Back surgery
Table of Contents
What is Back surgery?
Most pain in the lower back can be managed without surgery. In fact, surgery frequently does not relieve the pain; research suggests that 20 to 40 % of back surgeries are not successful. This lack of success is so usual that there is a medical term for it: failed back surgery syndrome.
Nonetheless, there are times when back surgery is a viable or required option to treat serious musculoskeletal injuries or nerve compression. A pain management specialist can help patients decide whether surgery is an appropriate choice after making sure they have exhausted all other options.
By the time they sign up for back surgery, the doctor will probably have tried a number of treatments to ease their back pain or lower body weakness. While there are no guarantees the operation will give relief, there are lots of options. Learn as much as they can about back surgery ahead of time. The more you know, the better the choice they will make.
There are so many questions to consider before attempting spine surgery. Is surgery required to treat the issue or would a non-surgical program be more appropriate? If surgery is required, is it good to have traditional spine surgery or minimally invasive spine surgery? What is minimally invasive spine surgery & how does it differ from traditional spine surgery?
back pain is a usual reason people consult the doctor, and in many cases, conservative treatment, including physical therapy & anti-inflammatory medications, can bring relief.
Nevertheless, spinal deformities, spinal infections, trauma, spine tumors, and some degenerative spine conditions, such as stenosis & herniated disks, might require surgical treatment. For the best result, it makes sense to consult a spine surgery team with plenty of experience.
The spine surgeon might opt for an open (traditional) spine surgery procedure, which involves an incision along the backbone. The surgeon moves muscle & soft tissue aside to gain access to the bones of the spine and the spinal cord.
Minimally invasive techniques include a smaller incision and the insertion of a tube, through which the surgeon inserts small surgical instruments to work on the spine. Minimally invasive techniques might be able to shorten recovery time & reduce the risk of complications.
Robotic spine surgery procedures can utilize GPS-like tracking systems to assist the spine surgeon in the extremely precise placement of screws & other hardware in the course of repairing a damaged or deformed spine.
How do you know when you need Back surgery?
When a patient comes to us with extremity symptoms, we almost always suggest they first get an evaluation by their primary care physician. If a patient is experiencing low back pain or neck pain, we will usually watch them over time & encourage them to maintain good, stable physical activity to see if the issue is resolved. If the issue is not resolved with physical activity, over-the-counter treatments, or pain management & anti-inflammatory medication, the next step would be to see a doctor for an evaluation.
Many patients with spine problems can be managed non-surgically. Physical therapy, home exercises, medication, & frequent times spinal injections are recommended prior to considering surgery. If the problem still is not resolved, then surgery becomes a better option.
For instance, if a patient has significant neurogenic pain in the extremities & non-surgical management has not been provided relief, surgical intervention is the best decision. For those with symptoms related to the spinal cord or nerve root compression, such as significant weakness in an arm or leg, or limb, we might recommend surgical intervention if non-surgical management was unsuccessful.
There are various procedures for spine-related back problems, but the 800-pound gorilla in the room during any discussion of back surgery is spinal fusion. In this technique, the surgeon joins two adjacent vertebrae (the large bones of the spine) to form a single unit.
Fusing an unstable joint is supposed to prevent movement that can cause pain, but it’s a major operation that often fails to offer a lasting solution. As a result, fusion has become the poster child for expensive, risky, & unnecessary back surgery. Despite that, the number of fusions has increased sharply over the years.
But men with aging spines should be cautious of fusion & its false promises. Based on the research, the indications for fusion are few & far between, but that does not halt surgeons from applying that or patients from getting that.
