Residual Poliomyelitis
Table of Contents
What is a Residual Poliomyelitis?
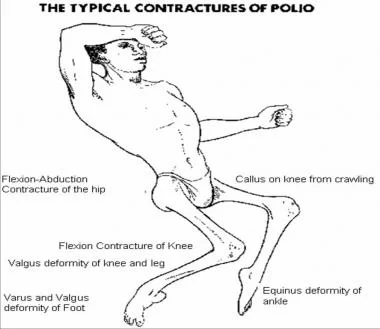
Deformities after polio arise due to residual paralysis that weakness the limb after acute attack of polio. The medical term for this is post polio residual paralysis. Weakened muscle strength, imbalance of the forces acting on a joint and unequal growth of affected and unaffected muscles results in limb length inequalities and joint deformities, muscle and fascial contracture.
- As polio may affect any region, there are plethora of deformities after polio that may occur in combination/alone.
- Fortunately, the polio is on the verge of eradication except for few countries.
- But we still come across the patients with post polio residual paralysis or PPRP.
How Does Muscle Weakness Occur?
- Muscle weakness results from the destruction of the nerve cells in the anterior horn which results in degeneration of the peripheral nerve. As the peripheral nerve degenerates, the muscle supplied by it atrophy. Therefore weakness in poliomyelitis is a kind of lower motor neuron injury.
- The extent of muscle degeneration depends on the amount of nerve involved.
- On dissection, atrophied muscle fibres are recognized by their yellowish- white colour. There could be fatty deposit around the atrophied muscle. Tendons atrophy from disuse and lose their normal glistening appearance. Bones are also involved in the pathological process they are more attenuated than normal with a considerable degree of osteoporosis.
- Shortening invariably occurs in paralytic limbs. The reduction of the blood supply from paralysed muscles is probably an important factor. Joint capsules and ligament when not protected by healthy muscles become stretched.
- The joints becomes unduly mobile and occasionally may dislocate if not protected. The skin circulation of the paralysed limb is affected and responds more readily to local temperatures.
- Once paralyzed, the recovery of individual muscle power may not show significant increase after 18 month though some functional improvement may continue.
Aim of Treatment in Residual Disease
-To correct soft tissue contracture,
-To improve function
-Prevent deformity by tendon transfer and stabilization procedures, and
-To correct inequality of leg length
-Exact approach varies with the person and the type of muscles affected.
-For sake of ease, I am going to discuss the deformities and condition, regionwise. The subject is vast and I am going to stick to the basics.
Hip Deformities
- Paralytic Dislocation of the Hip
- Paralytic dislocation of the hip is particularly common either acutely or slowly and indeed can be unnoticed. It follows flexion deformity, especially when associated with adduction. The relaxation of the joint capsule facilitates dislocation. The dislocation may be incomplete, giving rise to what is known as a ‘snapping’ hip.
- Some patients are helped by avoiding flexion and adduction positions of the hip by sitting and sleeping with their knees separated by a splint. Tenotomy of the adductors may be necessary.
- Surgeries for paralytic dislocation include Shelf operation where a bone shelf is created by turing piece of ilium.
- Arthrodesis of the hip is carried if other treatments fail.
Fixed Pelvic Obliquity
- Polimyelitis scoliosis is often associated with pelvic obliquity and perhaps a shorter lower extremity.
- A true, fixed pelvic obliquity is when the pelvis is held in a fixed oblique position by contractures, which may be above or below the pelvis or both.
It could be
- Infrapelvic, due to fixed contractures of soft tissues involving one or both femoral pelvic articulations
-Suprapelvic, due to fixed contractures at the spinal junction
-Intrapelvic when there is hypoplasia of one or both hemipelves.
-The treatment in severe deformities is surgical. For suprapelvic obliquity, correction of the scoliosis is desirable. - For infrapelvic fixed obliquity of pelvis, femoral intertrochanteric osteotomy is done.
