RHEUMATOID ARTHRITIS
Table of Contents
What is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) can affect your knees and any other joint in your body. It’s an immune system disorder in which the body attacks itself, and especially the joints.
Rheumatoid arthritis (RA) is a systemic disease of the immune system. It affects multiple joints in the upper and well as the lower limbs. Knees joint are one of the common joints affected by RA. RA can occur at any age and can affect both knees.
ANATOMY:

The three bone structures of the knee are the femur (thigh bone), tibia (shin bone), and patella (kneecap). These structures are connected by four major ligaments; ligaments connect bones to other bones.
The ACL prevents forward movement (anterior translation) of the lower leg as well as stabilizes the knee from rotational stress of the tibia. When rotational stress is applied when a cut or quick change in direction is performed, the ACL prevents anterior translation of the tibia, thus preventing tibial sub-luxation during the movement.
The shock-absorbing structures between the femur and tibia are the medial and lateral meniscus. The weight-bearing surfaces of the knee are covered by articular surface cartilage allowing the joint to move freely. The menisci act as shock absorbers and work in conjunction with the articular cartilage to reduce stresses placed upon them with movement.
The four main ligaments of the knee are:
- Anterior Cruciate Ligament (ACL)
- Posterior Cruciate Ligament (PCL)
- Medial Collateral Ligament (MCL)
- Lateral Collateral Ligament (LCL)
These ligaments connect the femur to the tibia and provide the structural integrity to the knee. There are other structures within the knee that are important for proper function such as the menisci, articular cartilage and the patella.
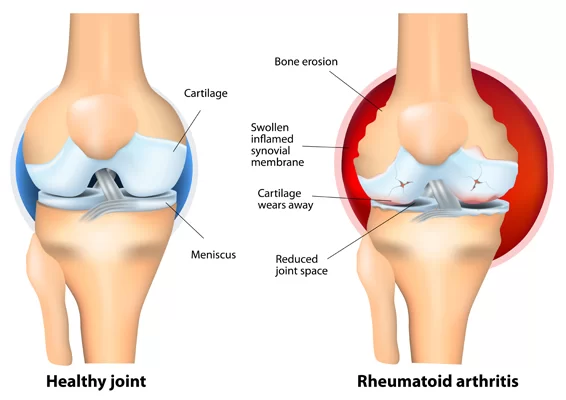
PATHOLOGY:
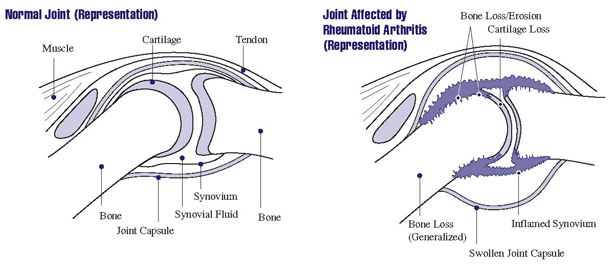
When RA affects the knee joint the synovium that lines the ends of the bones in the joints thickens and produces an excess of joint fluid.
This excess fluid, along with inflammatory chemicals that the immune system releases, leads to swelling and damage to the cartilage that acts as a cushion within the joint leading to pain, and joint erosion.
CAUSES:
The exact cause of rheumatoid arthritis is unknown. It’s possible that a virus or bacteria may trigger the disease in people with a genetic predisposition to rheumatoid arthritis.
Many doctors think rheumatoid arthritis is an autoimmune disease in which the tissue of the joint’s lining is attacked by the body’s immune system. It’s also possible that rheumatoid arthritis is caused by severe stress. The onset of rheumatoid arthritis occurs most frequently in middle age and is more common among women.
Cigarette smoking significantly increases the risk of developing rheumatoid arthritis.
There is some evidence that if you eat a lot of red meat and don’t consume much vitamin C, you may have an increased risk of developing rheumatoid arthritis.
SIGN & SYMPTOMS :-
- Joint Pain is present over the knee joint often affecting both right and left.
- Swelling and inflammation of the joint.
- The joint feels hot or warm to the touch.
- Joint Stiffness and loss of motion of the knee (or other joint) when bending and/or straightening the joint.
- Weakness, which may be manifested as difficulty walking, getting up from a sitting position, kneeling, squatting or climbing stairs.
- Fatigue or tiring easily when performing normal daily activities.
CLASSIFICATION OF RA STAGES:
I: Early – 1. Early destructive changes on radiographic examination
2. Radiographic evidence of osteoporosis may be present
II: Moderate – 1. Radiographic evidence of osteoporosis, with or without slight subchondral bone destruction; slight cartilage destruction may be present
2.No joint deformities, although the limitation of joint mobility may be present
3. Adjacent muscle atrophy
4. Extra-articular soft tissue lesions, such as nodules and tenosynovitis may be present
III. Severe – 1. Radiographic evidence of cartilage and bone destruction, in addition to osteoporosis
2. Joint deformities, such as subluxation, ulnar deviation, or hyperextension, without fibrous or bony ankylosis
3. Extensive muscle atrophy
4. Extra-articular soft tissue lesions, such as nodules and tenosynovitis may be present
IV. Terminal – 1. Fibrous or bony ankylosis
2. Criteria of Stage III
DIAGNOSIS:
1. Blood tests
Blood tests may be used to find changes in your blood that are produced by inflammation. They can also show if you’re anemic (have low levels of iron in your blood), as anemia is common in people with rheumatoid arthritis.
2. X-rays
X-rays will show any damage caused to the joints by the inflammation that occurs in rheumatoid arthritis. Doctors also use equipment such as ultrasound scans to look for inflammation and early damage to joints.
Treatment of Rheumatoid arthritis:
1.NSAIDs
Nonsteroidal anti-inflammatory drugs (NSAIDs) can relieve pain and reduce inflammation. Over-the-counter NSAIDs include ibuprofen (Advil, Motrin IB) and naproxen sodium (Aleve). Stronger NSAIDs are available by prescription. Side effects may include ringing in your ears, stomach irritation, heart problems, and liver and kidney damage.
2. Steroids.
Corticosteroid medications, such as prednisone, reduce inflammation and pain and slow joint damage. Side effects may include thinning of bones, weight gain and diabetes. Doctors often prescribe a corticosteroid to relieve acute symptoms, with the goal of gradually tapering off the medication.
3. Disease-modifying antirheumatic drugs (DMARDs) :
These drugs can slow the progression of rheumatoid arthritis and save the joints and other tissues from permanent damage. Common DMARDs include methotrexate (Trexall, Otrexup, Rasuvo), leflunomide (Arava), hydroxychloroquine (Plaquenil), and sulfasalazine (Azulfidine).
Side effects vary but may include liver damage, bone marrow suppression, and severe lung infections.
4. Biologic agents
Also known as biologic response modifiers, this newer class of DMARDs includes abatacept (Orencia), adalimumab (Humira), anakinra (Kineret), certolizumab (Cimzia), etanercept (Enbrel), golimumab (Simponi), infliximab (Remicade), rituximab (Rituxan), tocilizumab (Actemra) and tofacitinib (Xeljanz).
These drugs can target parts of the immune system that trigger inflammation that causes joint and tissue damage. These types of drugs also increase the risk of infections.
SURGERY

