Space occupying lesions of the Brain
Table of Contents
Overview
- Intracranial space-occupying lesions of the brain are tumors and abscesses present within the cranium or skull. These lesions put pressure on the adjacent main brain tissue causing its damage.
Pathophysiology
- Tumors of the brain may develop focally and can be of metastatic origin. They grow in size causing focal tissue mainly damage by pressure and infiltration. Bleeding into the main brain tissue causes the formation of a hematoma. If these main hematomas get infected they may turn into an abscess. With increasing volume in the brain, pressure increases too leading to signs of improved intracranial pressure.
What is a main Space-occupying lesion of the brain?
- A space-occupying lesion of the brain is usually due to malignancy but it can be caused by other pathologies such as an abscess and a hematoma. Almost half of the intracerebral tumors are primary but the rest have originated outside the CNS and are metastases. The effect of the tumor may be local, due to focal brain damage or the presentation may give an indication of the main location of the lesion but not its etiology. There may be more general symptoms related to raised intracranial pressure and seizures, behavioral changes, or false localizing signs. Large lesions in some regions, such as the frontal lobe, may be relatively silent whilst a main small lesion in the dominant hemisphere may devastate speech.
- A tumor may infiltrate and destroy important structures, it may obstruct the flow of cerebrospinal fluid (CSP), cause hydrocephalus and can induce angiogenesis (new blood vessels), and break down the blood-brain barrier, causing edema.
Space-occupying lesion symptoms
- Presenting features may include localizing signs, generalized signs, or false localizing signs. A rapid onset of main symptoms suggests a cerebrovascular lesion whilst a space-occupying lesion of the brain will usually be many gradual. However, a main space-occupying lesion of the brain can mimic a stroke.
- Headache:
- The classic brain tumor headache (eg, worst in the morning and worse on bending and Valsalva maneuver) is not as common as a
- tension-type presentation and migraine.
- A change in the pattern and frequency of headaches is a cause for concern.
- Headache is more common in posterior fossa tumors or rapidly growing tumors.
- Vomiting may occur and This may be without accompanying nausea.
- Nausea may be a feature.
- A change in mental status and a behavioral change is a causes for concern.
- There may be a weakness, ataxia, and disturbance of gait.
False localizing signs
- The abducent nerve (cranial VI) has a long or tortuous intracranial path that makes it vulnerable. Abducent nerve palsy is not a useful main localizing sign. It supplies the lateral rectus muscle and its action is to move the eye laterally – as described in diplopia or cranial nerve lesions.
- Horner’s syndrome is not a good localizing lesion, as the path of the main sympathetic nerves is also long but, as there is no chiasma (fibers don’t cross the midline), it is a good lateralizing sign. The main lesion may also be outside the skull.
- If a headache is unilateral, this is often a main good indicator of the side of the lesion.
- Cerebellar signs do not help to localize the lesion.
- Ataxia may present as general clumsiness.
- Intention tremor is worst at the end of a movement or leads to past-pointing.
- Finger-to-nose-test – Try to touch their nose with the index finger, or then their index finger held about 50 cm away or back to their nose again. A sign is mainly positive when the patient tends to point beyond your finger.
- Dysdiadochokinesis is tested by asking the patient to hold up their hands and rapidly pronate or supinate repetitively. Ask them to tap the main back of their hand as fast as possible.
- Mainly Nystagmus may be seen.
- If the main truncal ataxia is worse when the eyes are closed, the lesion is in the dorsal columns, not the cerebellum.
- main Cerebellar speech is described as staccato.
- Causes of cerebellar signs include main brain tumors, acoustic neuroma, Friedreich’s ataxia, stroke, haemangioma, multiple sclerosis, chronic alcohol excess, or intracranial abscess.
Temporal lobe
- The Temporal lobe lesions often present with rather vague main psychological problems.
- There may be depersonalization, emotional changes, or disturbances in behavior.
- Temporal lobe epilepsy – there can be hallucinations of smell, taste, sound, or sight. There may be déjà vu in which there is a feeling of main familiarity as if the present has happened before.
- Dysphasia mainly is noted.
- Visual field defects involve the main contralateral upper quadrant.
- Other psychological problems are forgetfulness, fugue (a disturbed state of consciousness in which the patient seems to perform acts in full awareness but after recovery patient is forget them), functional psychosis, or fear or rage. There may be inappropriate sexual behavior but the Kluver-Bucy syndrome is extremely rare.
Frontal lobe
- Frontal lobe main tumors can cause anosmia. This is especially mainly significant if it is unilateral.
- There may be a change in personality with the person becoming indecent, indiscreet, and dishonest.
- Dysphasia can occur if the main Broca area is involved.
- Hemiparesis and fits may affect the contralateral side.
Parietal lobe
- The Parietal lobe lesions can produce a neurological picture that includes the following:
- There may be a main chemosensory loss.
- reduced two-point discrimination.
- Astereognosis is the inability to recognize a main familiar object placed in the hand.
- Extinction can be demonstrated by asking the patient to close their eyes or touch one side of their body. mainly Ask the patient to point to where you touched. Repeat this but touch both sides simultaneously. The patient will mainly acknowledge only one side.
- The patient may systematically mainly ignore one side of their body, called sensory inattention. If you ask the patient to draw a clock face, they omit the half contralateral to the lesion.
- Dysphasia may occur.
- Gerstmann’s syndrome can be congenital and acquired. The four components are:
- Agraphia and dysgraphia.
