Triangular Fibrocartilage Complex Injury
Table of Contents
What is Triangular Fibrocartilage Complex Injury?
Triangular Fibrocartilage Complex (TFCC) injuries refer to a spectrum of conditions that affect the intricate network of tissues situated within the wrist joint. This complex anatomical structure, composed of ligaments, cartilage, and tendons, plays a vital role in maintaining wrist stability and facilitating smooth forearm movement. Situated on the ulnar side of the wrist, the TFCC bridges the gap between the ulna and the carpal bones, providing support to the joint and contributing to its overall functionality.
TFCC injuries can arise from a variety of causes, including traumatic incidents such as falls on an outstretched hand, forceful twisting motions, or direct impacts to the wrist. They can also develop gradually due to repetitive stress and degeneration over time. Athletes, particularly those engaged in sports that involve repetitive wrist movements or weight-bearing activities, as well as individuals in occupations that demand significant wrist use, are at an increased risk of TFCC injuries.
Description
The triangular fibrocartilage complex (TFCC) is a level of arrangement in the wrist, involving ligaments, cartilage, and tendons, that provide stability and support. TFCC injuries can range from tears to strains, often causing wrist pain, instability, and limited range of motion.
They can result from trauma or gradual wear and tear, and treatment may involve rest, splinting, physical therapy, or in some cases, surgery. It’s essential to consult a medical professional to properly diagnose and manage TFCC injuries.
Clinically relevant anatomy
Triangular fibrocartilage complex (TFCC) injuries involve structures within the wrist that play a crucial role in its stability and function. The TFCC is located on the ulnar side (pinky side) of the wrist and consists of the following clinically relevant components:
Triangular Fibrocartilage: This is a specialized cartilage that spans the gap between the ulna (one of the forearm bones) and the carpal bones of the wrist. It helps distribute forces and absorb shock.
Ulnar Collateral Ligament (UCL): This ligament connects the ulna to the carpal bones and provides stability to the wrist joint.
Ulnar Carpal Ligaments: Ligaments that connect the ulna to specific carpal bones, contribute to the TFCC’s overall stability.
Articular Disc: A fibrous structure that acts as a cushion between the ulna and carpal bones, facilitating smooth movement and shock absorption.
The sheath of the Extensor Carpi Ulnaris (ECU): The ECU tendon wraps around the ulna and passes through the TFCC, allowing wrist movement.
Meniscus Homologue: This structure is similar to the meniscus found in the knee joint and provides additional stability and support to the TFCC.
TFCC injuries can involve tears or damage to any of these components, leading to wrist pain, instability, and impaired function. Diagnosis often involves physical examination, imaging (such as MRI), and sometimes arthroscopy to visualize and treat the injury directly. Proper evaluation and management by a healthcare professional are essential for TFCC injury diagnosis and treatment.
Causes of triangular fibrocartilage complex injuries
Triangular fibrocartilage complex (TFCC) injuries can occur due to various causes. The etiology (causes) of TFCC injuries include:
Trauma: Sudden forceful impacts or accidents, such as falls onto an outstretched hand, can lead to TFCC injuries. Direct trauma to the wrist can cause tears or strains in the TFCC components.
Repetitive Strain: Overuse or repetitive motions of the wrist, such as those involved in certain sports (e.g., racket sports) or occupational activities can contribute to TFCC injuries over time.
Wrist Fractures: Fractures of the distal radius or ulna bones can indirectly impact the TFCC, leading to injuries. The bones’ misalignment can stress the TFCC or disrupt its normal function.
Aging and Degeneration: As a part of natural aging or due to wear and tear over time, the TFCC can degenerate, becoming more susceptible to injury.
Ulnar Impaction Syndrome: This occurs when the ulna bone is relatively longer than the radius, causing it to impact the TFCC during wrist movements. Over time, this can lead to TFCC injuries.
Instability of the Distal Radioulnar Joint (DRUJ): If the DRUJ, where the radius and ulna meet, becomes unstable, it can place additional stress on the TFCC and increase the risk of injuries.
Sports Injuries: Activities that involve forceful gripping, twisting, or weight-bearing on the wrist, such as gymnastics, can increase the risk of TFCC injuries.
Occupational Factors: Certain professions that involve repetitive wrist movements, vibration exposure, or manual labor can contribute to TFCC injuries.
Inflammatory Conditions: Chronic inflammatory conditions like rheumatoid arthritis or gout can affect the TFCC and increase the risk of injury.
Congenital Factors: Anatomical variations or congenital conditions that affect the wrist’s structure and stability can predispose individuals to TFCC injuries.