According to the National Institute of Arthritis & Musculoskeletal and Skin Diseases (NIAMS), part of the National Institutes of Health (NIH), the following conditions might be candidates for surgical treatment:
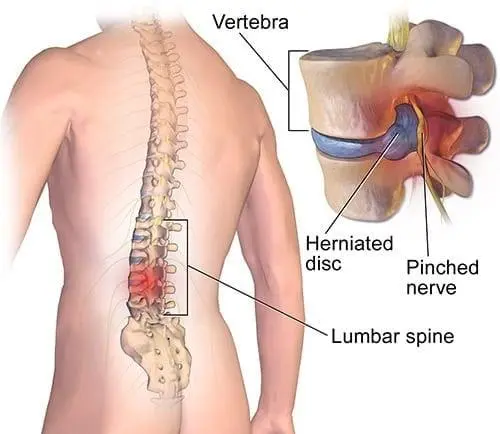
- Herniated or ruptured disks, in which one or more of the discs that cushion the bones of the spine are damaged
- Spinal stenosis is a narrowing of the spinal column that puts pressure on the spinal cord & nerves
- Spondylolisthesis, in which one or more bones in the spine move out of place
- Vertebral fractures caused by trauma to the bones in the spine or by osteoporosis
- Degenerative disc condition or damage to spinal discs as a person gets older
- In rare cases, back pain is caused by a tumor, an infection, or a nerve root issue called cauda equina syndrome. In these cases, NIAMS suggests surgery right away to ease the pain & prevent more problems.
What are the main differences between traditional spine surgery & minimally invasive Back surgery?
Traditional open spine surgery includes the complete exposure of the anatomy. In minimally invasive spine surgery we surgically expose less of the anatomy which means, in many cases, an earlier recovery in the first few weeks following surgery. In minimally invasive spine surgery, we frequently use additional surgical aids, such as intraoperative spinal navigation. This provides the surgeon with greater visibility into surgical regions with limited exposure.
Whether minimally invasive or traditional, the aims are the same for the long-term; we want to accomplish overall improvement in symptoms or a halt in degeneration. Ultimately, we want our procedures to outcome in less blood loss, shorter hospital stays, lower infection rates, & faster recovery in the weeks following surgery. Minimally invasive surgery typically results in an easier recovery process for patients, nevertheless, not every patient or surgical condition is appropriate for minimally invasive surgery. It is important that you partner with your spine surgeon to identify the best treatment choice for your condition.
Surgery is a controlled trauma. Therefore, we target to maximize the benefit for the patient while minimizing the trauma of surgery as much as possible. We implement leading surgical techniques & technology as appropriate, and our patients benefit from our surgeons’ academic research to further both minimally invasive & complex spine surgery procedures.
Some of the traditional spine surgery techniques include laminectomy, microdiscectomy, & traditional lumbar fusion. Laminectomy is a procedure that is utilized to treat spinal stenosis or pressure on the nerves of the low back. The surgery involves an incision on the back of the spine that allows the surgeon to remove bone spurs & thickened ligaments that are pressing on the nerves of the low back.
Microdiscectomy is utilized to treat nerve pain (sciatica) due to a herniated disc impinging a nerve in the spine. This surgery involves giving a small incision in the low back. The surgeon can then identify & remove the herniated disc that is impinging the nerve.
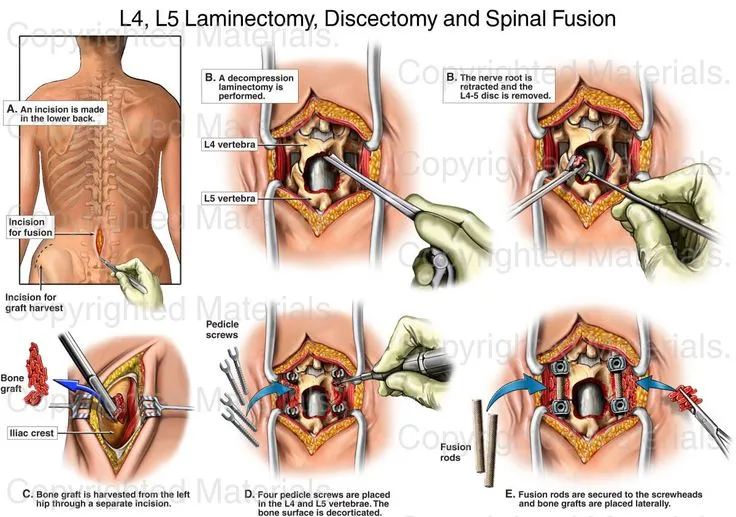
Traditional spinal fusions are utilized to treat instability of the spine, scoliosis, severe degeneration of the discs, or a combination of these issues. A fusion involves utilizing bone from the patient’s body to fuse one vertebra to another. Spinal instrumentation (pedicle screws) are placed into the vertebrae to stabilize the motion segment & assist with the fusion process.
