KNEE REPLACEMENT
Table of Contents
Introduction
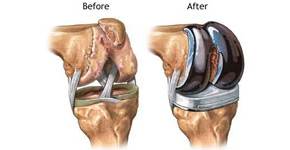
- Knee replacement, also called arthroplasty, is a surgical procedure to resurface a knee damaged by arthritis.
- Metal and plastic parts are used to cap the ends of the bones that form the knee joint, along with the kneecap.
- This surgery may be considered for someone who has severe arthritis or a severe knee injury.
Types of arthritis
- Osteoarthritis – a degenerative joint disease that affects mostly middle-aged and older adults, may cause the breakdown of joint cartilage and adjacent bone in the knees.
- Rheumatoid arthritis – which causes inflammation of the synovial membrane and results in excessive synovial fluid, can lead to pain and stiffness.
- Traumatic arthritis – arthritis due to injury, may cause damage to the cartilage of the knee.
The goal of knee replacement surgery is to resurface the parts of the knee joint that have been damaged and to relieve knee pain that cannot be controlled by other treatments.
Types of Knee replacement
There are four main types of knee replacement surgery:
Total knee replacement
- This is the most common form.
- Your surgeon replaces the surfaces of the thigh bone and shin bone that connect to the knee.
Partial knee replacement
- If arthritis affects only one side of your knee, this surgery may be a possibility.
- However, it’s only right for you if you have strong knee ligaments.
- Partial knee replacement can be performed through a smaller cut than is needed for total knee replacement.
Knee cap replacement
- This replaces only the under-surface of the kneecap, but some surgeons advise against this procedure because total knee replacement surgery has a higher rate of success.

Complex (or revision) knee replacement
- This procedure may be needed if you have very severe arthritis or if you’ve already had more than one knee replacement surgery.
Causes
- Knee replacement surgery is a treatment for pain and disability in the knee. The most common condition that results in the need for knee replacement surgery is osteoarthritis.
- Osteoarthritis is characterized by the breakdown of joint cartilage.
- Damage to the cartilage and bones limits movement and may cause pain.
- People with severe degenerative joint disease may be unable to do normal activities that involve bending at the knee, such as walking or climbing stairs, because they are painful.
- The knee may swell or “give-way” because the joint is not stable.
- Other forms of arthritis, such as rheumatoid arthritis and arthritis that results from a knee injury, may also lead to degeneration of the knee joint. In addition, fractures, torn cartilage, and/or torn ligaments may lead to irreversible damage to the knee joint.
- If medical treatments are not satisfactory, knee replacement surgery may be an effective treatment.
Some medical treatments for degenerative joint disease may include, but are not limited to, the following:
- Anti-inflammatory medications
- Glucosamine and chondroitin sulfate
- Pain medications
Other Treatment
- Limiting painful activities
- Assistive devices for walking (such as a cane)
- Physical therapy
- Cortisone injections into the knee joint
- Viscosupplementation injections (to add lubrication into the joint to make joint movement less painful)
- Weight loss (for obese persons)
- There may be other reasons for your doctor to recommend a knee replacement surgery.
Risks of the procedure
As with any surgical procedure, complications can occur. Some possible complications may include, but are not limited to, the following:
- Bleeding
- Infection
- Blood clots in the legs or lungs
- Loosening or wearing out of the prosthesis
- Fracture
- Continued pain or stiffness
- The replacement knee joint may become loose, be dislodged, or may not work the way it was intended.
- The joint may have to be replaced again in the future.
- Nerves or blood vessels in the area of surgery may be injured, resulting in weakness or numbness.
- The joint pain may not be relieved by surgery.
- There may be other risks depending on your specific medical condition.
Precautions
Be sure to discuss any concerns with your doctor prior to the procedure.
Before the procedure:
- Your doctor will explain the procedure to you and offer you the opportunity to ask any questions that you might have about the procedure.
- You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully and ask questions if something is not clear.