Understanding the underlying cause of a TFCC injury is crucial for proper diagnosis and treatment. Consultation with a healthcare professional, often an orthopedic specialist or hand surgeon, is recommended for accurate evaluation and appropriate management.
Symptoms of triangular fibrocartilage complex injuries
Triangular fibrocartilage complex (TFCC) injuries can manifest with a range of symptoms that may vary in severity. Common symptoms of TFCC injuries include:
Wrist Pain: Pain is a hallmark symptom of TFCC injuries. The pain is often localized to the ulnar (pinky) side of the wrist and may worsen with gripping, twisting, or weight-bearing activities.
Swelling: Inflammation and fluid accumulation within the TFCC can lead to swelling around the wrist joint.
Weakness and Instability: TFCC injuries can result in a feeling of weakness or instability in the wrist, making it challenging to perform certain tasks or activities that require wrist movement.
Limited Range of Motion: Reduced flexibility and limited movement of the wrist, especially during movements that involve rotation can be indicative of a TFCC injury.
Crepitus: Some individuals may experience a grinding or popping sensation (crepitus) when moving the wrist, particularly when rotating it.
Painful Grasping or Gripping: Activities that involve gripping or grasping objects may exacerbate wrist pain in individuals with TFCC injuries.
Pain with Weight-Bearing: Putting weight on the affected wrist, such as during push-ups or weightlifting, can elicit pain.
Painful Wrist Twisting: Twisting the wrist, such as when turning a doorknob or opening a jar, can be particularly painful.
Pain with Ulnar Deviation: Moving the wrist laterally (towards the pinky side) may trigger discomfort and pain.
Painful Activities: Activities that involve repetitive movements of the wrist, like typing, playing musical instruments, or certain sports, can worsen pain and discomfort.
Tenderness: The ulnar side of the wrist may be tender to touch, and pressure applied to this area can provoke pain.
- It’s important to note that the severity and combination of symptoms can vary based on the specific type and extent of the TFCC injury.
- If you suspect a TFCC injury or experience persistent wrist pain and discomfort, it’s advisable to consult a healthcare professional for proper evaluation, diagnosis, and appropriate treatment.
Pathology of triangular fibrocartilage complex injuries
The pathology of triangular fibrocartilage complex (TFCC) injuries involves various structural changes and disruptions within the TFCC can result from trauma or degeneration. Common pathologies associated with TFCC injuries include:
Tears: TFCC tears can occur in different parts of the complex, such as the triangular fibrocartilage itself, the ulnar collateral ligament, or the meniscus homolog. Tears can range from small partial tears to complete ruptures, affecting the stability and function of the wrist.
Degeneration: Over time, the TFCC can undergo degenerative changes, leading to thinning, fraying, and weakening of its components. Degeneration may be accelerated by repetitive use, aging, or underlying conditions like arthritis.
Vascular Changes: Injuries to the TFCC can disrupt its blood supply, impairing its ability to heal. This can lead to delayed recovery and increased vulnerability to further damage.
Instability: TFCC injuries can result in instability of the distal radioulnar joint (DRUJ), where the radius and ulna meet. Instability can contribute to pain, limited range of motion, and difficulty in performing daily activities.
Ulnar Impaction Syndrome: TFCC injuries can lead to ulnar impaction syndrome, where the ulna bone impacts the TFCC during wrist movements. This can cause further wear and tear, contributing to pain and dysfunction.
Inflammation: Injury to the TFCC can trigger an inflammatory response, leading to pain, swelling, and discomfort in the wrist.
Secondary Effects: TFCC injuries can result in altered wrist mechanics, affecting adjacent structures and joints, such as the carpal bones, radius, and ulna.
Complications: If left untreated or improperly managed, TFCC injuries can lead to chronic pain, limited wrist function, and the development of secondary conditions like wrist arthritis.
- Diagnosing the specific pathology of a TFCC injury often requires imaging techniques such as magnetic resonance imaging (MRI) or arthroscopy to visualize the extent of the damage.
- Treatment strategies will depend on the severity and nature of the pathology and may involve conservative measures (rest, splinting, physical therapy) or surgical intervention to repair or reconstruct the TFCC.
- It’s important to seek medical attention for accurate diagnosis and appropriate management of TFCC injuries.
Differential diagnosis
Several conditions can present with symptoms similar to triangular fibrocartilage complex (TFCC) injuries. A proper differential diagnosis helps healthcare professionals distinguish between different possible causes of wrist pain and identify the most appropriate treatment. Some conditions to consider in the differential diagnosis of TFCC injuries include:
Wrist Sprain or Strain: Ligament or tendon injuries in the wrist can lead to pain and limited mobility similar to TFCC injuries.
