneliness, sadness, uncertainty, or guilt are all a normal part of coming to terms with a diagnosis of a lifelong condition like MS. You feel a sense of relief or acceptance, especially if you have spent a long time trying to find out the reason for your symptoms.
Most symptoms develop abruptly, within hours and days. This is attacks or relapses of MS typically reach their peak within a few days at most or then resolve slowly over the next several days and weeks so that a typical relapse will be symptomatic for about eight weeks from the onset to recovery. Resolution is often completed.
MS varies from patient to patient so each individual has their own set of symptoms, problems, or their own course. There are peoples who have MS so mildly that they never even know that they have it.






17 Comments