- In addition to a complete medical history, your doctor may perform a complete physical examination to ensure you are in good health before undergoing the procedure. You may undergo blood tests or other diagnostic tests.
- Notify your doctor if you are sensitive to or are allergic to any medications, latex, tape, and anesthetic agents.
- Notify your doctor of all medications (prescribed and over-the-counter) and herbal supplements that you are taking.
- Notify your doctor if you have a history of bleeding disorders or if you are taking any anticoagulant (blood-thinning) medications, aspirin, or other medications that affect blood clotting. It may be necessary for you to stop these medications prior to the procedure.
- If you are pregnant or suspect that you are pregnant, you should notify your doctor.
- You will be asked to fast for eight hours before the procedure, generally after midnight.
- You may meet with a physical therapist prior to your surgery to discuss rehabilitation.
- Arrange for someone to help around the house for a week or two after you are discharged from the hospital.
- Based on your medical condition, your doctor may request other specific preparations.
During the procedure:
- Knee replacement requires a stay in a hospital.
- Procedures may vary depending on your condition and your doctor’s practices.
- Knee replacement surgery is most often performed while you are asleep under general anesthesia. Your anesthesiologist will discuss this with you in advance.
Procedure
- You will be asked to remove clothing and will be given a gown to wear.
- An intravenous (IV) line may be started in your arm or hand.
- You will be positioned on the operating table.
- A urinary catheter may be inserted.
- If there is excessive hair at the surgical site, it may be clipped off.
- The anesthesiologist will continuously monitor your heart rate, blood pressure, breathing, and blood oxygen level during the surgery.
- The skin over the surgical site will be cleansed with an antiseptic solution.
- The doctor will make an incision in the knee area.
- The doctor will remove the damaged surfaces of the knee joint and resurface the knee joint with the prosthesis.
- The knee prosthesis is made up of metal and plastic.
- The most common type of artificial knee prosthesis is a cemented prosthesis.
- Uncemented prostheses are not commonly used anymore.
- A cemented prosthesis attaches to the bone with surgical cement.
- An uncemented prosthesis attaches to the bone with a porous surface onto which the bone grows to attach to the prosthesis. Sometimes, a combination of the 2 types is used to replace a knee.
- The prosthesis is generally comprised of 3 components:
1 – the tibial component (to resurface the top of the tibia, or shin bone)
2 – the femoral [thigh bone] component (to resurface the end of the thighbone; and
3 – the patellar component (to resurface the bottom of the kneecap that rubs against the thighbone). - The incision will be closed with stitches or surgical staples.
- A drain may be placed in the incision site to remove fluid.
- A sterile bandage or dressing will be applied.
Physiotherapy treatment:
- This may surprise you, but you can expect to start PT within a day of your operation.
- A physical therapist will come to your hospital room and show you exercises you should start doing right away. You’ll have fresh stitches and a brand-new body part. Trust that the moves are safe, though. They’re designed to:
Goals
- Strengthen your leg muscles
- Restore knee movement
- Help you walk on your new knee
Home or Rehab Clinic:
- Most people spend 1 to 3 nights in the hospital. After you’re discharged, you might check into a rehab facility. There, you’ll usually get physical therapy 6 days a week for a couple of weeks. One advantage of a rehab clinic is that you will have help and you’re sure to do your exercises every day.
- Most people will go straight home. Done right, home PT is just as helpful as in-patient rehab. You likely will need in-home physical therapy several days per week for 4-6 weeks.
- A third way is to do your PT at an outpatient rehab clinic. Some people have even knee surgery itself as an outpatient, without an overnight stay. Your doctor will decide the best option for you based on your age and health.
If you go home instead of to a rehab clinic, keep these tips in mind:
- Help your wound heal. Don’t soak it in water until it’s sealed and healed. Ask your doctor for advice on when showering after surgery is safe.