- Synovectomy: Surgery to remove the inflamed synovium (lining of the joint). Synovectomy can be performed on knees, elbows, wrists, fingers, and hips.
2. Joint fusion:- Surgically fusing a joint may be recommended to stabilize or realign a joint and for pain relief when a joint replacement isn’t an option.
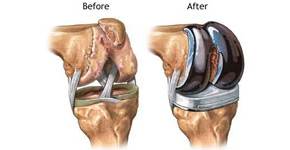
3. Total joint replacement:- During joint replacement surgery, your surgeon removes the damaged parts of your joint and inserts a prosthesis made of metal and plastic.
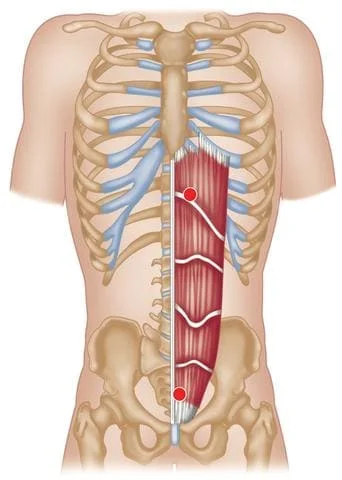
Physiotherapy treatment in Rheumatoid arthritis:
Heat and Ice Therapy :
Heat – heat works to reduce muscle tension and stimulate blood circulation. You may find that applying something warm prior to getting up in the morning, or during the day helps reduce discomfort and stiffness in your joint.
Ice – Ice helps to reduce inflammation in muscles and joints by constricting blood vessels and preventing fluids from leaking into surrounding tissues. You should try icing your joints after any significant activity or at the end of the day. This can minimize the inflammation resulting from daily activities.
Transcutaneous electrical nerve stimulation (TENS) is used to relieve pain.
Ultrasound Therapy: Ultrasound therapy uses sound waves to create a gentle heat that increases blood circulation to the patient’s deep tissues.
Exercise in Rheumatoid arthritis:
SQE (Static Quadriceps exercise):
Remain lying on your back with your legs straight and place a rolled-up towel under the knees. Tighten the front thigh muscle (quadriceps) by pushing the knee into the towel. Hold for 10 seconds and then release for 20 seconds. Repeat this process 10 times.