Carpal Tunnel Syndrome: Compression of the median nerve at the wrist can cause pain, tingling, and numbness in the hand, often affecting the thumb, index, middle, and ring fingers.
De Quervain’s Tenosynovitis: Inflammation of the tendons on the thumb side of the wrist can result in pain and limited movement, especially during thumb extension and abduction.
Scaphoid Fracture: A fracture of the scaphoid bone can cause pain, tenderness, and limited range of motion in the wrist, often aggravated by gripping.
Ulnar Collateral Ligament (UCL) Injury: Similar to TFCC injuries, UCL injuries on the ulnar side of the wrist can lead to pain and instability.
Ganglion Cyst: A fluid-filled sac that can develop on the wrist joint, causing swelling and discomfort.
Kienböck’s Disease: Avascular necrosis of the lunate bone in the wrist, leading to pain and limited wrist movement.
Osteoarthritis or Rheumatoid Arthritis: These conditions can affect the wrist joints and lead to pain, stiffness, and reduced function.
Intersection Syndrome: Inflammation of the tendons on the back of the forearm can cause pain near the wrist joint.
Radial Tunnel Syndrome: Compression of the radial nerve can result in pain and discomfort on the back of the forearm and wrist.
Tendinitis: Inflammation of tendons in the wrist can cause pain and limited movement.
Fractures of Other Wrist Bones: Fractures of other carpal or metacarpal bones can lead to wrist pain and dysfunction.
Lunotriquetral Ligament Injury: Damage to this ligament can result in ulnar-sided wrist pain and instability.
Properly diagnosing a TFCC injury involves a comprehensive evaluation, including a thorough medical history, physical examination, and often imaging studies such as X-rays or MRI. If you’re experiencing wrist pain or discomfort, it’s important to seek medical attention for an accurate diagnosis and appropriate treatment.
Diagnosis
Physical ExaminationTFCC Stress Test
- On examination, palpation of the TFCC is best with the wrist in pronation.
- It is in the middle of the flexor carpi ulnaris, ulnar styloid, and os pisiform.
- Several physical exam tests may suggest the diagnosis of TFCC injury.
- These contain:
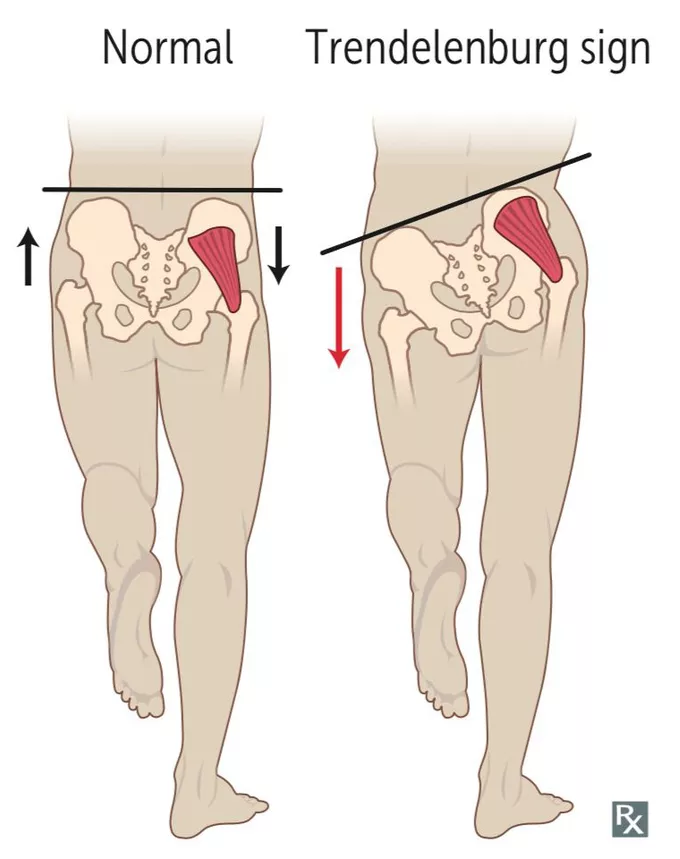
TFCC compression test: forearm in the neutral position with ulnar deviation produces symptoms
TFCC stress test: using a force across the ulna with the wrist in ulnar deviation produces symptoms
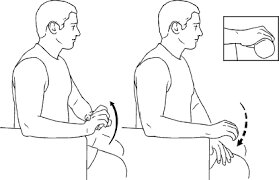
Press test: individuals lift themselves out of a chair utilizing their wrists in an extended position. Pain shows a positive test.
