Cervical examination
Table of Contents
Introduction
- The primary goal of the Cervical examination is to match a patient’s clinical presentation with the most efficacious treatment approach. The component of the decision is determining whether a patient is, in fact, appropriate for the therapy treatment.
- To perform this there are 3 essential elements of the examination:
- Rule out any pathological severe condition that can need a referral to the medical practitioner for further investigation or even surgical intervention.
- Most commonly identify motion dysfunction, impaired motor control, sensory-motor impairment, as well as related connective & nerve tissue dysfunction & if really possible rule in or even out particular situations.
- Identify other contributing factors that can affect deviations from the expected clinical course of neck pain.
What to do before the investigation?
- Wash the hands
- Introduce yourself
- Identity of the patient, confirm
- Permission (consent & explain examination)
- Pain
- Position sitting in the chair with room behind a chair for an examiner to stand
- Privacy
- Expose neck as well as clavicles (the patient can require to tie hair back/ remove necklace)
- Equipment – have the glass of water on hand.
General Inspection
- Surroundings
- Monitoring
- Treatments
- Paraphernalia
- Patient
Subjective
- Patient Intake
- Taking a detailed patient history is essential. Listen carefully to a patient’s past medical history (PMH) & history of present illness (HPI). The narrative provided by the patient contains much of the information needed to rule out red flags as well as guide a cervical examination.
- When taking the patient’s history this is also essential to ask if they have pain or even symptoms in other regions namely their thoracic spine or even shoulder.
- Outcome measures namely a neck Disability Index or even Patient-Specific Functional Scale can also be used at this stage (See outcome measures section).
Red Flags
Cervical Myelopathy
- Cervical myelopathy is a situation mainly involving compression of the spinal cord at the cervical level of the spinal column which is resulting in spasticity, hyperreflexia, pathological reflexes, digit/hand clumsiness, & gait disturbance.
- A spontaneous course of myelopathy is characterized either by long periods of stable disability followed by episodes of deterioration or the linear progressive approach. The presentation of cervical myelopathy varies according to the spinal cord compression severity.
- Any space-occupying lesion within a cervical spine with the potential to compress a spinal cord may cause cervical myelopathy. Cervical myelopathy is predominantly owing to pressure on an anterior spinal cord with ischemia due to the deformation of a cable by anterior herniated discs, spondylitis bone spurs, the ossified posterior longitudinal ligament, or spinal stenosis.
Signs & Symptoms
- Sensory disturbance of the hands
- Hand-intrinsic muscle wasting
- Unsteady gait
- Hoffman’s reflex
- Babinski
- Clonus
- Inverted supinator sign
- Hyperreflexia
- Bowel and bladder disturbances
- Multisegmental weakness
- Multisegmental sensory changes.
Cervical Instability
Definition
- Clinical instability of a cervical spine (CICS) is mainly defined as an inability of a spine under physiological loads to maintain its normal pattern of displacement so that there is no neurological damage or even irritation, no development of deformity, as well as no incapacitating pain.
- While no tools exist for an assessment of upper cervical ligamentous instability, the approach which takes into account risk factors, a patient history, as well as examination results to make informed decisions about patient management has been recommended.
Sign and symptoms
- Occipital headache & numbness
- Severe limitation while neck active range of movement (AROM) in all directions
- Signs of the cervical myelopathy
- Post-trauma
- Rheumatoid arthritis
- Down Syndrome
Vertebral Artery Insufficiency
Sign & symptom
- Drop attacks
- Dizziness
- Dysphasia
- Dysarthria
- Diplopia
Inflammatory or even Systemic Disease
Sign and symptoms
- Temperature >100 °F
- Blood pressure > 160/95 mmHg
- Resting pulse > 100 bpm
- Resting respiration >25 bpm
- Fatigue
Yellow Flags
- Yellow flags are factors that increase the patient’s risk of developing long-term disability.
- Psychosocial factors can contribute to the patient’s persistent pain and disability, or can contribute to a transition from an acute condition to a chronic, disabling condition.
- Some attitudes, as well as beliefs to look out for, are.
