Facet Arthropathy
Table of Contents
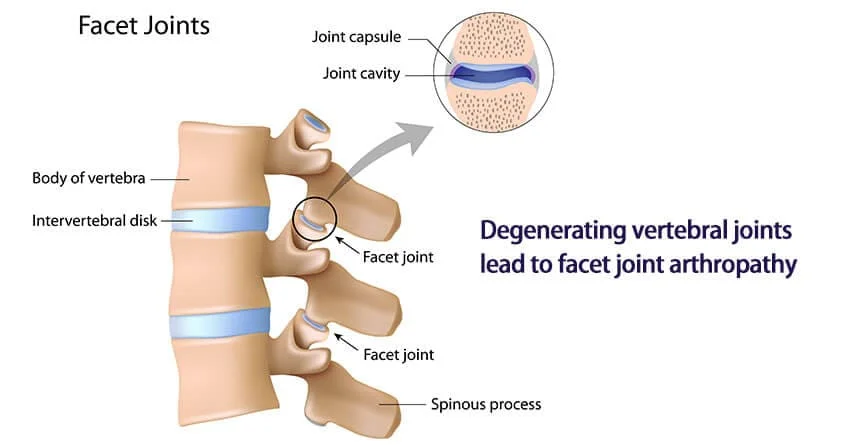
What is a Facet Arthropathy?
Facet Arthropathy (FA) is a painful and arthritic condition of the facet joints. It is a degenerative condition that affects the spine. These joints allow movement of bending, twisting, and alignment of the spine. The pain occurs when the facet joints wear down and pressure generates on the spinal cord.
The spine is made up of the vertebrae which run along the spinal column. The spinal nerves come into the spinal cord between the vertebra and the facet joints. Between each vertebrae two facet joints are present. In a normal spine, the spinal disc and the facet joints support each other for correct and safe movement.
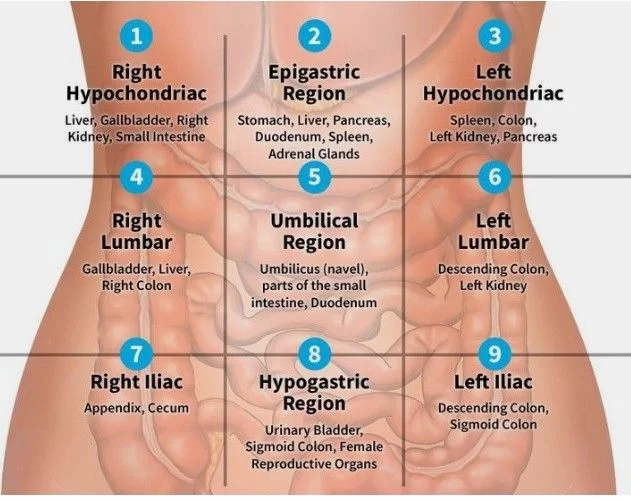
Facet Arthropathy is associated with chronic low back pain. Potential causes of low back pain include abnormalities in the ligaments that connect the muscles to the spinal discs, compression or pinching of the spinal cord roots, and protective covering of the spinal cord known as the dura and muscle. Disorders of the lower spine and facet joints result in low back pain due to the defects of the ligaments, spinal discs or muscles, and spinal nerve compression. It is the most common effect in older adults and those with high body mass index (BMI). Individuals may seek immediate medical treatment as this condition can negatively affect their quality of life.
Anatomy of Facet Joint:
The facet joints are the affected anatomy in this disorder. The posterolateral articulations are formed by the lumbar facet joints. This is accomplished by the attachment of one vertebra’s vertebral arch to the arch of the next vertebra. They are properly named the zygapophyseal joints.
Each facet joint includes a joint gape, in between 1 and 1.5 ml of fluid present, a synovial membrane, hyaline cartilage surfaces, and a fibrous capsule (1mm). Each level of the spine has a three-joint complex to give the joint functions. There are two facet joints in the posteriorly and a large disc in the anteriorly. It provides stability to the spine.
In the case of lumbar facet arthropathy, the joints get inflamed due to high compressive forces so the pain is present in this area.
Causes of the Facet Arthropathy
- Widespread arthritis of other joints like Ankylosing Spondylitis, Psoriatic Arthritis, and Rheumatoid Arthritis affected the facet joints resulting in facet arthropathy.
- Trauma such as undiagnosed fractures, disc tears, cartilage splitting, or hemorrhage in the lumber area can get some symptoms The synovial capsule may become distended and inflamed which puts pressure on the spinal nerves. Facet joint discomfort causes lower back pain when degenerative arthritis and joint instability are present.