Supination test: The individual grabs the underside of a tableland with the forearms supinated; this causes a limitation on the TFCC and dorsal impingement, which will generate pain if there is a peripheral, dorsal tear.
Piano key test: Put hands on an examination table and push the palms on the table. If the distal ulna is prominent on the involved side, this means distal radioulnar joint instability which may have associations with TFCC injury. If the palms are comfortable and the ulnar head goes around to regular placement, this is a positive test
Grind test: Squeeze the radius and ulna and have the individual rotate the forearm. Pain could indicate a degenerative process.
Diagnostic Imaging
Radiographs: They may show avulsion of the ulnar styloid, scaphoid fracture, distal radial fracture, the volar tilt of lunate or triquetrum; ulnar variance.
Triple Injection Arthrography: label of tear (low specificity).
MRI: identification of tears (high sensitivity and specificity).
Outcome Measures
- DASH Outcome Measure
- Modified Mayo Wrist Score
- Activities of Daily Living Score
Treatment of triangular fibrocartilage complex injuries
Conservative Treatment
The rehabilitation program should involve rest, activity modification to clear the inciting force of injury, ice application, and splint immobilization for 3 to 6 weeks after the immobilization, the patient should receive physical therapy
Surgical Intervention
Surgical possibilities should be considered if traditional medicine fails or if there is DRUJ instability. Surgical therapy will rely on the Palmer classification of the injury,
The Palmer classification is the most identified plan for TFCC lesions- It separates them into these two categories (with subdivisions, beyond the scope of this article):
Traumatic and Degenerative.-This classification supplies an exact anatomic explanation of tears, it does not guide treatment or indicate prognosis
A debridement – It is a surgical option that causes bleeding to stimulate healing. Debridement has advantageous results for central TFCC tears but has been shown to have more threatening results in degenerative tears or patients with higher positive ulnar variance.
Physiotherapy treatment of triangular fibrocartilage complex injuries
- Primary treatment includes rest, physical therapy, and corticosteroid injections.
- The period to attempt conservative therapy before advancing to surgical options varies.
- Six months of conservative treatment is proper if there is no DRUJ (distal radioulnar joint) instability.
Post-Operative Rehabilitation
Recovery after surgery varies, but generally, 4 to 6 weeks should be predicted for arthroscopy and roughly 3 months for an open approach. Individuals will undergo physical therapy after the procedure. The identical time to start physical therapy and the length of physical therapy relies on the type of surgery performed and the surgeon’s preference.
For type 1 injuries
- The wrist will be immobilized for 1 week after the arthroscopy.
- After 1 week, range of motion exercises may be initiated.
- Golf participants and tennis participants who sorrow from a stable TFCC tear may begin light exercise ball contact at 3 weeks after the arthroscopy.
- They may return to their normal sports activity in 4 to 6 weeks. When the symptoms stay, ulnocarpal corticosteroid injection may be an option.
- For more painful damages, post-operative immobilization in a Muenster cast for 4 weeks may be considered.
Basic range of motion exercise
Please note that these exercises are just a starting point and should only be performed under the guidance of a qualified healthcare professional. Range of motion exercises for triangular fibrocartilage complex (TFCC) injuries may include:
Wrist Flexion and Extension:
Wrist Flexion: Slowly bend the wrist forward, bringing the palm towards the forearm. Hold for some seconds and then release.
Wrist Extension: Slowly bend the wrist backward, pointing the fingers toward the ceiling. Keep briefly and then relax.
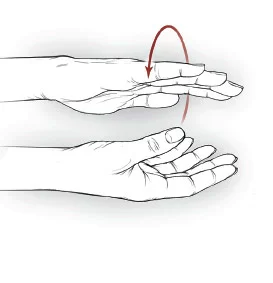
Wrist Supination and Pronation:
Wrist Supination: Rotate the forearm and palm upward as if you’re holding a bowl of soup.
Wrist Pronation: Rotate the forearm and palm downward as if you’re pouring out the bowl of soup.
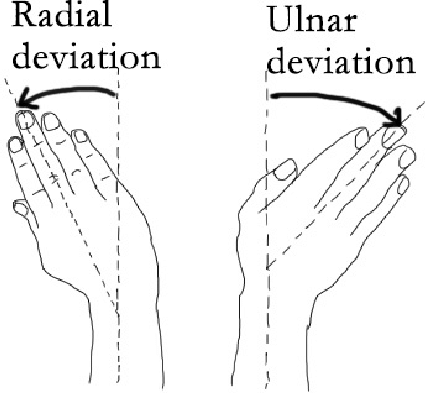
Ulnar Deviation and Radial Deviation:
Ulnar Deviation: Slowly tilt the wrist and hand towards the pinky side.