- Pain may be harmful or even disabling
- Pain can be eliminated prior to coming back to activity
- Passive attitudes towards the therapy
- The patient uses extended rest, reduced activity level moreover withdrawal from daily activities
- The patient reports an extreme pain intensity
- High intake of alcohol or even other substances
Investigations
Radiological Considerations
- Cervical spine radiographs are most commonly utilized to assess for fractures; But, a cervical CT- scan is more sensitive for ruling out fractures in the affected part. The patients along with rapidly worsening neurological signs and symptoms can be referred for a cervical MRI.
- Patients with red flags mainly including a history of cancer, possible cervical arterial disease, & possible instability must be referred for diagnostic imaging procedures.
- Positive cranial nerve signs
- AtaxiaNausea
- Constant pain, not relieved with the best rest
- Night pain
Observation
Posture
- Observing the patient’s posture in standing as well as sitting. As part of an examination, postural deviations may be corrected to determine an effect on a patient’s signs & symptoms.
- Common postural deviations:
- Protracted cervical spine or even forward head posture
- Protracted shoulder girdle & rounded shoulders
- Upper Thoracic Spine
- Kyphotic or even Flexed posture
- Lordotic or even Extended posture
- Normal
Palpation
Supine position
- Palpate bilateral sternoclavicular joints for mobility assessment or even tenderness.
- Then, palpate an acromioclavicular joint for mobility assessment or tenderness.
- Palpate suboccipital muscles, upper trapezius muscle, levator scapula muscle as well as pectoralis minor muscle to assess shortness or even tenderness.
Prone position
- Peripheral along with central Cervical and Thoracic Spine
- Palpate the ribs numbers 1 to 7 of the upper and mid thoracic part.
- Ribs 1 to 7 posterior to an anterior accessory action.
Movement Tests
Functional Movement
- Before anything else ask a patient to demonstrate a functional motion that most easily replicates the symptoms.
- The action that the patient demonstrates can give many clues to the main cause of the issue as well as a perfect performance-based outcome measure.
- Active range of motion of the cervical, passive range of motion of the cervical spine as well as overpressure.
- Prior to the action of the cervical spine testing the checker could be questioned a patient regarding baseline symptom location as well as intensity included.
- A doctor who is the chief examiner notes any change in a location or intensity during the testing and the area of problem happened.
- A tester(examiner) may assess for the presence of symptom centralization and peripheralization at the time of testing. Repeated movements can be utilized as a part of the assessment.
- Active, passive all types of cervical range of motion tests (Neck flexion, extension, rotation along with side-bending) performed with the patient in a seated position with upright posture.
- The cervical active or even passive range of motion may be done with the inclinometer instrument. The inclinometer instrument used for cervical range of movement measurements has exhibited reliability coefficients ranging from 0.66 to 0.84 (ICC).
- The universal goniometer is mainly used to find out the range of cervical rotation if measured in a sitting position.
- Passive overpressure could be primarily applied at the end of the active motion to assess for a pain response as well as an end feel.
Combined movements
- Upper cervical flexion with lower cervical extension is commonly assessed with a cervical
- retraction.
- An upper cervical extension motion along with lower cervical extension is most commonly assessed with cervical protraction.
- The cervical quadrant is mainly fixed with the cervical extension along with ipsilateral rotation & side bending.
A special test is done by the physical therapist
Passive osteoarthritis Joint testing (flexion/extension)
- The patient is positioned in the supine with head on or even off the management table
- A physical therapist is in standing at a head of a patient.
- Movement testing (Right OA joint)
- Rotate the head 20 – 30 to the right side to orient a right facet into a sagittal plane.
- The translate occiput anterior on a superior facet of C1 to examine for OA extension restriction
- Translate an occiput posterior to assess for the OA flexion restriction.
- Repeat to the Left side as well.
Mobility Testing (Cervical Rotation in the Flexion)
- Cradle head with both hands
- Contact a posterior aspect of C1 with fingertips
- Flex cervical spine
- Assess the amount of rotation to each side
- Maintain flexion during rotating the cervical spine.

Cranial Cervical Flexion Test
- A patient is in the position supine in a hook lying with a head as well as neck in mid-range neutral. After that, towels can be required under an occiput to achieve the neutral position.