A doctor will be able to tell which Minimally Invasive Spine surgeries if any, might be an option for treating a spinal condition. In some situations, Minimally Invasive Spine surgery might not be as safe or effective as traditional open surgery. If so, the doctor will be able to inform the patient about the relative risks & benefits. In addition, there are some conditions that are not truly manageable with Minimally Invasive Spine surgery.
In general, the goal of minimally invasive spine (MIS) surgery is to stabilize the vertebral bones & spinal joints and relieve the pressure being applied to the spinal nerves – often an outcome of conditions such as spinal instability, bone spurs, herniated discs, scoliosis or spinal tumors.
MIS Fusion Procedures:
- Minimally Invasive Lateral Interbody Fusion
- Minimally Invasive Posterior Lumbar Interbody Fusion (PLIF)
- Minimally Invasive Transforaminal Lumbar Interbody Fusion (TLIF)
- Minimally Invasive Posterior Thoracic Fusion
As opposed to open spine surgery, minimally invasive surgical approaches can be faster, safer, & need less recovery time. Because of the decreased trauma to the muscles & soft tissues (compared to open procedures), the potential benefits are:
- Faster recovery from surgery & less rehabilitation required
- Diminished reliance on pain medications after surgery
- Good cosmetic results from shorter skin incisions (sometimes as small as several millimeters)
- Less blood loss from surgery
- Decreased risk of muscle damage, since less or no splitting of the muscle, is needed
- Reduced risk of infection & postoperative pain
- In addition, some Faster recovery from surgery & less rehabilitation required
- Diminished reliance on pain medications after surgery surgeries are performed as outpatient procedures & utilize only local anesthesia – so there is less risk for an adverse reaction to general anesthesia.
What are the types of Back surgery
Vertebroplasty and kyphoplasty
These procedures are utilized to repair compression fractures of the vertebrae caused by osteoporosis. Both techniques include the injection of glue-like bone cement that hardens & strengthens the bone.
Spinal decompression
Spinal stenosis, which is a narrowing of the vertebral canal, is a common condition that can outcome in compression of the nerves. This can give a variety of symptoms, including pain, numbness, & muscle weakness. If surgery is recommended, it might be possible to remove the bone & soft tissues causing the nerve compression through an MIS approach using tubular dilators and a microscope or endoscope. The more common decompressive procedures include laminectomy & foraminotomy.
Laminectomy
This is the most usual surgery for lumbar spinal stenosis. In this procedure, a surgeon removes parts of the bone, bone spurs, or ligaments in the back. This relieves pressure on spinal nerves & can ease pain or weakness, but the procedure can make the spine less stable. If that happens, you’ll probably require a spinal fusion as well. Doctors sometimes do both procedures together.
Discectomy
Spinal discs are essentially elastic rings with soft material inside that act as cushions between the vertebral bones. If the elastic ring becomes weakened, the soft tissue inside can extrude or herniate outside of the elastic ring, press on a spinal nerve, & cause back pain. In a diskectomy, the surgeon removes the whole or part of the disc. They might have to make a big cut in the back, or they might be able to do it through a small one called a microdiscectomy. Microdiscectomy is performed with an operating microscope through a smaller incision to trim or remove the herniated disc, it might be possible to perform this procedure with minimally invasive surgery using tubular dilators & a microscope or endoscope than open discectomy & which has become the standard surgical procedure for lumbar disc herniation. Sometimes a discectomy is part of a bigger surgery that includes laminectomy, foraminotomy, or spinal fusion.