Radial Deviation: Slowly tilt the wrist and hand towards the thumb side.
Passive Range of Motion (PROM) Exercises:
Use a different hand to gently move the injured wrist through its range of motion, being careful not to force any activity that causes pain. Recognize, these exercises should be performed within a pain-free range and should not exacerbate symptoms. If a person experiences improved pain or discomfort, stop the exercises and consult the healthcare provider. A physiotherapist may guide you through a tailored exercise program that suits the specific TFCC injury and recovery needs.
After 4 weeks:
- The wrist is put in a short arm splint or Versa wrist splint, which permits a progressive motion to the wrist.
- The immobilization will lower wrist pain and aggravation, which could enhance healing.
- Some kinds of splints will help stabilize the wrist, which will lead to an advancement in hand function.
- Patients may then begin with a range of motion and grip-strengthening exercises.
- Therapists are more likely to give eccentric grip-strengthening exercises because this will influence the co-activation pattern of the wrist flexors, which help stabilize the wrist.
- Additional co-activation exercises may also be incorporated to improve global wrist stability.
- Exercises for the wrist while in a VersaSplit, a device designed for wrist and hand therapy, should be done cautiously and preferably under the guidance of a healthcare professional.
- Here are a few exercises that can be considered:
Wrist Flexion and Extension (With VersaSplit):
- Secure the wrist in the VersaSplit.
- Do controlled wrist flexion by moving the palm towards the forearm.
- Conduct controlled wrist extension by moving your fingers toward the ceiling.
- Repeat these actions for a comfortable range of motion.
Wrist Radial and Ulnar Deviation (With VersaSplit):
- Maintain your wrist secure in the VersaSplit.
- Gently tilt the wrist and hand towards the pinky side (ulnar deviation).
- Gently tilt the wrist and hand towards the thumb side (radial deviation).
- Do these motions within a comfortable range.
Grip Strengthening (With VersaSplit):

- Utilize the resistance provided by the VersaSplit to perform grip-strengthening exercises.
- Squeeze the device against resistance, hold for a few seconds, then release.
- Repeat for an expected number of repeats.
Wrist Circles (With VersaSplit):

- While the wrist is secure in the VersaSplit, perform gentle wrist circles in both clockwise and counterclockwise directions.
- Concentrate on maintaining smooth and controlled movements.
Pronation and Supination (With VersaSplit):
- Secure the forearm in the VersaSplit.
- Rotate the forearm and palm upward (supination).
- Rotate the forearm and palm downward (pronation).
When doing these exercises, always put your health and safety first. Start with low resistance and gradually increase as you feel more comfortable. If you experience pain, discomfort, or worsening of symptoms, stop the exercises and consult your healthcare provider or physiotherapist. They can provide specific guidance based on your condition and needs.
At 8 weeks post-operative:
- Active muscle training should be started
- A graded pain-free exercise program is recommended.
Physiotherapy treatment should have patient education and activity modification. Isometric activities should be incorporated to assist in strengthening the area and decrease the risk of instability. Isometric exercises can help strengthen muscles without causing joint movement, making them suitable for wrist and finger rehabilitation in cases of triangular fibrocartilage complex (TFCC) injuries. Remember to perform these exercises gently and without causing pain.
Here are a few isometric exercises you can consider:
Wrist Flexion Isometric Exercise:

- Rest the forearm on a surface with the palm facing upward.
- Put your other hand on top of the injured hand.
- Press the injured hand upward against the resistance of the other hand, without letting any action.
- Keep for 5-10 seconds and then release. Repeat for a few repetitions.
Wrist Extension Isometric Exercise:
- Rest the forearm on a surface with the palm facing downward.
- Put your other hand on top of the injured hand.
- Press the injured hand downward against the resistance of the other hand, without letting any motion.
- Keep for 5-10 seconds and then release. Repeat for a few repetitions.
Finger Isometric Exercise (Grip):

- Utilize a softball or a stress ball.
- Slowly squeeze the ball with the fingers and hold the contraction for 5-10 seconds.
- Release and relax the grip. Repeat for several repetitions.
Finger Isometric Exercise (Spread):
- Put the hand flat on a surface with the fingers slightly spread apart.
- Press the fingers outward against the surface, creating resistance without letting your fingers even move.
- Keep for 5-10 seconds and then relax. Repeat for a few repetitions.
- Always listen to the body and try to avoid any activity that causes pain or discomfort. As your strength increases, progressively raise the resistance from a low starting point.