- The pneumatic pressure device, namely the pressure biofeedback unit, is inflated to 20 mmHg to fill a space between a cervical lordotic curve & a surface of a table.
- During maintaining an occiput stationary (not lifting or pushing down it), the patient does the cranial cervical flexion in the graded fashion in 5 increments (22,24,26,28 and 30mmHg) & goal to hold each position for nearly seven to ten seconds. Ten seconds of rest is provided between the two stages.
- CCF is done by a patient gradually nodding a head as though a patient was saying “yes” with an upper neck. The movement may flatten a cervical lordosis & subsequently change the pressure in a pneumatic.
- During a patient’s CCF, a physiotherapist palpates the neck to monitor for unwanted activation of more superficial cervical muscles like sternocleidomastoid.
- A test is graded according to a pressure level a patient may achieve with concentric contractions as well as accurately sustain isometrically.
- A test is terminated when pressure is reduced by more than 20% or when a patient cannot do a proper CCF action without substitution strategies.
- The normal response is for a pressure to increase between 26 – 30 mmHg & be maintained for seven to ten seconds without utilizing superficial cervical muscle substitution strategies.
- The patient should follow the instructions of the physical therapist very carefully.
- The abnormal response is where a patient:
- Is not able to generate an increase in pressure of at least 6 mmHg.
- Is not able to hold a generated pressure for seven to ten seconds.
- Uses superficial neck muscles to accomplish the cranial cervical flexion or
- Uses the sudden motion of a chin or even pushing (extending) a neck forcefully against the pneumatic pressure device.
- ICC = 0.81, performance index ICC = 0.93
Neck Flexor Muscle Endurance Test
- A patient is in the position supine, with a hook lying. A chin is maximally retracted & maintained isometrically during a patient lifts a head as well as neck until a head is approximately 2.5cm (1 in) above a plinth during keeping a head retracted to a chest.
- A physical therapist focuses on skin that folds along with a patient’s neck & places the hand on a table Just below an occipital bone of a patient’s head. A physical therapist provides verbal commands namely “tuck the chin” or “hold the head up” whenever a skin folds start to separate or a patient’s occiput touches a physiotherapist’s hand.
- A test is terminated if a skin fold(s) is/are separated owing to loss of the chin tuck or a patient’s head touches a clinician’s hand for more than one second.
- Reliability
- Subjects without neck pain: ICC = 0.67 – 0.91, SEM 8.0 – 15.3 seconds
- Subjects with neck pain: ICC = 0.67, SEM 11.5 seconds

Upper Limb Tension Test (ULTT)
- How to perform this test:
- First of all, a patient is positioned in a supine. While the Upper Limb Tension Testthat places a bias toward testing a patient’s response to tension placed on a median nerve, an examiner sequentially introduces the following motions to a symptomatic upper extremity.
- Scapular depression,
- Shoulder abduction to approximately 90 degrees with an elbow flexed position,
- Forearm supination, wrist as well as finger extension,
- Shoulder lateral rotation,
- Elbow extension,
- Contralateral after that ipsilateral cervical side-bending
- The positive test is indicated by the presence of any of the following findings:
- Reproduction of all or part of a patient’s symptoms of tingling or numbness.
- Side-to-side differences of greater than ten degrees of an elbow or the wrist extension on the symptomatic side, contralateral cervical side-bending increases a patient’s symptoms, or ipsilateral side-bending reduces a patient’s symptoms.
- Sensitivity = 0.97
- Specificity = 0.22
- Likelihood Ratio = 1.3
- -Likelihood Ratio = 0.12
Distraction Test
- The importance of this test: Identify cervical radiculopathy
- A patient is in the supine position.
- An examiner grasps under a chin as well as occiput, flexes a patient’s neck to the position of comfort, & slightly applies the distraction force of up to approximately 14 kg.
- The positive test happens with a reduction or elimination of a patient’s upper extremity or scapular symptoms. A test is not indicated if a patient has no upper extremity or even scapular region symptoms.
