Abducens nerve palsy
Table of Contents
What is a Abducens nerve palsy?
The Abducens nerve is the sixth nerve of the cranial nerve. Sixth nerve palsy takes place when the sixth cranial nerve is damaged or does not work right. This condition causes problems in eye movement.
The sixth cranial nerve gives signals to the lateral rectus muscle. This is a tiny muscle that attaches to the outer part of the
eye. When this muscle contracts, the eye moves away from the nose. Every eye has its own lateral rectus muscle given out by its own cranial nerve.
The sixth nerve originates from the lower part of the brain. It goes far away before reaching the lateral rectus. Injury at any point along its path may cause the nerve to work badly or not at all. Because the lateral rectus muscle may no longer contract perfectly, the eye turns inward toward the nose.
Sometimes, sixth nerve palsy takes place without any other symptoms. This is known as isolated sixth nerve palsy. Other times, sixth nerve palsy can come with other symptoms. This is known as nonisolated sixth nerve palsy.
Sometimes, sixth nerve palsy is present from birth. It may also outcome from other problems that take place later on. In babies, injury is a leading cause. In younger, stroke is one of the most usual causes. It is relatively rare.
Description of 6th nerve (Abducens nerve)
- The abducens nerve is the 6th cranial nerve (CN VI).
- It is, accompanies the oculomotor nerve (CN III) and the trochlear nerve (CN IV)superintend for the extraocular motor functions of the eye.
- The 6th nerve has a purely somatic motor function.
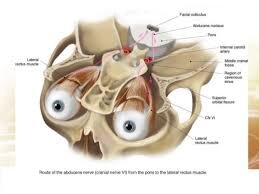
Course
- The abducens nerve arises from a set of neural cells that are ground in the ventral aspect of the pons. It then comes out from the brainstem at the pontomedullary junction to go into the subarachnoid space, coursing in an upward direction between the pons and clivus to come in the Dorello canal.
- At the petrous apex, it angulates to go into the cavernous sinus and travels in adjacent proximity to the internal carotid artery.
- The abducens nerve then goes through the superior orbital fissure and innervates the lateral rectus muscle.
- It has the 2nd longest intracranial course of all the cranial nerves.
Function
- The abducens nerve is a purely somatic motor nerve, It does not have any sensory function.
- It empowers the lateral rectus muscle, an extraocular muscle of the eye, which is responsible for the abduction of the eyes on the same (ipsilateral) side.
- The abducens nerve is also secondarily connected with innervation of the contralateral rectus muscle by way of the longitudinal fasciculus so that each eye moves laterally in a coordinated manner.
What causes Abducens nerve palsy?
Too many problems may disorganize the function of the 6th cranial nerve, causing sixth nerve palsy. Possible causes involve:
- Injury (specifically if a skull fracture is present)
- Stroke
- Infection (Particularly, from Lyme disease or from a virus)
- Brain tumor
- Inflammation of the nerve, particularly after a vaccine
- Multiple sclerosis
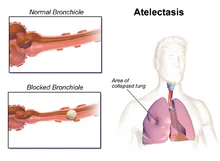
- Elevated pressure inside the brain (particularly, from meningitis)
- In congenital 6th nerve palsy, a problem with the 6th cranial nerve is present at the time of birth.
- This can takes place as an outcome of injury during birth. Sometimes, the cause of 6th nerve palsy is unknown.
- Sixth nerve palsy that occurs without additional symptoms is generally because of the following:
- Injury
- Congenital cause
- Viral illness
- High blood pressure
- Diabetes
What are the symptoms of sixth nerve palsy?
- Sixth nerve palsy can affect one or both eyes, depending on its cause.
- The most normal symptom of 6th nerve palsy is a double vision when both eyes are open.
- This is more normal when looking far away or when looking in the direction of the affected eye.
- But not everybody with sixth nerve palsy has this symptom.
- The eyes can also be out of alignment—a symptom that identifies strabismus.
- The eye on the involved side can drift toward the midline.
- Early on, a person might show this symptom only when looking in the direction of the involved eye (like looking to the right in a right sixth nerve palsy).
- If the palsy worsens, the involved eye may drift toward the midline, even when looking straight ahead.
- If a person has nonisolated sixth nerve palsy, additional symptoms can be present as well.