- If you’re unsure or experiencing pain, consult with a healthcare professional or a physiotherapist who can guide the most appropriate exercises for your TFCC injury. In special, unilateral isometric movements are advantageous as they have been found to increase voluntary muscle activation bilaterally.
- This may be due to the motor cortex being stimulated, resulting in greater neuromuscular control.
- In addition, controlled isometric activation of the pronator quadratus in supination and neutral wrist position will help to stabilize the distal radioulnar joint (DRUJ).
- This may be utilized pre- and postoperatively in person with TFCC injuries.
At three months:
Postoperatively persons are likely to renew normal activity.
It takes an additional 3 to 4 months to back to normal sports activities.
Passive Mobilisation
Initially, traction of the radiocarpal and the midcarpal joints can be used to determine whether this provokes pain. To promote wrist flexion, a dorsal sliding technique can be used. Passive mobilization techniques can be beneficial in promoting wrist flexibility and addressing issues like restricted wrist flexion. Here’s a description of a passive mobilization technique called “dorsal sliding” for wrist flexion:
Passive Mobilization – Wrist Flexion Dorsal Sliding:
This technique aims to gently increase wrist flexion by applying controlled pressure on the dorsal (back) side of the wrist to encourage sliding of the carpal bones and improve joint mobility.
Preparation:
The person receiving the mobilization should be comfortably seated or lying down.
The mobilizer, typically a qualified healthcare professional or physiotherapist, should stand in a position that allows easy access to the wrist.
Execution:
- The mobilizer places their hands on the dorsal side of the wrist, with one hand stabilizing the forearm and the other hand gently cupping the back of the wrist joint.
- The mobilizer slowly and gently applies a posterior (backward) pressure on the wrist, encouraging the carpal bones to slide and the wrist joint to move into flexion.
- The mobilization should be performed within a pain-free range of motion and with controlled pressure.
- The mobilizer communicates with the person receiving the technique to ensure comfort and avoid excessive force.
Duration and Repetitions:
The mobilization is typically held for a few seconds (5-10 seconds) and then released.
This process can be repeated for a few repetitions, gradually working within the individual’s tolerance.
Communication and Feedback:
Open communication between the mobilizer and the person receiving the technique is essential. The person should provide feedback on their comfort level and any sensations they experience.
Post-Mobilization Stretching:
After performing the mobilization, some gentle stretching of the wrist flexors can be incorporated to further promote flexibility. This can be done by using the opposite hand to provide a controlled stretch on the palm side of the wrist.
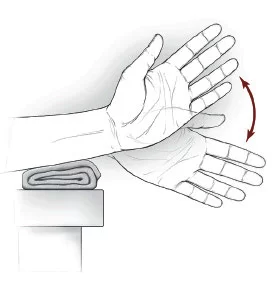
To encourage wrist extension, the volar sliding technique may be operated. Certainly, here’s an overview of a passive mobilization technique called “volar sliding” for wrist extension. This technique aims to gently increase wrist extension by applying controlled pressure on the volar (palm) side of the wrist to encourage sliding of the carpal bones and improve joint mobility:
Passive Mobilization – Wrist Extension Volar Sliding:
This technique focuses on promoting wrist extension by applying a controlled anterior (forward) pressure on the palm side of the wrist to encourage the carpal bones to slide and the wrist joint to move into extension.
Preparation:
The person receiving the mobilization should be comfortably seated or lying down.
The mobilizer, ideally a qualified healthcare professional or physiotherapist, should stand in a position that allows easy access to the wrist.
Execution:
- The mobilizer places their hands on the volar side of the wrist, with one hand stabilizing the forearm and the other hand gently cupping the palm side of the wrist joint.
- The mobilizer slowly and gently applies an anterior (forward) pressure on the wrist, encouraging the carpal bones to slide and the wrist joint to move into extension.
- The mobilization should be performed within a pain-free range of motion and with controlled pressure.
- The mobilizer communicates with the person receiving the technique to ensure comfort and avoid excessive force.
Duration and Repetitions:
- The mobilization is typically held for a few seconds (5-10 seconds) and then released.
- Repeat the technique for a few repetitions, working gradually within the individual’s comfort level.
Communication and Feedback:
- Maintain open communication between the mobilizer and the person receiving the technique.
- The person should provide feedback on their comfort level and any sensations they experience.
Post-Mobilization Stretching:
After performing the mobilization, consider incorporating gentle stretching of the wrist extensors by using the opposite hand to provide a controlled stretch on the dorsal side of the wrist.