Spinal fusion
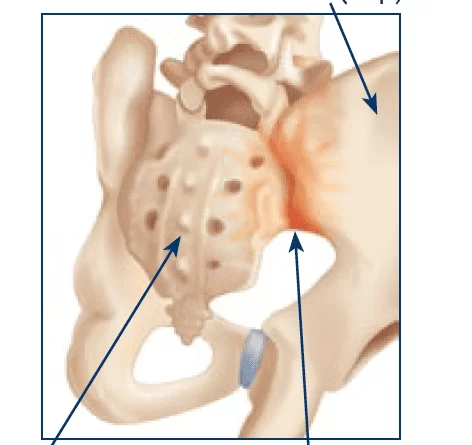
The surgeon removes the spinal disc between two or more vertebrae, then fuses the adjacent vertebrae utilizing bone grafts or metal devices secured by screws. Spinal fusion might result in some loss of flexibility in the spine & requires a long recovery period to allow the bone grafts to grow & fuse the vertebrae together. But it probably won’t limit daily activity. It is rare, but the bones do not always fuse completely. Smoking can make this complication more likely. If it happens, the patient may need another operation to fix it.
Foraminotomy
This surgery is utilized to relieve pain associated with a compressed nerve in the spine. The surgeon cuts away bone at the sides of vertebrae to widen the space where nerves exit your spine, the surgeon enlarges the bony hole where a nerve root exits the spinal canal to prevent bulging discs or joints thickened with age from pressure on the nerve. The extra room might relieve pressure on the nerves & ease your pain. Like a laminectomy, this procedure can also make the spine less stable. So the surgeon might do a spinal fusion at the same time. That’ll increase the amount of time the patient needs for recovery.
Nucleoplasty
Nucleoplasty is also called plasma disk decompression. This laser surgery utilizes radiofrequency energy to treat patients with low back pain associated with a mildly herniated disc. The surgeon inserts a needle in the disc. A plasma laser instrument is then inserted into the needle & the tip is heated, creating a field that vaporizes the tissue in the disc, reducing its size & relieving pressure on the nerves.
Disk replacement
A surgeon removes the damaged spinal disc & inserts an artificial one between your vertebrae that helps restore height & movement between the vertebrae. Unlike fusion, this lets the patient continue to move the spine. Recovery time might be smaller than for a spinal fusion, too. But there is a slight chance the new disc could slip or fall out of place & require repair. This is considered an alternative technique to spinal fusion for the treatment of patients with seriously damaged disks.
Transforaminal Lumbar Interbody Fusion (TLIF)
This is a minimally invasive spine technique that is performed for patients with refractory mechanical low back & radicular pain associated with spondylolisthesis, degenerative disc disease, & recurrent disc herniation. The procedure is performed from the back side (posterior) with the patient on his or her stomach. Utilizing two small incisions, screws & rods are placed between two or more vertebral levels. The intervertebral disc is removed & a cage filled with bone is placed in that void with the aim of stabilizing the levels affected.
Lateral Lumbar Interbody Fusion (LLIF)
Some of the most common minimally invasive spine procedures we perform are Lateral Lumbar Interbody Fusion (LLIF) Minimally Invasive Transforaminal Lumbar Interbody Fusion (MIS TLIF) & percutaneous instrumentation.
LLIF is a fusion during which the surgeon makes a small incision on the patient’s side, under their ribs to approach the spine from a lateral direction. This allows the surgeon to do a spinal fusion without disrupting the muscles of the spine.
The LLIF procedure might be accompanied by another procedure that is fairly usual, percutaneous instrumentation of the spine. In this procedure, the surgeon places rods & screws between the muscle fibers, frequently using computer navigation or intraoperative X-ray as opposed to removing the muscles from the spine as is done with traditional spinal fusion surgery. When possible, we pursue utilizing a minimally invasive approach, if it is an appropriate choice.
Interlaminar implant
This is a minimally invasive technique alternative to more invasive laminectomy or laminectomy plus fusion surgery. The surgeon implants a U-shaped instrument between two vertebrae in the lower back. It helps keep the gap between them open & eases pressure on spinal nerves. It can take place at the same time as a laminectomy. Unlike spinal fusion, the implant provides stability & lets you move your back almost like normal. You might not be able to bend backward as easily
in that area.