- Rheumatoid arthritis is also damage to facets commonly the mid-lumbar and lower lumbar areas.
- Aging is the indirect cause of this condition.
- Osteoarthritis is the degeneration of joint cartilage and bone, with pain present in the affected area.
- Synovial cyst is affected when the fluid-filled sac develops in the spine, it is seen in aging.
- Low Back Pain (LBP) is a major cause of disability and the pain affects a person’s daily living activities. LBP is the most common musculoskeletal disorder in society and it is seen in persons of any age. Work-related injuries are the primary cause of LBP.
The prevalence of low back pain is 60-70% in industrialized countries. The most relevant cause of mechanical low back pain is lumbosacral facet joint discomfort, which affects 15-45% of individuals with persistent LBP. Facet joint syndrome is commonly seen in patients with chronic low back pain.
Symptoms of Facet Arthropathy
Pain: Pain is the most common symptom of facet arthropathy. It is the following:
Pain that is worse during sleep or rest. It is a dull aching type of pain on both sides of the spine.
Lower back pain that worsens when twisting, backward bending, and standing. Pain relieves in forward bending and when the pressure decreases on the facet joint.
Pain in one specific location of the spine.
A dull discomfort on one or both lower back sides.
Facet arthropathy pain, unlike sciatica or a slipped disc, does not usually spread down the legs.
the development of other diseases such as spinal stenosis and bone spurs.
Pins-and-needles sensations in the hands or feet.
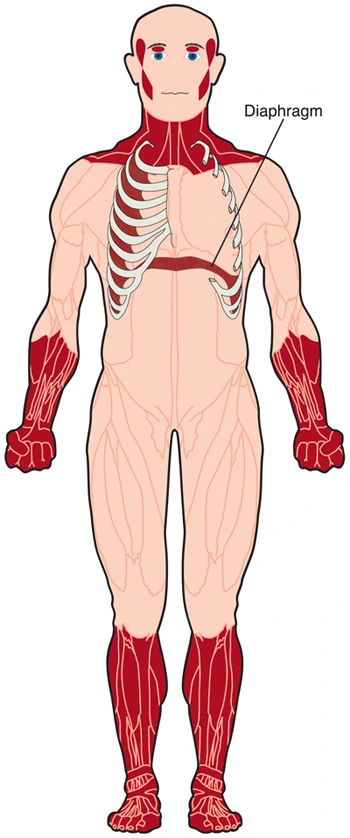
Muscle spasms or cramps.
Muscle weakness.
How is Facet Arthropathy Diagnosed?
First of doctor takes a patient history and physical examination. Check, MRI, CT scan, or X-ray, to identify the involvement area and degeneration of the spine. Injection of anti-inflammatory steroids injection given into the facet joints can also assist the confirming the diagnosis. If symptoms are reduced after the injection, then it is confirmed that the individual has facet arthropathy.
Physical examination
In the physical examination tenderness and palpation are present in the lumbar at the paravertebral region over the transverse processes and paraspinal muscles. Pain may increase in the spinal extension and rotation.
Check the neurological findings, like lower limb sensation, muscle strength, and deep tendon reflexes. The lower limb strength may be decreased because of pain.
The Kemp test (also known as the quadrant test and the extension-rotation test) is a provocative examination used to identify facet joint pain. In this test, a patient performs extension and rotation combined movement of the spine, if the pain is produced during this movement the test is positive.
Examine paraspinal muscular fullness or asymmetry, lumbar lordosis increase or reduction, muscle atrophy, or postural asymmetry.
If a patient has chronic facet arthropathy resulting in the flattening of the lumbar lordosis and rotation or lateral bending at the sacroiliac joint and the thoracolumbar area.
Tenderness is present over the facet joint. In some cases, facet joint pain may radiate to the gluteal or posterior thigh area.
Range of motion:
Range of motion should be checked to lumber flexion, extension, lateral bending, and rotation. Pain is increased while a patient is in standing, extension, flexion, or the (axial)rotation position of the lumbar spine and it may be radiating. Also, the pain increased during sitting and sitting-to-stand activity.
Flexibility:
The inflexibility of the pelvic muscles can directly affect the mechanics of the lumbosacral spine. The doctor may discover an abnormality with facet joint pathology, an abnormal pelvic tilt, and rotation of the hip.
Sensory examination:
Check the deep sensation and superficial sensation over the affected area. Sensations are normal in this condition but in other pathology of the spine, the sensations are altered.
Muscle stretch reflexes:
Muscle stretch reflex is normal in facet joint–mediated LBP patients. In other pathology nerve root impingement is present.