- Sensitivity = 0.44
- Specificity = 0.90
- Likelihood Ratio = 4.40
- – Likelihood Ratio = 0.62

Valsalva Test
- How to perform this test:
- A patient needs to take a sitting position with he is instructed by the therapist to take a deep breath as well as hold the position while doing exhalation for five to seven seconds.
- A positive response happens with the reproduction of symptoms.
- Sensitivity = 0.22
- Specificity = 0.94
- Likelihood Ratio = 3.50
- – Likelihood Ratio = 0.83
Spurling test ( Foraminal compression test)
- Assessment of the facet joint pain as well as nerve root irritation.
- Procedure: A patient has to take a sitting position with a head rotated as well as tilted to one side.
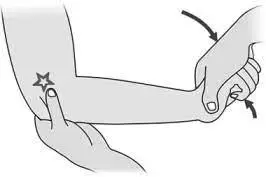
- An examiner stands behind a patient with one hand placed on the patient’s head. With another hand, an examiner lightly taps (compresses) a hand resting on a patient’s head. If a patient tolerates the initial step of a test, this is then repeated with a cervical spine extended as well.
- How to do an assessment: A test gives the clinical evidence of both the facet syndrome as well as nerve root compression. Where facet joint irritation or nerve root compression is present, an examination may intensify the pain.
- Simultaneous extension of a cervical spine narrows the intervertebral foramina by 20–30%. Existing radicular pain may be increased by the movement.

Shoulder depression test
- Why this test is important?
- To get an assessment of the nerve root compression
- Procedure:
- First of all, the side flexes the patient’s head on the unaffected side after that apply downward pressure on the opposite shoulder(affected side).
- Positive sign- increase in pain.
- The test provides evidence for nerve root compression.
Alternative distraction test
- Differentiates between radicular pain in the back of the neck, shoulder, & arm & ligamentous or muscular pain in these regions.
- Procedure: The position of patient is sitting. The inspector grasps the patient’s head regarding the jaw as well as the back of the head & applies superior axial traction.
- Assessment: Distraction of a cervical spine decreases the load on an intervertebral disk as well as exiting nerve roots within affected levels or segments during producing the gliding movement in the facet joints. Reduction of radicular symptoms, even in passive rotation, when the cervical spine is distracted is a sign of discogenic nerve root irritation. Increased pain
- while distraction, as well as rotation, suggests functional impairment in a cervical spine owing to muscular or ligamentous pathology.
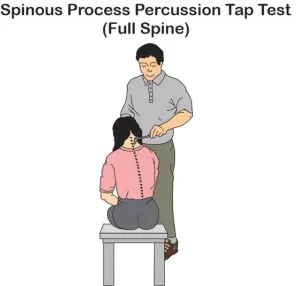
Percussion test
- How to do this test: With a patient’s cervical spine slightly flexed, an exam- inner taps the spinous processes of all the exposed vertebrae.
- How to do an assessment: Localized nonradicular pain is a sign of a fracture or of muscular or even ligamentous functional impairment. After that, radicular symptoms indicate intervertebral disk pathology along with nerve root irritation.
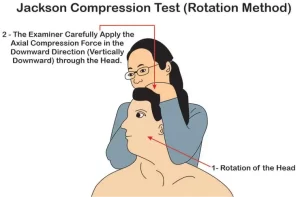
Jackson compression test
- How to perform this test on the patient:
- A patient needs to take a sitting position. An examiner stands behind a patient with his or her hand on the top of the patient’s head as well as passively tilts a head to either side. In maximum lateral bending, an examiner presses down on a head to exert axial pressure on the spine.
- Assessment: An axial loading results in increased compression of intervertebral disks, exiting nerve roots, as well as facet joints. Pressure on intervertebral foramina acts on a facet joint to elicit distal pain that does not exactly follow identifiable segmental dermatomes.
- The presence of nerve root irritation may cause radicular pain symptoms.
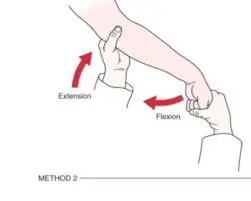
Flexion compression test
- How to perform this test: A patient has to take a seating position. An examiner stands behind a patient as well as passively moves a cervical spine into the flexion position(tilts a patient’s head forward). After that, axial compression is given to the top of the head.