Some surgical treatments are not advocated by NINDS (National Institute of Neurological Disorders and Stroke), which cautions, for example, that intradiscal electrothermal therapy is “of questionable gain.” NINDS notes that radiofrequency denervation gives only temporary pain relief & that “evidence supporting this technique is limited.”
What are the risks of Back surgery?
Back surgery can carry more risks than some other types of surgery because it is done near the nervous system. The most serious of these risks involve paralysis & infections.
That said, any surgery has some degree of risk, including:
- Reaction to anesthesia or other drugs
- Bleeding
- Stroke
- Herniated disc
- Infection
- Blood clots, for instance in the legs or lungs
- Heart attack
- Nerve damage, which can cause weakness, paralysis, pain, sexual dysfunction, or loss of bowel or bladder control
The odds that something could go wrong go up for patients with certain health conditions. They also vary by type of surgery. Part of your surgeon’s job is to identify potential risks. So discuss it before you head to the operation.
Even with successful surgery, the recovery time can be longer. Depending on the type of surgery & your condition before the surgery, healing might take months. And you might lose some flexibility permanently.
Back surgery will almost always be done under general anesthesia. In addition to the usual risks associated with anesthesia, there are also risks associated with the patient lying face down on their stomach on the surgical table.
This position changes the patient’s body’s hemodynamics that is, how blood flows through the body. The position also limits the surgical doctor’s access to the patient’s airway. This needs extra care in the positioning of equipment, monitors, patient, & anesthesiologist. It is extremely important to have an anesthesiologist in the operating room to make sure everything is set up correctly & to be able to take immediate action in case anything goes wrong. An anesthesiologist is a doctor who specializes in anesthesia, critical care medicine, & pain management.
What are the benefits of Back surgery?
Frequently, the result is more than just a drop in pain. You may find:
- the patient can move around better.
- they’re more physically fit.
- their mood improves.
- they don’t need to take as much pain medicine.
- they can go back to work.
- they’re more productive at work.
How to do pain management during recovery from Back surgery?
Many options will involve medications such as opioids, nonsteroidal anti-inflammatory drugs, corticosteroids, & local anesthetics. Sometimes more than one drug can be taken. This multimodal therapy can improve pain control while limiting opioid usage.
Opioids should be used with care to avoid addiction & manage side effects, some of which can be life-threatening.
Alternative or complementary methods of pain relief that do not include medicines should also be discussed.
Anesthesiologists who specialize in pain management can work with you before & after surgery to develop a plan tailored to your condition, personal history, & preferences. They will consult with patients after surgery to determine what is working & what is not, and they will adjust their pain management treatment based on the level of pain they are experiencing.
FAQ (frequently asked questions)
Spinal decompression & fusion: It is the most usual spine surgery performed in the U.S., & it’s performed to take pressure off of “pinched” nerves & the spinal cord and to stabilize the spine.
In general, pain is generally the worst during the first one to three days following the surgery. After that, it should start to subside. the patient might feel some mild to moderate pain for up to six weeks after the surgery, but you should not feel severe pain.
Whenever surgery is done on the spine, there is some risk of injuring the spinal cord or the individual nerves. This can occur from instruments utilized during surgery, from swelling, or from scar formation following surgery. Damage to the spinal cord can cause paralysis in certain parts & not others.
A traditional spinal fusion surgery with general anesthesia takes about four hours & needs a hospital stay of three to four days as well as IV painkillers. The awake spine surgery takes half the time & significantly has patients out of the hospital within 24 hours.
No, there is no hard & fast age limit for spinal surgery. Because both elderly patients and young patients can be afflicted with spinal issues, age is not the primary deciding factor in whether or not spinal surgery is an option.
The average fee for back Surgery in India is INR Rs. 2,30,000. The maximum amount to be paid for back Surgery in India is up to INR Rs. 5,50,000.
The success rate of spinal fusion surgery Concerning pain relief is 70 to 80 percent.





One Comment