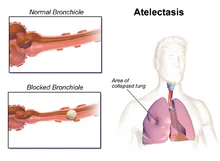
Atelectasis
- Atelectasis happens when lung sacs (alveoli) can not inflate properly, which means blood, tissues, and organs may not get oxygen. It can be caused by pressure outside of your lung, a blockage, decrease airflow, or scarring. The most usual cause of atelectasis is surgery with anesthesia. Atelectasis usually resolves later by treating the underlying cause.
- When some of the alveoli in your lungs do not fill with air, it is called atelectasis.
- Your airways are branching tubes that rush throughout both your lungs. When you breathe, air moves from the main airway in your throat, sometimes known as your windpipe, to your lungs.
- The airways continue branching and get progressively smaller until they end in little air sacs known as alveoli.
- Your alveoli are where your body exchanges the oxygen in the air for carbon dioxide (CO2), a waste product from your tissues and organs. In order to do this, your alveoli must fill up with air.
- Depending on the underlying cause, atelectasis can include either small or large portions of your lung.
- Keep reading to learn more about atelectasis, involving its obstructive and nonobstructive causes.
Table of Contents
What is atelectasis?
- Atelectasis (pronounced at-uh-LEK-uh-sis) is the collapse of one or more areas of the lung. It specifically harms the little air sacs called alveoli.
- When you inhale, your lungs fill up with air. The air travels to pockets in your lungs (alveoli), where the oxygen moves into your blood. The blood delivers oxygen (O2) to organs and tissues throughout your body.
- If you do not have enough air coming in to inflate your alveoli or if outside pressure is pushing on them, they can collapse (atelectasis). Atelectasis can occur in a small area or the whole lung. If enough of your lung is harmed, your blood may not receive enough oxygen, which can cause health issues.
What is the difference between atelectasis and pneumothorax?
- Atelectasis is a condition where alveoli in your lung or an area of your lung deflate, causing a partial or complete collapsed lung. Pneumothorax is a condition where air drains into the space around your lung, compressing it and causing it to collapse.
What does atelectasis indicate?
- If you have not had a chest or abdominal surgery recently, atelectasis can indicate an obstruction of your airway that is causing a partial or complete collapse of your lung.
Who is at risk for atelectasis?
You are at a higher risk for atelectasis if you have:
- Had chest or abdominal surgery that requires medication to retain you relaxed or asleep (anesthesia), preventing you from taking deep breaths.
- A condition that blocks the little airways (branches) in your lungs, preventing normal lung expansion.
- A chest injury or rib fracture causes serious pain. This may retain you from being able to take deep breaths.
- Had smoke exposure.
What are the three types of atelectasis?
- There are three important types of atelectasis: compressive, resorptive (obstructive), and contraction.
Compressive atelectasis
- Compressive atelectasis is when something around your lung — such as fluid, air, blood, or a tumor — pushes against it, causing it to collapse.
Resorptive/obstructive atelectasis
- Resorptive atelectasis occurs when the oxygen and carbon dioxide in your alveoli move into your bloodstream and no new air moves in. This causes your alveoli to collapse. Surgery that requires anesthesia is a usual cause of resorptive atelectasis.
- Something blocking the inside of your lung, retaining air from coming into the alveoli, can also cause resorptive atelectasis. Also known as obstructive atelectasis, the blockage can be mucus, a tumor, or an object that you accidentally inhaled.
Contraction atelectasis
- Lung scarring (fibrosis) causes contraction atelectasis. Scarring retains the alveoli from opening properly.
Other types of atelectasis
- Newborns, particularly premature newborns, or people with acute respiratory distress syndrome (ARDS) can have an unusual type of atelectasis called patchy atelectasis. Patchy atelectasis occurs when you do not have enough of a protein in your lungs that helps keep them from collapsing (surfactant).
- Other types of atelectasis (bibasilar atelectasis, rounded atelectasis, gravity-dependent atelectasis, and subsegmental atelectasis) describe the location, appearance, or seriousness of the collapse.
What are the symptoms of atelectasis?