- Based on the other structures involved, a person might have symptoms like:
- Hearing loss
- Facial weakness
- Decreased facial sensation
- Droopy eyelid
- Fever
- Headache
- Nausea and vomiting
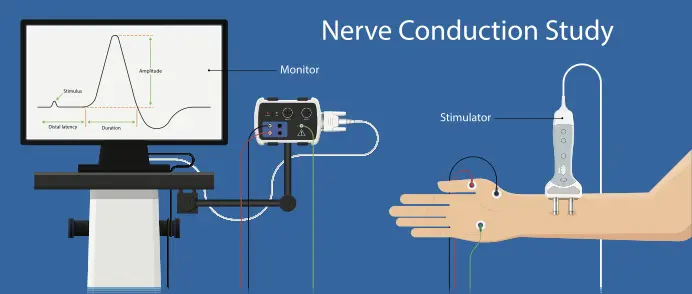
How is Abducens nerve palsy diagnosed?
- Diagnosis initiates with a thorough past and present medical history and physical exam. The doctor will do a detailed neurological exam. This is testing to recognize other involved parts of the brain and nervous system. A general practitioner or a physician who specializes in the nervous system (a neurologist, optometrist, ophthalmologist, or neuro-ophthalmologist) might
- first examine the patient. They will try to identify the root cause of the sixth nerve palsy as well.
- The doctor will probably want to order brain imaging tests because the nerve frequently becomes compressed as it
- leaves the brain. Brain imaging is also necessary to make sure a brain tumor is not causing symptoms.
- Possible imaging tests incorporate computed tomography (CT) and magnetic resonance imaging (MRI).
- MRI gives more information. But it is frequently hard to do as quickly as a CT.
- A CT might be needed if the doctor suspects that a person has increased pressure inside the brain.
Sometimes, the doctor might order other tests if they identify a specific cause of the sixth nerve palsy. For example, a person might require blood tests and a lumbar puncture if meningitis is diagnosed.
How is sixth nerve palsy treated?
Treatment of sixth nerve palsy based on its cause. Possible treatments for the underlying cause involve:
- Antibiotics, for 6th nerve palsy due to bacterial infection
- Corticosteroids, for 6th nerve palsy due to inflammation
- Surgery or chemotherapy, for 6th nerve palsy due to a tumor
- Sometimes, there is no direct treatment available for the underlying cause.
- The doctor can want to wait a few months prior to starting additional treatment.
- Often, symptoms from sixth nerve palsy resolve on their own. Sixth nerve palsy following a viral illness frequently completely goes away within a few months. Symptoms following trauma can also improve over several months.
- But in cases of trauma, symptoms are less likely to run away completely.
- The symptoms can be more likely to go away completely if a person has isolated sixth nerve palsy.
- If a person still has symptoms 6 months or so later, the doctor might suggest further treatments.
- Some available treatments are:
- Alternate patching of each eye to eliminate double vision (often a primary treatment)
- Special prism glasses to help straighten the eye
- Botulinum toxin temporarily paralyzes the muscle on the opposite side of the eye and helps eye alignment
Surgery
- The doctor can be most likely to suggest surgery if other treatment choices have not been effective.
- Strabismus surgery may be done for persistent abducens nerve palsies that demonstrate stable measurements over a 6-month period.
- A forced duction test is done in the office or in the operating room in order to assist with surgical planning.
- If there is residual lateral rectus muscle function: Frequently, a resection of the involved lateral rectus and recession of the ipsilateral medial rectus (recess/resect or “R and R” procedure) is done.
- Alternatively, a resection of the involved lateral rectus with a recession of the contralateral medial rectus can be performed.
- If there is no lateral rectus muscle function: various kinds of transposition surgeries may be considered (for example full tendon transposition, Jensen, Hummelsheim, Augmented Hummelsheim with resections +/- Foster modifications, Knapp’s procedure).
- Superior rectus transposition managed with medial rectus recession has been shown to improve esotropia, head position, and abduction in patients with abducens palsy.
- Botulinum toxin injections to the medial rectus of the involved eye may also be used as a temporary treatment.
What are the possible complications of Abducens nerve palsy?
- Isolated sixth nerve palsy itself does not generally cause complications. But many of the possible causes of 6th nerve palsy may have complications. Like any procedure, surgery for 6th nerve palsy brings a risk for complications.