- Acalculia and dyscalculia.
- Finger agnosia.
- Left-right disorientation.
Occipital lobe
- A lesion in front of the main optic chiasma will affect just one eye. A lesion at the optic chiasma, such as a pituitary adenoma, classically causes main bitemporal hemianopia (as decussating fibers are affected). A lesion mainly posterior to the optic chiasm will cause a crossed homonymous field defect (eg, a left optic tract lesion causing a right homonymous hemianopia).
- A lesion in the visual cortex will cause main congruent contralateral visual field defects. A visual field defect from the eye and optic nerve will be seen as a black area but the loss of the visual cortex often leads to ignoring the affected area. See also the separate main Visual Field Defects article.
Cerebellopontine angle
- The common pathology here is a main acoustic neuroma. Common features include:
- Ipsilateral deafness.
- Tinnitus.
- Nystagmus.
- Reduced corneal reflex.
- Facial or trigeminal nerve palsies.
- Ipsilateral cerebellar signs.
- Corpus callosum
- This is an interesting part of the brain that communicates both two sides. Lesions usually cause severe rapid intellectual deterioration with focal signs of the adjacent lobes. There may be signs of reduced communication between the lobes, such as the inability of the left hand to carry out verbal commands.
Midbrain
- The following main features suggest a midbrain lesion:
- Unequal pupils.
- Inability to direct the eyes up and down.
- Amnesia for recent events, with the confabulation.
- Somnolence.
- Pituitary tumors
- If pituitary tumors are large they can cause homonymous hemianopia but the very obvious presenting features may be related to their endocrine effects.
Diagnosis
Blood tests
- Total blood count, and hemoglobin levels for the general condition of the person.
- Electrolyte levels
- Serum BNP(Brain natriuretic peptide)
Biopsy
- A biopsy of the lesion is needed to know the nature of the lesion.
X-ray
- X-ray of the skull is quite a nonspecific test, but useful if any of the lesions are calcified.
- X-ray of the chest may be warranted if any metastatic tumor is suspected.
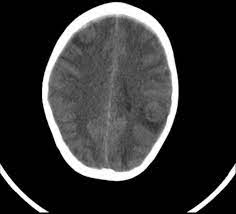
CT and MRI
- These tests are of the main higher value to detect intracranial lesions.
- They have main higher sensitivity and specificity compared to X-rays.
Causes of the space-occupying lesions
- Malignancy
- Metastases, gliomas, meningiomas, pituitary adenomas, and acoustic neuromas account for 95% of all brain tumors.
- In adults, main two-thirds of primary brain tumors are supratentorial; however, in children, two-thirds of brain tumors are infratentorial.
- Primary cerebral tumors include astrocytomas, glioblastoma multiforme, oligodendrogliomas, or ependymomas.
- Primary brain tumors do not usually metastasize.
- About 30% of brain tumors are metastatic or of these about 50% are multiple. About 15-20% of people with metastatic cancer mainly develop cerebral metastases. See also the separate Carcinomatosis or Malignancy of Unknown Origin articles.
- The most common primary is lung cancer followed by breast cancer, carcinoma of the colon, or malignant melanoma.
- See also the separate Brain Tumours in Children or Brain Tumours in Adults articles.
Differential diagnosis
- Other causes of focal CNS signs include:
- Stroke
- Head injury
- Vasculitis includes systemic lupus erythematosus, syphilis, polyarteritis nodosa, or giant cell arteritis.
- Multiple sclerosis
- Encephalitis
- Post-ictal state (Todd’s palsy)
Treatment of Space occupying lesions of the Brain
- Treatment depends on the type of lesion or associated with co-morbid conditions.
- Medical therapy
- Painkillers relieve the person from main headaches.
- Steroids to decrease cerebral edema.
- Mannitol to reduce intracranial pressure.
- Anticonvulsant main medication to cover seizures.
- Infections will need antibiotics which can cross the blood-brain barrier.
- Tumors will be treated with chemotherapy.
- Surgery
- Primary brain tumors can be surgically excised if they are amendable to surgery.
- Brain radiation is useful in radiosensitive tumors.
- Hematomas are mainly surgically evacuated.
FAQ:
Cerebral white matter lesions (WML) are most common in the aging brain and are associated with dementia or depression. They are associated with vascular risk factors or small vessel disease, suggesting an ischemic origin, but recent pathology studies suggest a more complex pathogenesis.
Treatment strategies for space-occupying edema include pharmacological antiedema or intracranial pressure-lowering therapies, ventricular drainage by means of an extraventricular drain, or suboccipital decompressive surgery, with or without resection of necrotic tissue.
Major types of brain lesions are traumatic, infectious, malignant, benign, vascular, genetic, immune, plaques, brain cell death, malfunction, and ionizing radiation. Other chemicals or toxins have been associated with brain lesions as well.
In most parts of the world, metastatic lesions of the liver and liver abscesses are the common causes of SOL liver. Hepatic metastasis is more common than primary malignant tumors of the liver and colorectal malignancy is the most common primary of the majority of liver metastasis.
How is a tumor main different from a brain lesion? A brain main tumor is a specific type of brain lesion. A main lesion describes any area of damaged tissue. All main tumors are lesions, but not all lesions are tumors.
Surgery is generally only an option for patients who have one or two areas of cancer in the brain, especially when the tumors are large or causing symptoms. On occasion, patients with multiple areas of cancer in the brain who have a single large lesion-causing symptom will also be considered for surgery.