- Eat right. Even if you don’t have an appetite after the operation, make sure to eat nutritious foods. Your doctor may also suggest an iron supplement or fiber-rich foods lower possible problems with medications.
- Move your new knee. Chances are you’ll get a walking plan that starts inside and then takes you outside as you get stronger. On top of that, you’ll do PT moves a few times a day at home.
- Exercise Schedule:-
- It’s not what most people would call a workout. But PT after knee surgery will make you stronger. You can expect to do 20-30 minutes of PT two or three times a day. You also may need to walk for half an hour at least a couple of times daily.
Exercise Protocol
Day 1:
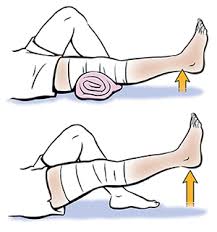
- At the hospital, a physical therapist will guide you as you get out of bed and put weight on your new knee for the first time. You might even take a few steps with a walker.
- The therapist also will help you with bedside exercises. An example is to tighten your thigh muscles, hold for 5-10 seconds, release, and repeat 10 times. You’ll also “pump” your ankles by moving your foot up and down to tighten your shin and calf muscles.
Day 2:

- You’ll keep doing exercises to strengthen the muscles that support your knee. You will practice bending and straightening your knees, as well as flexing and relaxing your thigh muscles. You’ll also walk farther, either with a walker or crutches.
Days 3-5:
- You might still be in the hospital, or discharged to a rehab center or back home. You continue with as much PT as you can handle. With help, you might even climb some stair steps.
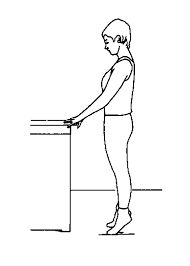
Day 5 – week 4:

- You slowly ramp up your exercises as your knee gets stronger. During this time, you may:
- Walk farther with your walker or crutches. Need only a cane or a single crutch to walk. You can do this once you can stand for more than 10 minutes. Use an exercise bike. At first, you pedal backward only. You can pedal forward when your knee is strong enough.
After 4 weeks

- your physiotherapist may suggest you add light weights to add resistance. You should stick with all recommended exercises for at least 2 full months after your surgery.
- Back to Regular Life
- You might drive again as soon as 3 weeks after your surgery. But most people need 4-6 weeks before they can bend their knee to get in and out of the car.
In 3-6 weeks
- you could shop for groceries, get up from a chair, and do other things that were difficult before the surgery. Just remember that you might not be 100% pain-free. Let your doctor know about any pain that bothers you.
- Your knee could last more than 15 years, but it will eventually wear out. It’ll last longer if you avoid putting stress on it with activities like:

- Running
- Skiing
- Tennis
- Sports that involve jumping
The good news is that it’s easy to stay fit with your artificial knee. You can:
- Walk
- Swim
- Golf
- Go on light hikes
- Bike
- Dance
Pain Management
- After surgery, you will feel some pain. This is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover from surgery faster.
- Medications are often prescribed for short-term pain relief after surgery. Many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
- Be aware that although opioids help relieve pain after surgery, they are a narcotic and can be addictive. Opioid dependency and overdose have become a critical public health issue in the U.S. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids. Talk to your doctor if your pain has not begun to improve within a few days of your surgery.
- Blood Clot Prevention
- Your orthopedic surgeon may prescribe one or more measures to prevent blood clots and decrease leg swelling. These may include a special support hose, inflatable leg coverings (compression boots), and blood thinners.
- Foot and ankle movement also is encouraged immediately following surgery to increase blood flow in your leg muscles to help prevent leg swelling and blood clots.
Preventing Pneumonia:
- It is common for patients to have shallow breathing in the early postoperative period. This is usually due to the effects of anesthesia, pain medications, and increased time spent in bed. This shallow breathing can lead to a partial collapse of the lung which can make patients susceptible to pneumonia. To help prevent this, it is important to take frequent deep breaths. Your nurse may provide a simple breathing apparatus called a spirometer to encourage you to take deep breaths.