- Atelectasis often causes no symptoms on its own, though certain underlying conditions that lead to atelectasis (like COPD) can cause symptoms.
- If atelectasis harms large areas of the lungs, the oxygen level in your blood may go down (hypoxemia).
This can conduct in symptoms like:
- Trouble breathing/shortness of breath (dyspnea).
- Coughing.
- Chest pain.
- Rapid breathing (tachypnea).
- Skin and lips turning blue.
- The symptoms of atelectasis range from nonexistent to very severe, depending on how much of your lung is affected and how fast it develops. If only a few alveoli are involved or it occurs slowly, you might not have any symptoms.
If you are looking for signs and symptoms of atelectasis, they may involve:
- shallow breathing
- rapid breathing
- fever
- chest pain
- wheezing or crackling sounds
- coughing
- sputum (phlegm, or thick mucus) production
- less chest expansion.
Sometimes, pneumonia develops in the affected area of your lung. When this occurs, you can have the typical symptoms of pneumonia, such as:
- coughing up phlegm
- fever
- chest pain.
What is the most common cause of atelectasis?
- Surgery is the most usual cause of atelectasis. When anesthesia is used during surgery to keep you asleep, you do not breathe deeply enough to fill your lungs all the way or cough to clear your lungs of mucus. This can conduct in blockages or lack of air to the alveoli, causing resorptive atelectasis.
Other causes of atelectasis involve:
- Mucus plug. A buildup of mucus is common later surgery, in children, in people with cystic fibrosis, and during severe asthma attacks.
- Inhaled object. A lung blockage by an accidentally inhaled object is particularly usual in children, who often inhale small toy parts or foods.
- Fluid around the lungs (pleural effusion). Underlying illness (such as heart disease) is commonly the cause of pleural effusion.
- The air around the lungs (pneumothorax).
- Non-cancerous (benign) growths.
- Cancerous tumors.
- Lung scarring.
- Underlying illness. Conditions such as chronic obstructive pulmonary disease (COPD) or acute respiratory distress syndrome (ARDS) and respiratory infections such as COVID-19 or pneumonia can lead to atelectasis.
Causes of obstructive atelectasis
- Obstructive atelectasis occurs when a blockage develops in one of your airways. This prevents air from getting to your alveoli, and as an outcome, they collapse.
Things that can block your airway involve:
- inhalation of a foreign object, such as a little toy or small pieces of food,
- mucus plug (a buildup of mucus) in an airway,
- tumor growing in an airway,
- tumor in the lung tissue that presses on the airway.
Causes of nonobstructive atelectasis
- Nonobstructive atelectasis refers to any type of atelectasis that is not caused by certain kinds of blockage in your airways.
Common causes of nonobstructive atelectasis involve:
Surgery
Atelectasis can happen during or later any surgical procedure. These procedures often need you to:
- receive anesthesia
- use a breathing machine
- take pain medications and sedatives later the surgery
- potentially stay in bed
- Together, these factors can make your breathing shallow. They can also make you less likely to cough, even if you require to get something out of your lungs.
- Sometimes, not breathing deeply or not coughing can cause certain of your alveoli to collapse. If you have a procedure coming up, speak with a healthcare professional about ways to decrease your risk of atelectasis after surgery.
- You may have access to a handheld device called an incentive spirometer to use in the hospital or at home to encourage deep breathing.
Pleural effusion
- Pleural effusion is a buildup of fluid in the space connecting the outside lining of your lung and the lining of your inner chest wall.
- Usually, these 2 linings are in close contact, with the lining of the chest wall helping hold the lungs open. These assists keep your lung expanded.
- However, a pleural effusion causes the linings to disconnect and lose contact with each other. The elastic tissue in your lung pulls inward, driving air to exhale your alveoli.
Pneumothorax
- People sometimes confuse atelectasis with pneumothorax, which is also known as a collapsed lung. However, they are different conditions.
- That said, pneumothorax can conduct to atelectasis because your alveoli will deflate as your lung collapses.
- Pneumothorax is very similar to pleural effusion but includes a buildup of air, rather than fluid, between the linings of your lung and chest.
