USE OF COLD THERAPY IN PHYSIOTHERAPY
Table of Contents
DEFINITION:
the application of cold to the tissues after an injury is a practice as old as medicine itself. the local temperature of the tissue may be reduced by the application of various forms of ice or frozen of ice or frozen gel packs, or by the evaporation of volatile fluids from the skin. often the skin temperature is reduced to 10 c.
Ice therapy may be used to:
1) reduce pain
2) reduce spasticity
3) reduce muscle spasm
4) reduce swelling
5) promote repair
6) provide excitatory stimulus when muscles are inhibited.
Physical principles
when ice is applied to the skin, heat is conducted from the skin to the ice in order to melt it. to change its state, the ice requires considerable energy to raise the temperature of 1 g of ice at 0 Celcius to 1 g of water at 37 c requires only 155 j.
Physiological effects and uses
1) circulatory response
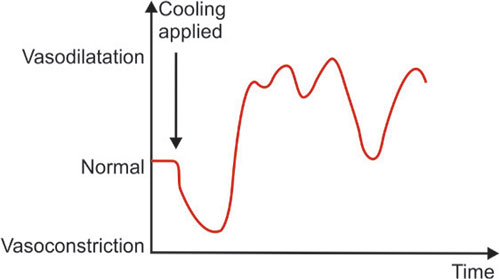
the neural response of the skin to cooling is an attempt to preserve heat, and this is accomplished by an initial local vasoconstiction. this homeostatic response has the effect of allowing the part to become very cold. after a short periods there follow a vasodilation ans then alternate periods of constriction and dilatation. this apperent hunting for a mean point of circulation is called lewis’s hunting reaction. some authorities suggest that during the periods of vasodilatation the arteriovenous anastomosis is closed, thus causing an increased blood flow through the capillaries.this is beneficial in the treatment of swelling and tissue damage.
Physiotherapeutic uses of circulatory effect
1) the initial vasoconstriction is often used to limit the extravasation of blood into the tissues following injury, e.g, sports injuries ice therapy is then usually followed by some form of compression bandage.
2) the alternate periods of vasoconstriction and dilatation affect the capillary blood flow, and it is across the capillary meembrane that tissue fluid and metabolic exchange take place. consequently an effect is being produced at a very local level which can reduce swelling: excess tissue fluid can be removed from the area and returned to the systemic circulation. increased circulation allows more nutrients and repair
substance into damaged areas. thus ice is very useful in removing swelling and aiding repair. for instance, ice-cube massage may be used to accelerate the rate of repair of bed-sores.
3) the reduced metabolic rate of cooled tissues allows cooled muscle to contract many more time before fatigue sets in.
4) it is possible that the incresed circulation could carry away chemical substance which are stimulating nocieceptor and producing pain as in the case of local tissue damage or accumalation of metabolites.
2) neural response
the skin contains primary thermal receptors. t here are several times more cold than warm receptors. the cold receptors respond to cooling by a sustained discharge of impulses, the rate of which increase with further cooling.
it has been shown that the rate of conduction of nerve fibres in a mixed peripheral nerve is reduced by cooling.mixed peripheral nerve is reduced by cooling. the first fibres affected by gradual cooling the first fibres affected by gradual cooling are the A fibres. eventually, at very low temperature, the B and then C fibres are affected
Reduction of pain
this is one of the major effects of ice and ice has been used to relieve pain for many years. the probable mechanism involved is the stimulation of cold receptors which send back impulses which have to pass into the spinal cord via the posterior root. these impulses which arrive through relatively large-diameter nerves, effectively block out any other impulses attempting to gain access to the cord, i.e. the pain-gate is closed the cold stimulation itself could be considered noxious, and as such cause stimulation of area in the mid-brain which may in turn release B endorphine or enkephalin into the posterior horn, with a consequent reduction of pain. this reduce pain temporarily.
Reduction of spasticity
spasticity is the pathogical state of increased muscle tone resulting from damage to the upper motor neuron. often the small anterior horn cell is released from the higher control of the extrapyramidal system and fires spontaneously at in increased rate. the net result of this is ultimately to increase tone in the extrafusal muscle fibres, when the hypertonic spastic state appears.
spasm is a normal response to injury or pain and is manifested as an increase in muscle tone in a specific area with the apparent aim of limiting movement and futher damage. however, the amount of spasm produced is often far in excess of the that needed just to afford protection, and the sustaind contraction of muscle itself starts to produce pain, often resulting in more spasm. the mechanism by which cold reduces spasticity and spasm are probably the same.