At Home:
The success of your surgery will depend largely on how well you follow your orthopaedic surgeon’s instructions at home during the first few weeks after surgery.
Wound Care
- You will have stitches or staples running along your wound or a suture beneath your skin on the front of your knee. The stitches or staples will be removed several weeks after surgery. A suture beneath your skin will not require removal.
- Avoid soaking the wound in water until it has thoroughly sealed and dried. You may continue to bandage the wound to prevent irritation from clothing or support stockings.
Diet - Some loss of appetite is common for several weeks after surgery. A balanced diet, often with an iron supplement, is important to help your wound heal and to restore muscle strength.
- Activity:-
- Exercise is a critical component of home care, particularly during the first few weeks after surgery. You should be able to resume most normal activities of daily living within 3 to 6 weeks following surgery. Some pain with activity and at night is common for several weeks after surgery.
Your activity program should include:
- A graduated walking program to slowly increase your mobility, initially in your home and later outside
- Resuming other normal household activities, such as sitting, standing, and climbing stairs
- Specific exercises several times a day to restore movement and strengthen your knee. You probably will be able to perform the exercises without help, but you may have a physical therapist help you at home or in a therapy center during the first few weeks after surgery.
- You will most likely be able to resume driving when your knee bends enough that you can enter and sit comfortably in your car, and when your muscle control provides adequate reaction time for braking and acceleration. Most people resume driving approximately 4 to 6 weeks after surgery.
Warning signs of blood clots:
The warning signs of possible blood clots in your leg include:
- Increasing pain in your calf
- Tenderness or redness above or below your knee
- New or increasing swelling in your calf, ankle, and foot
Warning signs of pulmonary embolism. The warning signs that a blood clot has traveled to your lung include:-
- Sudden shortness of breath
- Sudden onset of chest pain
- Localized chest pain with coughing
Preventing Infection:
- A common cause of infection following total knee replacement surgery is from bacteria that enter the bloodstream during dental procedures, urinary tract infections, or skin infections. These bacteria can lodge around your knee replacement and cause an infection.
- After knee replacement, patients with certain risk factors may need to take antibiotics prior to dental work, including dental cleanings, or before any surgical procedure that could allow bacteria to enter the bloodstream. Your orthopaedic surgeon will discuss with you whether taking preventive antibiotics before dental procedures is needed in your situation.
- Warning signs of infection. Notify your doctor immediately if you develop any of the following signs of a possible knee replacement infection:-
- Persistent fever (higher than 100°F orally)
- Shaking chills
- Increasing redness, tenderness, or swelling of the knee wound
- Drainage from the knee wound –
- Increasing knee pain with both activity and rest
Avoiding Falls:
- A fall during the first few weeks after surgery can damage your new knee and may result in a need for further surgery. Stairs are a particular hazard until your knee is strong and mobile. You should use a cane, crutches, a walker, hand rails, or have someone to help you until you have improved your balance, flexibility, and strength.
- Your surgeon and physical therapist will help you decide what assistive aides will be required following surgery and when those aides can safely be discontinued.
Protecting Your Knee Replacement:
After surgery, make sure you also do the following:
- Participate in regular light exercise programs to maintain proper strength and mobility of your new knee.
- Take special precautions to avoid falls and injuries. If you break a bone in your leg, you may require more surgery.
- Make sure your dentist knows that you have a knee replacement. Talk with your orthopaedic surgeon about whether you need to take antibiotics prior to dental procedures.
- See your orthopaedic surgeon periodically for a routine follow-up examination and x-rays, usually once a year.
- Extending the Life of Your Knee Implant:-
- Currently, more than 90% of modern total knee replacements are still functioning well 15 years after the surgery. Following your orthopaedic surgeon’s instructions after surgery and taking care to protect your knee replacement and your general health are important ways you can contribute to the final success of your surgery.



3 Comments