Muscle strength:
Manual Muscle Testing is important to check whether weakness is present and whether the distribution of weakness corresponds to a single root, multiple roots, or a peripheral nerve root or plexus. Also, checking the functional core strength is important to identify other abnormalities.
Straight leg–raise test:
While performing the straight leg raise test, patients don’t feel pain. However, if facet joint hypertrophy or a synovial cyst in the intervertebral foramen, causes nerve root impingement, this condition may produce pain.
Posture Analysis, ADL, and technique: Observe the activity that may have started the problem. Examination of dynamic and static postures that may have caused or contributed to your current back problem. A review of the things you do at work and at home right now that could or might not be affecting or worsening your current health.
Differential diagnosis
- Herniated disc
- Rheumatoid arthritis
- Psoriatic arthritis
- Reactive arthritis
- Spinal gout
- Discogenic pain syndrome
- Lumbosacral radiculopathy
- Piriformis syndrome
- Paraspinal muscle/ligament sprain/strain
- Lumbar spondylosis/spondylolysis/spondylolisthesis
- Diffuse idiopathic skeletal hyperostosis
- Sacroiliac joint dysfunction
- Thoracolumbar fascia dysfunction
- Infection
- Neoplasm
- Fibromyalgia
Risk factors of Facet Arthropathy
Age: This condition is more common in older people.
Sex: Women are more affected compared to men.
Ethnicity: African Americans are less likely to develop this condition.
Body weight: Persons with a BMI of 25-30 are three times more likely to develop lumbar facet arthropathy, while persons with a BMI of 30-35 are five times more likely to get it.
Heredity: Some people had facet arthropathy due to their genetics or have any family history of the condition. Facet arthropathy can result from the collapse or degeneration of discs in the back, which may be inherited.
Osteoarthritis may occur the facet arthropathy. Osteoarthritis affects the hip or knee also sometimes it’s hereditary.
Treatment of Facet arthropathy
Treatment options for the discomfort and signs brought on by facet arthropathy include the following:
Medications:
Medicines like NSAIDs, Aspirin, Ibuprofen, Naproxen, and Toradol are given to reduce pain.
Physical therapy, strengthening exercises, avoiding the movements that aggravate the symptoms like twisting, lifting, or lower back extension.
Intra-joint injections and medial branch blocks of steroids under radiographic guidance and radiofrequency (RF) ablation to block the sensation of pain are two standard therapies. Reduce the complication rates in both treatments.
With improved long-term outcomes, shockwave therapy is superior to steroid injections and equally efficacious to RF ablation.
Stem Cell Regeneration:
A non-invasive and experimental treatment for painful and injured facet joints is stem cell regeneration. Patients have experienced success with focused stem cell therapies for the facet joint or hip and knee joints for many years. An orthopedic doctor will carefully inject stem cells during treatment into the facet joints with the aid of CT imaging guidance. The cells begin to work on joint repair and regeneration in response to inflammatory signals from the arthritic joint. Shockwave therapy, which was described previously, and other supportive therapies can help with this
Spine Surgery:
If patients are not relieved of the symptoms by conservative therapies, surgery may be required to relieve the pain of facet arthropathy – in conditions like nerve compression, spinal stenosis, spinal instability, and associated motor or sensory symptoms.
Disc Replacement is an option for mild to moderate Facet Arthropathy that is associated with a degenerative spinal disc at the same level. Disc Replacement is an option for In certain types of spinal fusion, the surgeon eliminates the facet joints between the levels of the spine that are to be fused together, thus removing the facet joints.
The facet joints are no longer a cause of future problems.
Physiotherapy treatment:
Physical therapy and core strengthening exercises can help to strengthen the spine while also reducing stress on the facet joints. The following is the primary focus of therapy for acute facet joint pain:
Educate the patient:
Educate the patient about the impairments, and pain types. Understanding the condition and therapy. The therapist gives advice about the patient’s posture and correction of the daily activities.
Relative rest:
The patient doesn’t take a full rest. They can do an activity as possible. The patient is encouraged to limit activity once a day when the symptoms are more painful. The patient should not be completely inactive. The therapist told to the patient to do an activity or movement as soon as possible.
Reducing lumbar lordosis:
It is important to decrease lumbar lordosis with exercise because, in lumber lordosis, the weight is directly on the posterior aspect of the spine and the z-joints. To do this, the patient should be taught pelvic motions to lower lumbar lordosis. These pelvic tilt exercises can be performed in different positions like sitting, or standing with knees bent or straight legs.