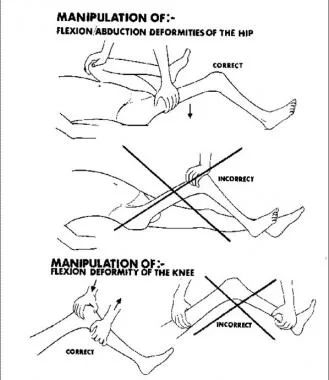
- Hip Flexion Contracture
- This results from contracture of the tensor latae, the iliopsoas, the Sartorius and the ractus femoris. It is frequently associated with adduction of the hip, flexion deformity of the knee and talipes equines of the foot.
- In severe cases and in cases which resist stretching, Soutter’s open division and fasciotomy is performed which involves stripping og hip flexors subperiosteally from their origin on lium and allowed to slip down the side of the pelvis. This permits of full extension of the hip.
- It is often combined with Yount’s operation [described later]
- Paralysis of Gluteus Maximus
- Paralysis of the gluteus maximus leads to increased lumbar and backward lurch on walking.
- Ober’s operation is done in paralysis of gluteus maximus which involves transfer of tensor fascia lata by dividing fascia lata, to inertion of guteus maiximus.
- In Dickson’s operation, the origin of the tensor fascia latae is transplanted with a piece of its bony attachment to a groove on the crest of the ilium near the posterior superior spine, the muscle thus being changed from an abductor and flexor or an abductor and extensor.
Paralysis of the Gluteus Medius Muscle
- Gluteus muscle is hip abductor and on its paralysis, when the weight is borne on the affected side, the patient lurches over to that side.
- Gluteus medius limp may occasionally be improved by posterior transference of the tensor fascia lata [Legg’s operation] when some residual power remains in the glutei but results are uncertain.
- Mustard operation involves transfer of iliopsoas tendon to act as the hip abductor in the presence of a normal gluteus maximus and of a normal Sartorius muscle.
- Contracture of the iliotibial band
- Contractures of iliotibial band are responsible for flexion—abduction deformity of the hip and also for obliquity of the pelvis. Bilateral contractures will produce increased lumber lordosis.
- Contracture and paralysis of tensor fasciae latae are intrinsically bound up with similar disease of the gluteus medius and minimus, and it only acts as a stabilizer of the pelvis in flexion and not in abduction.
Established contracture of the iliotibial band will not respond to conservative measures.
Early contractures may be satisfactorily corrected by division of the iliotibial band [ Yount’s operation]. In this surgery, the iliotibial band is divided about 2.5 cm proximal to the patella. A 5 cm section is excised.
If there is flexion—abduction contracture of the hip, the surgery may be supplemented by Complete release of the muscles of the iliac wing and transfer of iliac crest [Campbell Surgery].
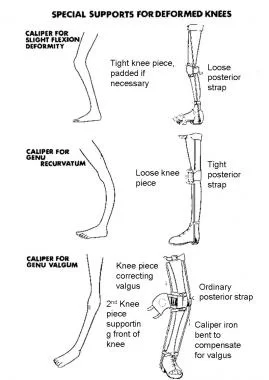
Knee Deformities
- Flexion Deformity of Knee
- Flexion knee deformity occurs when there is weakness of the anterior thigh muscles. There is strong over-action of the posterior group. The deformity can be prevented and corrected by the use of a Thomas’s knee splint. Other non-operative methods of reduction of the deformity are wedge plasters, reversed dynamic traction.
- Surgical correction is done by tendon lengthening of the semimembranosus, semitendinosus, gracilis, sartorius biceps and tensor fasciae latae.
- Knock knees
- Mild deformities usually are well tolerated. Severe deformities require corrective osteotomy.
- Genu Recuravatum
- Genu recurvatum signifies excessive extension at the knee. If there is adequate muscle power in hip flexors, the gluteus maximus and the hamstrings, the biceps femoris transfer to weakened quadriceps muscles could provide good results.
- For mild deformities, bracing can be done. Femoral flexion osteotomy could be considerd for severe deformities.
For all kind of deformities, knee arthrodesis may be considered if the deformity is not corrected by other methods.