As with any passive mobilization technique, it’s important to ensure that it is performed by a qualified professional with expertise in manual therapy. If you’re experiencing wrist issues or considering such techniques, consult a healthcare provider or a physiotherapist who can evaluate your condition and provide appropriate guidance and treatment.
- To facilitate the radial deviation the ulnar sliding technique may be used.
- To facilitate the ulnar deviation, the radial sliding technique may be used.
- Certainly, here are descriptions of passive mobilization techniques for both radial and ulnar deviations of the wrist.
- These techniques aim to gently increase the range of motion in these directions by applying controlled pressure on the wrist to encourage sliding of the carpal bones and improve joint mobility:
Passive Mobilization – Ulnar Sliding for Ulnar Deviation:
This technique focuses on promoting ulnar deviation by applying controlled pressure on the ulnar side of the wrist to encourage the carpal bones to slide and the wrist joint to move into ulnar deviation.
Preparation:
- The person receiving the mobilization should be comfortably seated or lying down.
- The mobilizer, ideally a qualified healthcare professional or physiotherapist, should stand in a position that allows easy access to the wrist.
Execution:
- The mobilizer places their hands on the ulnar side of the wrist, with one hand stabilizing the forearm and the other hand gently cupping the ulnar side of the wrist joint.
- The mobilizer slowly and gently applies a lateral (sideways) pressure on the wrist, encouraging the carpal bones to slide and the wrist joint to move into ulnar deviation.
- The mobilization should be performed within a pain-free range of motion and with controlled pressure.
- The mobilizer communicates with the person receiving the technique to ensure comfort and avoid excessive force.
Duration and Repetitions:
- The mobilization is typically held for a few seconds (5-10 seconds) and then released.
- Repeat the technique for a few repetitions, working gradually within the individual’s comfort level.
Passive Mobilization – Radial Sliding for Radial Deviation:
This technique focuses on promoting radial deviation by applying controlled pressure on the radial side of the wrist to encourage the carpal bones to slide and the wrist joint to move into radial deviation.
Preparation:
Follow the same preparation steps as described for the ulnar sliding technique.
Execution:
- The mobilizer places their hands on the radial side of the wrist, with one hand stabilizing the forearm and the other hand gently cupping the radial side of the wrist joint.
- The mobilizer slowly and gently applies a lateral (sideways) pressure on the wrist, encouraging the carpal bones to slide and the wrist joint to move into radial deviation.
- Ensure that the mobilization is performed within a pain-free range of motion and with controlled pressure. Communication with the person receiving the technique is crucial to ensure comfort and safety.
Duration and Repetitions:
- The mobilization is typically held for a few seconds (5-10 seconds) and then released.
- Repeat the technique for a few repetitions, working gradually within the individual’s comfort level.
As with any passive mobilization technique, it’s important to ensure that it is performed by a qualified professional with expertise in manual therapy. If you’re experiencing wrist issues or considering such techniques, consult a healthcare provider or a physiotherapist who can evaluate your condition and provide appropriate guidance and treatment.
General Mobility Exercises
The patient should perform general mobility exercises:
Wrists rotations-

- Wrist Rotations are an easy activity to learn and need little to no equipment to complete depending on the variation that a person chooses. Start by extending the arms straight out in front of you.
- Close the hands into a fist, and start rotating the wrist outwards in a circular movement. Initiateslowly in a tiny circle, then slowly Expand the range of motions as you go.
- Repeat for 10–15 secs and the change direction of rotation.
Horizontal ulnar and radial deviation-
- Start with sitting alongside the table the affected arm if possible is flexed at 90° so the arm and wrist may rest on the table the involved hand is placed, palm down on the picture receptor with the hand in radial deviation shoulder, elbow, and wrist should all be in the transverse plane, vertical to the central beam the wrist and elbow can be at shoulder height which produces the radius and ulna parallel (reducing the degree of arm motion causes the radius cross the ulna and thus relative shortening of the radius)
Active pronation and supination-

- Start with Sitting up straight with the arm to be exercised resting on a table.
- Carry a spoon or pen in your hand, with the majority of the spoon length extending towards the thumb side of your hand.
Stretching flexion and extension of the wrist
Wrist Stretching Exercises
Wrist Flexion, Extension & Side to Side
A. Wrist flexion – Slowly bend the wrist forward. Keep for 5 seconds. Perform 3 sets of 10.
B. Wrist extension – Slowly bend the wrist backward. Maintain for 5 seconds. Perform 3 sets of 10.
C. Sid to Side – Slowly move the wrist from side to side as though you were shaking hands. Keep for 5 seconds at each end. Perform 3 sets of 10.
Wrist Stretch

- With the opposite hand, help to flex the injured wrist down by pressing the return of the hand and holding it down for 15 to 30 seconds.