Pain relief:
Combination treatment like spinal manipulative therapy (SMT) combined with trunk strengthening exercises (TSE) or SMT combined with trunk stretching exercises. Non-steroidal anti-inflammatory drug (NSAID) for reducing pain. During 11 weeks they examined the patient’s pain rating for low back pain, disability, and functional status of health. Spinal manipulation therapy is used for both short- and long-term pain relief.
Exercises:
Primary treatments for facet joint syndrome are heat, cryotherapy, and mobilizations. These techniques give to relaxing effect on the muscles.
When the pain is reduced stretching and strengthening exercises can be initiated. Stretching can help to restore standard mechanics to the lumbar spine and pelvis. Stretching is given to the hamstrings, quadriceps, hip abductors, gluteals, and abdominals muscles.
In the rehabilitation phase, eccentric muscle strengthening exercises and dynamic exercises are done. All exercises were performed in the treatment under the supervision of a physical therapist with proper knowledge. The therapist placed each patient in the optimal position to produce proper posture and muscular contraction. The main focus of exercise therapy should be on stabilization therapy.
Mechanical traction to help decompress the spine.

Knee-to-chest exercise: Teach the patient to bend your knees to the chest and hold for 30 to 60 seconds.
Aquatic therapy: To alleviate pressure on the spine during exercise.
Advise the patient to walk for 10 to 20 minutes per day.
Graded exercises: A graded emphasizes stabilizing exercises for patients with nonspecific LBP to improve disability and Physical health.
Heat and cold therapy: Heat and cold therapy are recommended by the therapist to reduce the pain. If the patient has low back and is in a chronic stage advise the heat pack in periodically. If the pain is in an acute manner then ice application is suggested.
Therapeutic massage: Massage therapy is effective in providing short-term improvement of sub-acute and chronic LBP symptoms.
Balneotherapy: Has positive effects in reducing pain and improving function, on the patient’s quality of life, as well as on their analgesic and NSAID requirements. Combined with exercise therapy with physical modalities plus exercise in improving quality of life and flexibility of patients with chronic low back pain.
Shockwave diathermy: Shockwave therapy is a type of heating treatment that affects pain reduction.
Spinal mobilization: Suggest to the non-specific LBP patients should take a 12-week session of manual therapy including spinal manipulation.
Aerobic exercise: slow walking, stationary cycling, Elliptical machine can be used.
Stretching exercises: Hip flexors stretch, Cat/Camel exercise, Child’s pose, Foam Rolling, Pelvic tilt lying on the floor.
Prognosis:
Facet arthropathy worsens with age, and the first line of treatment is conservative treatment like physiotherapy. Patients who do not react to a trial of physical therapy may have the facet joint diagnostically blocked. Radiofrequency neurotomy has been shown to reduce pain for 6 months to 1 year, after which a repeat treatment may be necessary.
Most facet disorders resolve without surgery and allow patients to resume regular activities. Depending on the severity of the symptoms, therapy might last anywhere from 4 to 12 weeks. The therapist did the stretching, strengthening, and stabilization exercises for the patients. Proper mechanics, posture, body mechanics, and knowledge of the dos and don’ts for a healthy back are required.
Prevention:
Prevention is the best part of avoiding any type of worsening condition and lifelong activity restriction. Preventative measures are the following:
- Maintain a healthy body weight.
- Do exercise regularly.
- Avoid injury to the spine.
- Wear protective gear while participating in sports.
- Maintaining a good posture while you sit, walk, and stand activity.
- Take bone-supporting supplements like vitamin D and calcium. Always supplement use with your doctor’s advice.
Once damaged, the facet joints. This doesn’t mean there is no chance for recovery, it can be healed with proper treatment. With the help of a healthcare professional who can give a proper treatment plan.
FAQ:
Is facet arthropathy serious?
Over time, facet arthropathy can lead to complications, like osteophytes (i.e., bone spurs), which are small bony projections that narrow the spaces in the spine available for the passage of nerve roots, thereby causing spinal stenosis and potentially neuropathic pain.
What is the best treatment for facet arthropathy?
The treatment includes over-the-counter pain relievers such as anti-inflammatories or acetaminophen. It is possible to apply topical remedies like heat or ice. Physical therapy is often recommended and includes a focus on postural correction, stretching, and strengthening.
What exercises should be avoided with facet arthropathy?
Jogging and other high-impact workouts like high-impact aerobics can exert strain on a disc and aggravate an existing injury. Avoid twisting motions as well, such as playing golf, as these might exacerbate back pain.
What are the best exercises for lumbar facet arthropathy?
Knee to chest: Lye on your back. …
Posterior pelvic tilt: lay on your back with your feet flat on the ground, knees bent, and back upward.
Walking.