Excitatory cold
when cold is applied in an appropriate way the skin stimulus of ice can be used to increase the excitatory bias around the anterior horn cells. combined with other forms of excitation and with the patient’s volition, this can often produce contraction in an inhibited muscle.this effect can be used where muscles are inhibited post-operatively.
Types of ice and cold packs
1) ICE TOWEL.

Wet a towel with cold water and squeeze it until it is just damp. Fold the towel, place it in a plastic bag, and freeze it for 15 minutes. Remove the towel from the bag and place it on the injured or sore area.
2) ICE PACKS.

Put about 1 lb (0.5 kg) of ice in a plastic bag or ice pack you buy at the store. Add enough water to barely cover the ice. Squeeze the air out of the bag and seal it. Wrap the bag in a wet towel and apply to the affected area.
COLD PACKS
- Bags of frozen peas or corn are inexpensive, last 10 to 20 minutes, and mold well to your body.
- Mix 3 cups (710 mL) water and 1 cup (235 mL) rubbing alcohol in a freezer bag. Seal the bag and place it in
- the freezer until slush forms. Refreeze the bag when the slush melts.
- You can also buy cold packs that can be reused. Store them in your freezer. Some of them are designed to wrap around an injured area, such as an arm or knee.
3) IMMERSION

immersion is a technique in which the part to be treated is immersed in an ice solution. Unfortunately, it is only practical to immerse certain areas such as hands feet, and elbows.
- preparation
the solution is made up of 50 percent ice and 50 percent water placed in a suitable container. - application
the patient immerses the part in the solution and keeps it in either for a single ten-minute session.
4) ICE CUBE MASSAGE
ice cube massage is a useful method of application as it does not require an ice machine. the freezer compartment of a domestic refrigerator is sufficient.
preparation
a large block of ice, e.g. water frozen in a yoghurt pot, has one end wrapped in a towel, the other end is left free. the patient is adequately exposed to and supported
application
the exposed end of the ice block is massaged in a circular manner over the treatment area, applying only minimal pressure to the part. the maximum time of application is ten minutes. this application is useful in bed-sore, ice application is repeated three to four times in day.
Uses of Cold Therapy
Cold therapy is the “I” component of R.I.C.E. (rest, ice, compression, and elevation). This is a treatment recommended for the home care of many injuries, particularly ones caused by sports.
Cold therapy for pain relief may be used for:
1) Runner’s knee
2) Tendonitis
3) Sprains
4) Arthritis pain
5) Pain and swelling after a hip or knee replacement
6) To treat pain or swelling under a cast or a splint
CONTRAINDICATION
1) psychological
the thought of ice terrifies many patients, particularly the elderly. in fact many claim that their condition is made worse by the cold.
2) cardiac conditions
for 6 months after a myocardial infarct ice treatment should be avoided. the initial shock of the ice application may cause marked drop in blood pressure, thus causing an increase in heart rate may not be able to meet this demand.
the left shoulder and the heart the same sympathetic nerve supply and is has been shown that ice applied to the left shoulder can cause overflow of excitatory impulses to the heart via these sympathetic nerves. ice to the left shoulder should therefore be avoided in patient with any sort of cardiac disease.
3) peripheral nerve injury
blood vessels in the area supplied by a severed peripheral nerve lose their normal response to cooling. if such an area were cooled with ice, the net result would be that the part would get very cold and take many hours to regain a normal temperature.
4) vasospastic disease
the vasospasm in disease such as raynaud’s is made worse by the application of ice
5) peripheral vascular disease
as cold application many reduce an already inadequate blood supply, ice is avoided . however since the metabolic rate of the tissue is also lowered it is doubtful whether gangrene would ensue from cold treatment.
6) cold sensitivity
even if all precaution are taken there will still be a small number of patient who react adversely to ice. following the application of ice, these patient produce a local histamine -like urticaria which looks like a nettle rash and itches.
Benefits of applying ice include
- It lowers your skin temperature.