- Following, stretch the hand back by pushing the fingers in a backward direction and holding it for 10 to 20 seconds.
- Do 5 sets.
Wrist Extension Stretch
- Start with standing at a table with your palms down, fingers flat, and elbows straight.
- Lean the body weight forward. Maintain this position for 15 seconds.
- Repeat 3 times.
Strengthening Exercises
At the end of the therapy, then proceed to Strengthen exercises.
Wrist Extension With Dumbbell

- For the wrist extension, a person will need a dumbbell, a chair, and a table or desk.
- Start with sitting in a chair with the forearm resting on a table.
- Maintain a 2- or 3-pound dumbbell and hang the wrist and hand over the edge of the table.
- With the palm facing down, gradually lift the hand so the back of the hand pushes towards the ceiling.
- The forearm should stay on the table.
- Once the wrist is fully expanded, hold the position for a few seconds, then gradually lower your hand down.
- Repeat this motion 10 to 15 times.
- Perform two to three sets.
Dumbbell Wrist Flexion
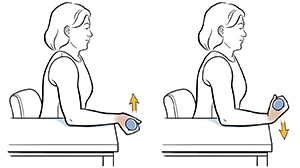
- Resume holding the weight and resting the forearm on the table. Turn the hand over, so the palm is facing the ceiling.
- Maintain the back of the arm against the table.
- Then, flex the wrist so that the palm pushes towards the ceiling.
- Once the wrist is fully flexed, maintain the position for two to three seconds.
- Then, gradually lower the hand back to the starting position.
- Repeat the wrist flexion movement for 2 to 3 sets of 10-15 repetitions.
- This exercise may also be done without the dumbbell.
Prayer Stretch

- Start with a Stand with the elbows bent and press the palms together, fingertips up, just below the chin (as if you’re praying).
- Keeping the fingers together, drop them until you feel a stretch along the insides of the arms.
- Allow the palms to separate but maintain the fingers together.
- Maintain for 30 seconds.
- Perform 2 to 4 repetitions.
Steeple Stretch
- For this stretch, begin in the “prayer” position from above.
- Splay the fingers and thumbs as wide as a person can comfortably.
- Keeping the fingers together, separate the palms and bring them back together.
- perform several repetitions a few times per day.
Wrist Supination With Dumbbell

- Start with sitting in a chair with the side of the forearm resting on the table and the wrist and hand hanging over the edge. The thumb should face the ceiling.
- Maintain the end of a small (1- to 3-pound) dumbbell in the hand, like you would hold a hammer.
- Gradually allow the hand and wrist to rotate over so the palm is facing up toward the ceiling.
- Maintain the stop position for a few seconds, then gradually rotate the hand back up, so the dumbbell is straight up once again.
- A person may link the supination movement with the pronation movement explained in the next step, alternating which way you rotate your wrist.
Wrist Pronation With Dumbbell
- Wrist pronation drives the position of the hand facing down as if a person were pouring a pitcher of water.
- To strengthen the wrist pronators, sit in a chair with the forearm supported on a table and the wrist and hand over the edge.
- Carry one end of a dumbbell with the weight pointing up towards the roof.
- Gradually rotate the hand, so the wrist and palm are facing down towards the floor. Maintain this position for a few seconds, then gradually turn the hand back to the starting position with the weight pointing up towards the ceiling.
- Perform 2 to 3 sets of this exercise with 10 to 15 repetitions.
- If a person combines this movement with wrist supination (in the previous step), alternate turning the palm up with turning the palm down.
FAQ
Recovery for TFCC tears that do not require surgery is usually four to six weeks. If surgery is necessary, it may take six weeks to several months to restore full wrist function. Physical therapy and avoiding activities that put pressure on your wrist can help you recover faster.
Treatment options for TFCC tears depend on the type, cause, and extent of the injury. In such cases, a TFCC tear will heal on its own. However, one should avoid using the affected wrist to prevent further injury and allow it to heal properly.
In a few cases, severe TFCC injuries can require surgery. Surgery is often necessary when a ligament tears in the hand. After surgery and recovery, your doctor may prescribe physical therapy for several weeks to restore flexibility and range of motion in your wrist.
In all cases, during primary inflammation, the recommended protocols are rest (so no exercise, lifting, or movement), ice, and immobilization. The best position for an injured wrist is neutral (see left) and supported.
Standard MRI scan
A TFCC tear can be detected with high throughput using conventional MRI. In a recent study, Zlatkin et al. found that the sensitivity, specificity, and accuracy were 92%, 89%, and 91% respectively (4).