AHKF (Active Hip-Knee flexion exercise):
Lie on the floor (or bed if the floor is difficult) with your knee straight, and slowly bend the affected knee as far as possible (moving your ankle as close to your bottom as possible). When you feel a stretch in the thigh muscle hold the position for 10 seconds then return to a straightened position and hold again for 10 seconds. Repeat 10 times.
SLR (Straight leg Raising) :
Lie flat on your back on the floor or bed with your arms at your sides, toes up.
Keep your leg straight while tightening your leg muscles, and slowly lift it several inches.
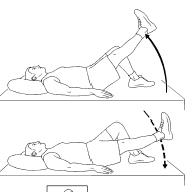
Tighten your stomach muscles to push your lower back down.
Hold and count to 5, then lower your leg as slowly as possible.
Repeat, then switch to the other leg.
SIDE LEG RAISES
Lie on one side with your legs stacked. Bend the bottom leg for support. Straighten the top leg and raise it to 45 degrees. Hold for 5 seconds, lower and relax briefly, then repeat 10-15 times.

Switch sides and start over. Want to try a bit of a different spin on the move? Point the toe of your upper leg slightly toward the floor as you raise it.
PRONE STRAIGHT LEG RAISES
Lie on your stomach with your legs straight. Tighten the muscles in your bottom and the hamstring of one leg, and lift toward the ceiling. Hold for 3-5 seconds, lower, and repeat. Do 10 -15 lifts and switch sides. You can add ankle weights as you gain strength. You shouldn’t feel back pain. If you do, limit how high you lift up. If it still hurts, stop
HAMSTRING CURLS
These are the muscles along the back of your thigh. Lie flat on your stomach. Slowly bring your heels as close to your butt as you can, and hold that position. Do three sets of 15. You can also do this exercise standing while you hold onto a chair and lift one leg at a time. If this becomes easy, you can add ankle weights, slowly increasing the weight from 1 to 3 to 5 pounds.
HALF SQUAT
Stand with your feet shoulder-distance apart and stretch your arms out in front of you.

Slowly bend your knees until you’re in a half-sitting position. Hold on to a chair for balance, if necessary.
Keep your back straight and chest lifted — don’t lean forward.
With your feet flat on the floor, hold the position for 5 seconds, then slowly stand back up.
There should be no pain while performing this exercise. Do 10 repetitions, and slowly work up to three sets of 10.
LDE (last-degree knee extension):
Sit on a mat and place a rolled towel right below the arthritic knee. Make sure your heel touches the floor.
Flex the other knee and place the sole of your foot against the towel. Place your palms behind you on the mat. This is your starting position.
Flex your foot so that your toes point straight up at the ceiling. Raise your lower leg so that your shin bone and knee are at the same level.
Hold this pose for a second. Lower your leg back to the starting position.
3 sets of 8 reps. Do this 3-4 times a day.
DO’S & DON’TS:
1) Cross-leg sitting:
can’t sit with cross Legs on the floor (as the Indian custom of eating) but you can on a high-rise bed. The funda is when you sit on the floor and get up there is tremendous pressure on your knees
2) Kneecaps:
people with severe knee pain and swelling need to use it as a support keeping in mind to do the knee exercises religiously.
3) Walking:
You need to walk in a pain freeway at a pain-free speed. Kneecaps can be worn while walking and obese people need to do warm-up and muscle-strengthening exercises before they decide to walk in order to capacitate their knees to take their heavy body weight.
4) Hot packs:
get temporary relief from pain and swelling.
5) Weight loss:
Obese ladies and gentlemen reduce their weight with proper exercise and dieting
6) Ergonomics:
Maintain your body posture while sitting and standing. While sitting for long hours take a walk break every 30min or do a few knee movements. While standing, take a break every 30 min by having a walk or sitting, or taking some sort of support.
7) Avoidance:
avoid squatting i.e. using Indian toilets, and shift to the Western system to reduce excessive loading of your knees. Stair climbing also needs to be avoided whenever possible. Another way to climb stairs is by using side rails or sticks and instead of climbing the steps with a forward step take a side step by facing the side railing instead of the front steps.
8) Footwear:
Wear comfortable shoes or whatever you prefer but avoid heels -both male and female-were ergonomically designed footwear that provides adequate cushioning and reduces ground reaction force.
9) Best activity for knee pain: Swimming, elliptical trainer, static cycle, and yoga.




30 Comments