- How to do an assessment: It is a good test of the integrity of an intervertebral disk. In a presence of the posterolateral disk extrusion, the maneuver may press an extruded portion of a disk in the posterior direction, resulting in increasing compression of the nerve root.
- An increase in radicular symptoms can so indicate the presence of the posterolateral disk extrusion.
Extension compression test
- How to do this test:
- A patient may take a sitting position as well as an examiner standing behind the patient. A cervical spine is extended 30°. The teste who is chief of the examination department applies axial compression to the top of the head.
- How to do an assessment: The test assesses the integrity of an intervertebral disk. Where a posterolateral extrusion with the intact annulus fibrosus is present, shifting pressure on the disks anteriorly may decrease symptoms.
- May increase the pain without radicular symptoms usually indicates irritation in facet joints as a result of reduced mobility owing to degenerative changes.
Bakody’s Sign

- Introduction
- The described test was designed to assess radicular pain, especially at C4-C6 nerve roots. It is otherwise known as a shoulder abduction test. The test may be suggestive of cervical nerve involvement, however, is not diagnostic of it.
- Purpose
- This sign is mainly utilized for diagnosing cervical radiculopathy as well as this is as definitive as a spurting test however is less painful. This may also be used in case of herniated disc pathology, spinal nerve root compression, or acute neck pain that may be neural-related.
- How to do this test:
- A subject may be sitting or even lying down. An upper limb has to be active or even passively raised above the head with a palm of a hand above the head.
- Interpretation
- Positive sign: Decrease of the symptoms with the painful arm placed on the top of the head. A suggested mechanism includes the reduction of the pain as a traction force to the nerves, as well as lower brachial plexus trunks, which are relieved. Along with the arm hanging at the side of someone’s body a mechanical traction motion on a nerve increases, therefore increasing symptoms.
- When it is called a negative sign: Increase in the symptoms when a patient’s hand is placed on a head. These symptoms are probably increased owing to inter-scalene muscle compression.
- Therefore, placing the hand can be termed positive for an inter-scalene compression as well as negative for the Bakody sign.
Cervical Distraction Test
- Purpose
- A Cervical Distraction Test is a diagnostic test for the presence of cervical radiculopathy. Position of the
- Supine or even sitting upright
- How to perform this test:
- The position of patient is supine lying as well as the neck is comfortably positioned. An Examiner securely grasps a patient either by placing each hand around a patient’s mastoid processes, standing at his head, or even placing one hand on their forehead & the other on an occiput. Slightly flex a patient’s neck as well as pull a head towards the torso, applying the distraction force.
- When called positive test is a reduction or even elimination of symptoms along with traction
- Tissues being tested
- Neural foramen along with joint capsules is around the facet joints of the cervical spine. Neck extensor muscles are also secondarily observed while the test.
- Positive Test
- If the pain is relieved as a result of the motion, after that a test is positive for nerve root compression as well as facet joint pressure. Determining the grade of pressure could be decided by the amount of pressure as well as the pain relieved while performing a cervical distraction test.
Cervical Flexion-Rotation Test
- Purpose
- A Cervical Flexion-Rotation Test (CFRT), in contrast to other forms of manual examination, is the easily applied clinical test purportedly biased assessment of the dysfunction at the C1-C2 movement segment. A C1-C2 action (motion) segment accounts for 50% of a rotation in a cervical spine.
- The manual examination has high sensitivity as well as specificity to detect the presence or even absence of cervical joint dysfunction in neck pain & headache patients. But, the described test involves a high degree of skill on the part of an examiner, and his reliability has been questioned.
- In this test procedure, a cervical spine is fully flexed, in an attempt to isolate motion to C1- C2, which has the unique ability to rotate in the flexion position. The normal range of the cervical rotation motion in end-range flexion has been shown to be 44° to each side. On the other side, subjects suffering from headaches with C1-C2 dysfunction have an average of 17° less rotation.
- One examiner(Smith et al.) concluded that age did not significantly influence mobility while the Cervical flexion rotation test.