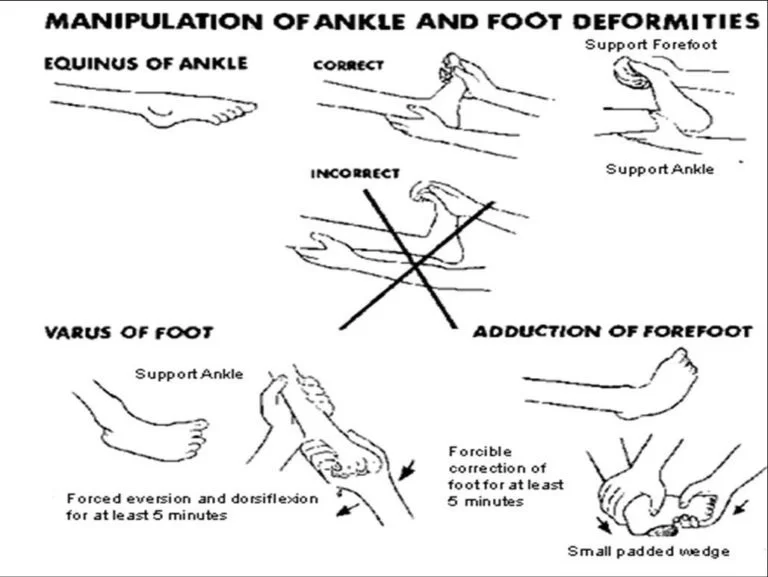
Leg and ankle Deformities
- Contracture of the Tendoachilles
- It may occur from overaction of the calf muscles unopposed by paralysed extensors.
- In severe cases the tendo calcaneus may have to be lengthened by open operation and the posterior capsule of the ankle joint divided it contracted.
- It must be noted that the patient with weak quadriceps use equines of the foot to back-knee for stability in stance and in these patients, lengthening of tendoachilles may cause worsening of the gait.
- Lateral Rotation Deformities of the Leg
- Lateral rotation deformities of the leg are commonly seen due to the muscular imbalance around the knee and ankle joints when either flexion or equines contractures develop. Corrective osteotomy may be done in selected cases.
- Plantar Fascia Contracture
- Persistent contracture of the plantar fascia produces a cavus or cavo—adducted foot. Steindler stripping operation gives a satisfactory result. In this surgery, the plantar fasica is divided close to calcaneus. After this, the foot is manipulated for correction and immobilized in plaster.
Deformities of the foot
- foot deformity: Foot deformities are treated by tendon transfers and bony procedure. The idea is to create a balance in opposing muscles so that recurrence of deformity can be avoided, or corrected with improvement in function. Following things should be kept in mind
- Imbalance between invertors and evertors should always be achieved
The opposing action tibialis anterior and peroneus longus should be kept in mind. Tibialis anterior elevates the base of the first metatarsal and supinates the base of the forefoot, while peroneus longus depresses the base of the first metatarsal and pronates the foot.
Valgus Foot - This is resulted by paralysis of the tibialis muscles. The calcaneum everts and no longer supports the head of the talus, which inclines medially and downwards with depression of the longitudinal arch.
Following procedure are used for this deformity
- Strut graft stabilization of the talocalcaneal joint
Peroneus brevis transfer to the medial cuneiform.
In the presence of over activity of the peroneus longus with cocking of the big toe, the tendon of extensor hallucis longus can be transplanted to the first metatarsal and the interphalangeal joint of the hallux is fused.
In long standing deformities where passive correction of the subtalar joint is not possible, triple arthrodesis is done.
Varus Foot - This is due to paralysis the peroneal muscles. The foot becomes inverted due to the action of the tibialis anterior and posterior.
- Correction may be obtained by a strut-graft inserted into the sinus tarsi from the inner side, supplemented by transplantation of the tibialis anterior to the cuboid.
- Calcaneus Foot
- Calcaneovalgus foot
Calcaneovalgus foot
This deformity is due to isolated paralysis of the gastrocnemius. Active dorsiflexors plus active peronei and tibialis posterior muscles produce a progressive calcaneocavus deformity despite caliper protection. - In the young child the deformity may be minimized by transplantation of the tibialis posterior and peroneal tendons into the heel cord, followed by protection with a caliper.
- In the older child, transplantation of tendons into the heel cord should be accompanied by triple arthrodesis.