Exercise therapy for Abducens nerve palsy
Who benefits from exercises:
- Digital eye strain as in individuals who works on a computer for a long time and can cause dry eyes, eye strain, blurred vision, and headaches.
- Increased light sensitivity.
- A surgery that required strengthening the muscles
- If there is a problem in focusing eyes in reading.
- Convergence insufficiency.
- The lazy eye that develops in some children – eye exercises stimulate the vision centers in the brain.
Effect of oculomotor and gaze stability exercise:
- Ocular-motor exercises increase dynamic visual acuity (DVA) in dynamic sports that have a prominent effect on athletes’ performance for example basketball, in this study on women basketball players the intervention, was for four weeks six sessions per week for ten min twice daily.
- Gaze and ocular-motor increase balance and stability in normal adults and a study proves that it can be promising to increase balance after stroke.
- These exercises improve symptoms of eye fatigue and strengthen the extraocular muscles.
- Eye movements will improve the strength of weak eye muscles, improving blood circulation and muscle tone.
- The eye muscles should be done to reach the most sensitive vision possible, with the benefit of glasses and contacts, if needed.
- This toning allows for minimizing eye stress, permitting the eyes to work more efficiently.
Blinking exercises
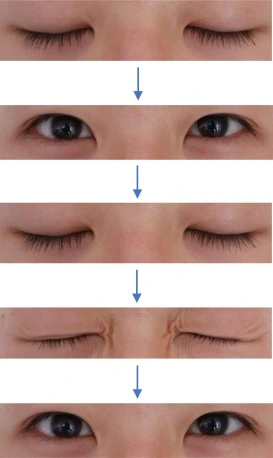
- Blinking activities are like a rest for the eyes it assists in maintaining them fresh and concentrating for a longer time.
- Blinking improves symptoms of dry eye, digital eye pressure, and blinking patterns, a 10-second blinking activity every 15 minutes will be with the asset.
Eye movement
- Eye activity usually shifts the eyes up and down and reprises three times then also moves the eye slowly from right to left and reprises three times then relaxing.
Figure of 8
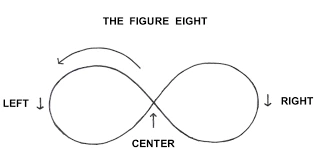
- A figure of 8, is another activity for eye movement, suppose there is a significant figure of 8 away 9 to 10 feet from the patient, then move the eye in the path of this infinity spiral for almost 20 seconds then change the direction.
Focus change
- Focus shift, maintain the finger a few inches far from a patient and concentrate the gaze on it then concentrate on another item far from the patient, now back to the look to the finger.
Pencil pushups

- The person maintains a pencil/patient’s thumb on the outstretched arm midway between eyes, ask the person to attempt to maintain a single picture of the pencil while slowly moving the pencil in relation to the nose till it is not likely to see the pencil in a single picture right away.
- now ask the person to move it slowly away to the nearest point where there is a single figure of pencil achieved.
- This activity permits persons with symptomatic convergence deficiency.
FAQ
A nerve injury can influence or affect the brain’s ability to communicate with muscles and organs. Injury to the peripheral nerves is known as peripheral neuropathy. It is necessary to get medical care for a peripheral nerve injury as early as possible. Early diagnosis and treatment can prevent complications and lifetime damage.
Patients who develop abducens nerve palsy frequently present with binocular horizontal diplopia, which is a double vision when looking at objects side by side. There will be a notable weakness of the ipsilateral lateral rectus muscle leading to a deficit in eye abduction on the involved side.
The abducens nerve functions to innervate the ipsilateral lateral rectus muscle and moderately innervate the contralateral medial rectus muscle (at the level of the nucleus – via the medial longitudinal fasciculus).
oculomotor
Cranial nerves 3rd (CNIII) (oculomotor), 4th (trochlear), and 6th (abducens) control the position of the eyeballs; CN3rd influences the position of the eyelids and the size of the pupils.
Sympathetic fibers destined for the pupil dilators and Mueller’s muscle of the lid run in continuity with the abducens nerve for some millimeters prior to joining the ophthalmic division of the trigeminal nerve within the cavernous sinus.




One Comment