- One explanation for it is could be that an upper cervical spine undergoes minimal age-related degenerative changes, in comparison to joints lower in a cervical spine.
- Moreover, lifestyle factors which included sleep position, time spent sitting, as well as side dominant lifestyle did not appear to influence variability in cervical mobility.
- Technique
- The position of patient is relaxed in a supine.
- The examiner fully flexes a cervical spine with an occiput resting against the examiner’s abdomen
- After that, the patient’s head is rotated to the left as well as the right side.
- If mild resistance is experienced, along with pain provoked, as well as the range is limited prior to the expected end range, after that this cervical rotation flexion test is considered positive, with the presumptive diagnosis of a limited rotation of the C1 on C2.

Cervical rotation lateral flexion test
- Purpose
- The purpose of this test is to check the presence of 1st rib hypomobility in patients with brachialgia.
- Technique
- This test is mainly done with a patient in a sitting position. A cervical spine is passively as well as maximally rotated away from a side being tested. During maintaining the position, the spine is mildly flexed as far as possible moving an ear toward the chest.
- This described test is considered positive when a lateral flexion motion is blocked.
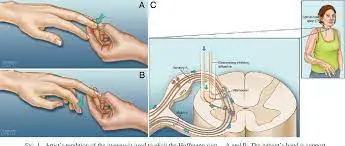
Hoffman sign
- Interpretation
- The positive Hoffman’s sign is most commonly suggestive of the corticospinal tract dysfunction localized to cervical segments of the spinal cord. In this regard, this is analogous to a Babinski sign.
- Conditions namely, multiple sclerosis, hyperthyroidism, as well as anxiety may also result in positive signs.
- Systemic disorders usually result in the bilateral response during structural anomalies namely tumors resulting in the unilateral response.
- It is worth almost noting that up to three percent of the population have been researched with a positive sign without any indication of cord compression or upper motor neuron lesion disease.
- Purpose
- The assessment of the integrity of an atlantoaxial joint & more notably the stabilizers of the dens on an Atlas. It specifically assesses the integrity of a Transverse Ligament. If a transverse ligament that maintains a position of an odontoid process relative to C1 is torn, C1 may translate forwards on the C2 in flexion.
- Atlantoaxial instability is the complication of rheumatoid arthritis in the cervical spine, mostly seen in 29-70% of RA patients. A cervical spinal cord compromise because of the atlantoaxial subluxation can have serious neurological results, which mainly include quadriplegia as well as death.
- Technique
- A patient has to take a sitting position. An examiner places the palm of one hand on a patient’s forehead, as well as an index finger or even thumb of another hand on a tip of a spinous process of an axis (C2).
- A patient is asked to gradually flex a head doing the slight cervical nod, and at the same duration, an examiner presses posteriorly on a patient’s forehead.
- The sliding movement of a head in relation to an axis indicates atlantoaxial instability. The positive result can also be accompanied by a reduction in symptoms, the “clunk” sensation, or the patient reports of the “click” or “clunk” felt in the roof of their mouth.
- This is thought that this technique decreases atlantoaxial subluxation caused by the forward flexion of the unstable cervical spine.
- A spinal suggests that if the upper cervical instability is suspected, a Sharp-Purser test may be done first before any other ligamentous test.
- If, and only if, a Sharp-Purser is negative, A spinal then suggests that, in an absence of neurological symptoms, the test that passively moves an atlas on an axis be used for assessing for laxity of a transverse ligament, namely, a transverse ligament stress test.
- A Sharp-Purser test is not without controversy, this is stated that the test is intended to relieve neurological symptoms, but Meadows called the use of a Sharp-Purser in a presence of neurological symptoms the “exercise in futility & risk.
Transverse Ligament Stress Test
- Purpose
- The transverse Ligament Stress Test(TLST) for hypermobility of the atlantoaxial articulation.
- Technique
- A patient is placed in the supine position with a physical therapist supporting the patient’s head along with the palms as well as the 3rd-5th fingers.
- A physical therapist places the index fingers between the occiput as well as the spinous process of C2, thus the index fingers are over the neural arch of the C1 vertebra.