- Air gets stuck in the space connecting the outside of your lung and your inner chest wall. This causes your lung to contract or collapse, squeezing the air out of your alveoli.
Lung scarring
- Lung scarring is also known as pulmonary fibrosis.
- It is usually caused by long-term lung infections, such as tuberculosis. Long-term exposure to irritants, involving cigarette smoke, can also cause it. This scarring is permanent and creates it harder for your alveoli to inflate.
Chest tumor
- Any kind of mass or growth near your lungs can lean pressure on your lung. This can force certain of the air out of your alveoli, causing them to deflate.
Surfactant deficiency
- The walls of your alveoli are normally coated with a substance known as a surfactant that helps them stay open. When there is too small of it, the alveoli collapse. Surfactant deficiency tends to occur in infants who are born prematurely.
How is atelectasis diagnosed?
- Chest X-rays (pictures of your lungs) are the 1st step in diagnosing atelectasis. Your healthcare provider (doctor) may use a computed tomography (CT) scan to get more detailed pictures if necessary.
- In some cases, your provider may see the inside of your lungs using a small camera attached to a tube that goes down your throat (bronchoscopy). Blockages may be removed during bronchoscopy.
- Blood oxygen level test: A healthcare professional typically does this with an oximeter, a little device that fits on the end of your finger.
- Blood test: A healthcare professional takes blood from an artery, commonly in your wrist, and runs a blood gas test to check your blood chemistry and levels of oxygen and carbon dioxide (CO2).
- Chest X-ray: A chest X-ray uses a small dose of radiation to make images of the inside of your chest so a healthcare professional can look for any abnormalities.
- CT scan: A CT scan assists them to check for infections or blockages, such as a tumor in the lung or airway.
- Bronchoscopy: A bronchoscopy is a procedure that includes inserting a thin, flexible tube with a camera through your nose or mouth and into your lungs.
How is atelectasis treated?
- Many cases of atelectasis acquire better without treatment, under careful monitoring by your healthcare provider (doctor).
Another treatment depends on the cause and extent of the collapse. Treatments could involve:
- Deep breathing exercises (incentive spirometry).
- Removing obstructions in your lung (usually using bronchoscopy).
- Physical therapy helps promote the expansion of your lungs.
- Inhaled medications to expand your airways (bronchodilators).
- Treatment of tumors or chronic lung conditions.
Nonsurgical treatment
Most cases of atelectasis do not require surgery. Depending on the underlying cause, a healthcare professional (doctor) might suggest one or more of these treatments:
- Chest physiotherapy treatment: This involves moving your body in various positions and using tapping motions, vibrations, or wearing a vibrating vest to help loosen and drain mucus. It is generally used for obstructive or postsurgical atelectasis. This treatment is also usually used in people with cystic fibrosis.
- Bronchoscopy: A healthcare professional can insert a little tube through your nose or mouth into your lungs to remove a foreign object or clear a mucus plug. They can also use the technique to remove a tissue sample from a mass to assist figure out what is causing the problem.
- Breathing exercises: Exercises or devices, such as an incentive spirometer, can force you to breathe in deeply and assist open up your alveoli. This is especially helpful for postsurgical atelectasis.
- Postural Drainage: If your atelectasis is due to pneumothorax or pleural effusion, a healthcare professional may require to drain air or fluid from your chest. They will likely insert a needle through your back, connecting your ribs, and into the pocket of fluid. To remove air, they may require to insert a plastic tube, known as a chest tube. This may need to be left in for several days in more serious cases.
Surgical treatment
- In very rare cases, you may require to have a small area or lobe of your lung removed.
- Healthcare professionals will usually only do this later trying all other options or in cases involving permanently scarred lungs.
Physiotherapy treatment
| Airway clearance techniques | Suctioning of respiratory secretions. Percussion and vibration therapy. Positive expiratory pressure. Active cycle of breathing technique. Postural drainage. Chest high-frequency oscillations (CHFO) can be delivered via The Metaneb System. Mechanical insufflation and exsufflation. Manual lung hyperinflation. | |
| Breathing exercises | Incentive spirometry Sustained maximal inspiration Intermittent positive pressure breathing | |
| Positioning | Kinetic Therapy: It is defined as the continuous turning of a patient slowly along the longitudinal axis to ≥ 40° onto each side, using a specialized bed. Turning side to side Prone positioning | |
| Early mobilization | Sitting out of bed Standing on the first postoperative day, Walking a short distance in the room or corridor on the second postoperative day |
How can I reduce my risk of atelectasis?