2. It reduces the nerve activity.
3. It reduces pain and swelling.
Experts believe that cold therapy can reduce swelling, which is tied to pain. It may also reduce sensitivity to pain. Cold therapy may be particularly effective when you are managing pain with swelling, especially around a joint or tendon.
How to apply cold therapy?
Putting ice or frozen items directly on your skin can ease pain, but it also can damage your skin. It’s best to wrap the cold object in a thin towel to protect your skin from the direct cold, especially if you are using gel packs from the freezer.
Apply the ice or gel pack for about 10 to 20 minutes several times a day. Check your skin often for sensation while using cold therapy. This will help make sure you aren’t damaging the tissues.
You might need to combine cold therapy with other approaches to pain management:
1) Rest. Take a break from activities that can make your pain worse.
2) Compression. Applying pressure to the area can help control swelling and pain. This also stabilizes the area so that you do not further injure yourself.
3) Elevation. Put your feet up, or elevate whatever body part is in pain.
4) Pain medicine. Over-the-counter products can help ease discomfort.
optimal ‘dosage of cryotherapy
- There is no optimal dosage that is ideal for all body locations. Consider the nature of the tissue when icing:
- The duration of icing for a small area with minimal fat and muscle, such as a finger, would be significantly less (~3‐5 minutes) than that for a larger area and deeper tissue such as at the hip (~20 minutes) Intermittent icing (e.g., 10 minutes on: 10 minutes off) may be more effective for management of acute inflammation than icing for 20 consecutive minutes
Type/duration of cooling dependent upon the goal
- Cooling to reduce pain will likely require less intense (ice pack) and shorter durations (5 minutes)
- Cooling to reduce metabolism of uninjured cells will likely require more intense cooling (ice bath or ice chips in a wet towel) for longer durations (10‐15 minutes)
- The hierarchy of the efficiency of cooling from most to least: ice‐water immersion, crushed ice, frozen peas and gel pack
Possible Risks/Undesirable Effects
- Inhibit muscle function
- Cooling can temporarily Inhibit muscle function with potential for increased risk of injury/re‐injury
- Be cautious when having patients weight bear/undertake complex exercise after icing a lower extremity
Ice burn
Elderly patients with impaired sensation and/or circulation will be more vulnerable to an ice‐burn, therefore consider using less intense icing techniques (e.g., moderately cold ice pack wrapped in an insulating layer of toweling)
Younger patients with intact sensation and circulation may benefit most from direct immersion of the limb in cold water then progressively adding ice cubes-Cold gel packs stored in a freezer have a surface temperature below 0°C (32°F) and thus an insulating layer should be used between the cold pack and the patient’s skin
Cryotherapy‐induced nerve injuries
Most common when cold is applied in combination with compression. Check capillary refill during application of ice combined with compression therapy to ensure adequate blood flow Generalized cooling and decrease in core temperature Shivering and piloerection are signs of decrease in core temperature which may compromise patient safety (especially in the elderly and those with fever) The application of therapeutic cryotherapy should produce only local effects.
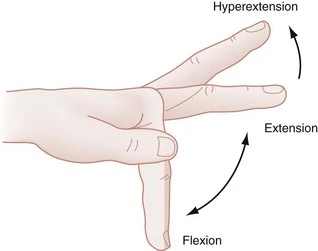
Reduced ROM
Ice may contribute to shortening of collagen fibers in connective tissue After gaining ROM by warming, stretching and then strengthening in the newest part of the ROM, it is likely .
counterproductive to cool the tissue in a shortened position.
If one wishes to cool the tissue post stretch and exercise, it is best to do so with the tissue in a lengthened position.
In patients with significantly restricted ROM due to scar tissue, it may be preferable not to use ice.
Be aware of conditions in which icing is contraindicated.
E.g. CRPS, hemoglobinuria, cryoglobinemia, Raynaud’s disease and cold uticaria.
Rehabilitation exercises.
Depending on where your injury is, you might want to try stretching and strengthening exercises that can support the area as recommended by your healthcare provider.
Stop applying ice if you lose feeling on the skin where you are applying it. If cold therapy doesn’t help your pain go away, contact your healthcare provider. Also, you may want to avoid cold therapy if you have certain medical conditions, like diabetes, that affect how well you can sense tissue damage.




Do you recommend using a damp towel between the joint being iced and the ice pack ? Thx.