- The physical therapist lifts the patient’s head as well as the C1 vertebra anteriorly, without giving permission for flexion or even extension.
- A position may be held for nearly five to fifteen seconds, according to the patient’s ability.
- The positive test is a recurrence of symptoms:
- Abnormal pupil response, eye twitching or nystagmus, soft end-feel, muscle spasm, dizziness, nausea, paresthesia of a lip face, or even limb, lump sensation in the throat.
Vertebral Artery Test
- Description
- The vertebral artery test (VAT) is mainly used in the field of physical therapy to test the vertebral artery blood flow to the brain, finding for symptoms of vertebral artery insufficiency as well as disease.
- A test maneuver causes the reduction of a lumen at the third division of a vertebral artery, resulting in a reduction in the blood flow of an intracranial VA of a contralateral side. The causes of this condition are ischemia, owing to blood loss in the pons as well as the medulla oblongata of the brain.
- It results in dizziness, nausea, syncope, dysarthria, and dysphagia, along with disturbances of the hearing or vision, paresis, or even paralysis of patients with Vertebrobasilar Insufficiency (VBI).
- Purpose of the test
- The vertebral artery test is mainly utilized to test a vertebral artery blood flow, researching or finding symptoms of vertebral artery insufficiency.
- The reduction of blood flow can result in a transient ischemic attack (TIA), the critical sign of an impending stroke. This could mean that, if a disease is not quickly diagnosed, there is the risk of missing an opportunity to prevent permanent disability or death or if a cervical spine is placed in a compromising position, there is the risk of causing permanent disability or death.
- Technique of this test
- The active range of movement of a cervical spine is usually done before passive assessment.
- After that, Place the patient in a supine position along with doing the passive extension as well as side flexion of the head 7 necks.
- Do passive rotation of a neck to the same side & hold for approximately thirty seconds.
- Try to repeat the test with the head motion to the opposite side.
- Do repeat test is considered positive if there is a dropping of the arms, along with loss of balance, or pronation of the hands; the positive result indicates reduced blood supply to the brain.
- Modification:
- Next, rotate a head to the opposite side to a tested side maximally as well as holds the position for nearly five to seven seconds
- Come back to neutral for five to seven seconds.
- Extend head for ten to eleven seconds.
- Return to the neutral for five to seven seconds
- Extends as well as rotate the head (against the opposite tested side) maximally for nine to fifteen seconds
- Positive symptoms include (The 5 D’s) dizziness, diplopia, dysarthria, dysphagia, drop attacks, nausea as well as vomiting, sensory changes, and nystagmus.

FAQ
Examination of a neck includes inspection for scars, masses, and glandular or even nodal enlargement. Inspect a trachea, noting any deviation. After that, inspect a thyroid gland as a patient swallows, noting any enlargement.
C1, C2, & C3 (the first 3 cervical nerves) control the head along with the neck, including actions forward, backward, as well as to sides. These nerves also play the main roles in breathing. A C2 dermatome mainly handles sensation for the upper part of the head of our body, while a C3 dermatome covers the side of the face along with behind the head.
A cervical spine, comprised of 7 cervical vertebrae referred to as C1, C2, C3, C4, C5, C6 as well as C7, is divided into 2 major segments: a craniocervical junction (CCJ) as well as a subaxial spine. The craniocervical junction includes an occiput & two most cervical vertebrae, known as an atlas (C1) as well as the axis (C2).
Examination of a head
Inspect a skull as well as the face. Inspect the skin as well as the scalp. Palpate skull (especially if the patient complains of tenderness or even recent trauma). Assess facial sensation & motor function.
In general, a standard physical exam typically includes Vital signs: blood pressure, breathing rate, pulse rate, temperature, height, as well as weight. Vision acuity: testing a sharpness or clarity of vision from the distance. Head, eyes, ears, nose as well as throat exam: inspection, palpation, & testing, as appropriate
Manual Muscle Testing of a Cervical Spine
An examiner applies resistance with one hand over an occiput, as well as another hand is placed under a head should this give way with applied resistance. The model is supine with the head on the table as well as arms at the side. An examiner is standing at the head of the table facing the patient.