Here are some ways to decrease the risk of atelectasis:
- Get up and walk around, perform breathing exercises, and use an incentive spirometer later surgery as directed by your healthcare provider.
- If you have any underlying conditions that can cause atelectasis, follow your provider’s (doctor’s) recommendations for treating that condition.
- Do not smoke or quit smoking.
- Keep little objects away from children to reduce their risk of inhaling them.
Is atelectasis serious?
While atelectasis is commonly not serious itself, some cases can have serious complications:
- Decrease blood oxygen level (hypoxemia). If air can not get into the alveoli because of collapse, it can not get into your blood or out to your tissues and organs.
- Pneumonia. A mucus sitting in collapsed airways can cause an infection.
- Respiratory failure. Serious cases of atelectasis (like an entire lung collapsing) can cause respiratory failure, which is life-threatening.
Can you prevent atelectasis?
It may be possible to prevent atelectasis in certain cases.
To help prevent atelectasis during and later surgery, healthcare professionals may recommend that you:
- stop smoking if you smoke, ideally 6 to 8 weeks ahead of surgery
- do regular deep breathing exercises,
- help an incentive spirometer to encourage deep breathing
- take medication,
- help a breathing device — a continuous positive airway pressure (CPAP) machine, for example.
- Children may be at a higher risk of inhaling little objects. You can assist prevent them from developing obstructive atelectasis by keeping small objects safely out of reach.
- People who have to remain in bed for long periods of time should try to move around regularly. It is also important for them to frequently practice taking deep breaths.
What is the outlook for atelectasis?
- Most of the time, atelectasis is reversible once the cause is treated. Most people recover quickly and have no severe lasting effects. In people who have a long-lasting (chronic) condition, further treatment may be required to manage the underlying cause of atelectasis.
- Mild atelectasis is rarely life-threatening and commonly goes away quickly once the cause is addressed.
- Atelectasis that affects most of your lungs or occurs suddenly is almost always caused by a life-threatening condition, such as a blockage of a major airway or when a big amount of fluid or air is compressing 1 or both lungs.
How do I take care of myself?
- The best way to take care of yourself is to follow your healthcare provider’s recommendations for care later in surgery. Make sure you manage any underlying conditions that can improve your risk of atelectasis.
When should I see my healthcare provider?
- If you have recently had surgery or have an underlying condition and have any new or worrisome symptoms, contact your healthcare provider (doctor) immediately.
NOTE
- Your lungs are a complicated and main organ. They require to get airflow in and oxygen to your blood so that your tissues and organs work properly. Atelectasis is something that can occur when one part of that system isn’t working quite as planned. Fortunately, while “collapsed lung” — even just a partial one — sounds scary, in most cases, atelectasis is not a life-threatening condition.
FAQs
Atelectasis is caused by a blockage of the air passages (bronchus or bronchioles) or by pressure on the outside of the lung. Atelectasis is not the same as another type of collapsed lung called pneumothorax, which occurs when air escapes from the lung.
Treatment of atelectasis depends on the cause. Mild atelectasis may go away without treatment. Sometimes, medications are used to loosen and thin mucus. If the condition is due to a blockage, surgery or other treatments may be needed.
What are the three types of atelectasis? There are three main types of atelectasis: compressive, resorptive (obstructive), and contraction.
Atelectasis usually resolves itself with time or treatment, while lung or airway collapse is reversible. For example, most people who develop atelectasis due to surgery recover 24 hours afterward.
The duration of atelectasis depends on what is blocking the airway and can be affected by pain levels and shallow breathing post-op. 7 The lung will usually begin reinflating once whatever was blocking the airway is cleared or lungs are able to expand again, but it takes time to regain full use of the airways.






2 Comments