- Equinus Foot
- Paralysis drop- foot is satisfactorily controlled by a caliper with a toe-raising spring or a dorsiflexion spring at the ankle. Lambrinudi foot fusion with transplantation of overacting pernoei to the dorum of the foot is reserved for the older patient.
- A Pes Cavus
A Pes Cavus
Claw Toe Defomity of the Hallux - This is hyperextension deformity of the first metatar-sophalangeal joint, which occur on attempted dorsiflexion of the foot is caused by unco-ordinated contraction of the extensor hallucis when the tibialis anterior is paralysed.
- Claw toe deformity occurring in a foot with adequate dorsiflexion power is satisfactorily treated by interphalangeal fusion of the hallux.
- Transference of the extensor hallucis tendon to the neck of the first metatarsal accompanied by interphalangeal fusion of the hallux is a satisfactory procedure when the power of dorsiflexion of the foot is only slightly impaired.
- Different Stabilizing Surgeries of the Foot
- Stabilizing operations consist of fusion of different joints of foot and/or osteotomies.
- Foot fusion operations should be postponed until the age of 10—12 unless deformities is too severe to press for an early fusion.
- Different Stabilizing Procedures of the Foot are
- Extra articular arthrodesis of the subtalar joint .
- This involves the reduction and maintenance of the calcaneus in normal relationship the sinus by means of strut bone grafts placed the sinus tarsi. Muscle balance is restored by tendon transplantation to avoid recurrence.
Triple arhtrodesis
- Fusion of the subtalar and midtarsal joints is indicated when deformity or instability of the foot is accompanied by lateral stability of the talus in the ankle mortice. Varus or vagus deformities are corrected by excising appropriate wedges of bone from the midtarsal and subtalar joints. Deformities such as knock knee the tibial torsion should also be corrected at the site of deformity.
- Naughton Nunn operation
- In case of severe static deficiencies, it is desirable to secure forward displacement of the talus on the calcaneus. The operation combines a subtalar arthrodesis with a reconstructive shortening of the forefoot.
- The head of the talus is divided behind its articular cartilage, and this along with the proximal surfaces of the cuneiform bone, is removed together with the navicular.
- The foot is displayed backwards at the subtalar joint so that the head of the talus will rest in a shaped depression prepared for it by the removal of bone from the dorsal surface of the cuneiform bones.
- Polio treatment in the acute stage of muscle paralysis
- It involves meticulous attention to intensive care during the acute paralytic phase.
- Feeding by nasogastric tube in those with bulbar dysfunction.
Endotracheal intubation and ventilation should be instituted in case of respiratory muscle failure or bulbar and laryngeal muscle paralysis.
Pulmonary atelactasis and infection are treated with antibiotics and regular physiotherapy intervention.
Rest on a firm mattress with back supported on a lumbar board. Avoid forceful exercise as this may increase paralysis. Avoid massage.
Moist hot packs to the affected muscles produce considerable relief from the pain. Analgesics can also be used to relief pain.
Feet to be supported by rigid boards at 90° angle. Early spinal bracing for the back if it is weak.
Hip and knees should be positioned as straight as possible and arms in abduction with mild support.
Passive range of motion for the joints to avoid contracture formation.
Positon the patient with face down and hip extended every 2 hourly to prevent pressure sores and deformities. - Polio treatment in the recovery or convalescent stage
- Sitting up can be encouraged if the paralysis is not severe.
As soon as the fever drops, exercises should be started to prevent contractures and return strength.
Passive, active assisted to active resisted/ strengthening exercises, sitting balance training, standing balance training in parallel bars, gait training should be started.
Crutches, leg braces(calipers) and other aids may help the child to move better and may prevent contractures or deformities.
Whenever possible make exercises fun. Active games, swimming and other activities to keep limb moving as much as they can are important throughout the child’s rehabilitation.
Rehabilitation (stage 3) in poliomyelitis once all the recovery has taken place. Goals of polio treatment in the stage of residual paralysis
Strengthening of all the innervated muscles.
Preventing contractures and deformities.
Making the patient as independent as possible.
Emotional and psychological support.