Electromyography (EMG)
Table of Contents
What is electromyography (EMG)?
- Electromyography (EMG) measures muscle response or electrical activity in reaction to a nerve’s stimulation of the muscle. The test is used to assist detect neuromuscular abnormalities.
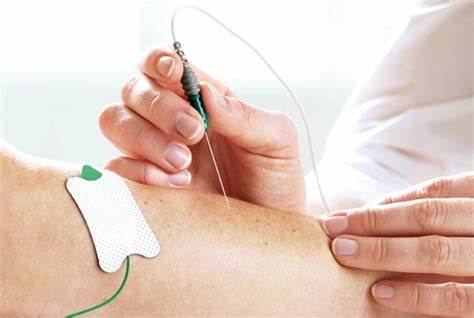
- During the test, one or more little needles (also called electrodes) are inserted through the skin into the muscle.
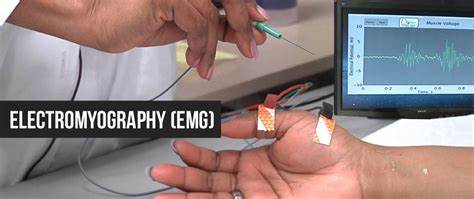
- The electrical activity taken up by the electrodes is then displayed on an oscilloscope (a monitor that displays electrical activity in the form of waves).
- An audio amplifier is used so the activity can be learned.
- Electromyography (EMG) measures the electrical activity of muscle during rest, slight contraction, and forceful contraction.
- Muscle tissue does not commonly produce electrical signals during rest.
- When an electrode is inserted, a brief period of activity can be seen on the oscilloscope, yet after that, no signal should be present.
- After an electrode has been inserted, you may be asked to contract the muscle, for example, like, by lifting or bending your leg.
- The action potential (size and shape of the wave) that this makes on the oscilloscope provides information about the ability of the muscle to respond when the nerves are stimulated.
- As the muscle is contracted more forcefully, more and more muscle fibers are activated, creating action potentials.
- A related procedure that may be performed is a nerve conduction study (NCS).
- Nerve conduction study (NCS) is a measurement of the amount and speed of conduction of an electrical impulse through a nerve.
- Nerve conduction study (NCS) can determine nerve damage and destruction and is often performed at the same time as Electromyography (EMG).
- Both procedures assist to detect the presence, location, and extent of diseases that damage the nerves and muscles.
- Electromyography (EMG) is a diagnostic procedure that assesses the health condition of muscles and the nerve cells that control them.
- Electromyography (EMG) results can help diagnose muscle disorders, nerve disorders, and disorders affecting the connection between nerves and muscles.
- Electromyography (EMG) is a diagnostic procedure that assesses the health condition of muscles and the nerve cells that control them.
- These nerve cells are known as motor neurons.
- They transmit electrical indications that cause muscles to contract and relax.
- An Electromyography (EMG) translates these signals into graphs or numbers, helping doctors to make a diagnosis.
- A doctor will usually order an Electromyography (EMG) when someone is showing symptoms of a muscle or nerve disorder. These symptoms may involve tingling, numbness, or unexplained weakness in the limbs.
- Electromyography (EMG) results can help the doctor diagnose muscle disorders, nerve disorders, and disorders affecting the connection between nerves and muscles.
- Certain doctors may refer to electromyography as an electrodiagnostic exam.
Why is electromyography (EMG) performed?
- Your doctor may perform electromyography (EMG) if you are experiencing symptoms that may indicate a muscle or nerve disorder.
Some symptoms that may call for electromyography (EMG) include:
- tingling
- numbness
- muscle weakness
- muscle pain or cramping
- paralysis
- involuntary muscle twitching (or tics).
- The results of electromyography (EMG) can help your doctor determine the underlying cause of these symptoms.
Possible causes could involve:
- muscle disorders, like as muscular dystrophy
- disorders that affect the ability of the motor neuron to send electrical signals to the muscle, like as myasthenia gravis
- radiculopathies
- peripheral nerve disorders that affect the nerves outside the spinal cord, like as carpal tunnel syndrome
- nerve disorders, such as amyotrophic lateral sclerosis (ALS).
Before the procedure of EMG:
- Your doctor will describe the procedure to you and offer you the opportunity to ask any questions that you might have about the procedure.
- Generally, fasting is not needed previous the test.
- In some cases, cigarettes and caffeinated beverages, such as coffee, tea, and cola may be restricted for two to three hours before testing.
- Inform you are doctor of all medications (prescribed and over-the-counter) and herbal supplements that you are taking.
- Inform you are doctor if you have a pacemaker.
- Dress in clothes that permit access to the area to be tested or that are simply removed.
- Stop using lotions or oils on your skin for a few days previous your procedure, or at least stop using them on the day of the exam.
- Based on your medical condition, your doctor may supplicate other specific preparation.
- Make sure to inform your doctor about any over-the-counter or prescription medications you may be taking.
- It is also the main thing to tell your doctor if you have a bleeding disorder, or if you have a pacemaker or implantable defibrillator.
- You may not be able to have an electromyography(EMG) if you have any of these medical conditions or devices.
If you’re able to have an electromyography (EMG), you should do the following beforehand:
- Avoid smoking for at least three hours previous to the procedure.
- Bathe or take a shower to get rid of any oils from the skin.
- Do not apply any lotions or creams later washing.
- Wear comfortable clothing that does not block the area that your doctor will be evaluating.
- You may be asked to change into a hospital gown right previous the procedure.
What happens during electromyography (EMG)?
- You will be requested to lie down on an examination table or to sit in a reclined chair.
- Your doctor may ask you to move into various positions during the procedure.
There are two components to an electromyography (EMG) test:
The nerve conduction study and needle electromyography (EMG). The nerve conduction study is the 1st part of the procedure. It includes placing small sensors called surface electrodes on the skin to assess the ability of the motor neurons to send electrical signals. The second part of the electromyography (EMG) procedure, known as needle EMG, also uses sensors to evaluate electrical signals.
The sensors are called needle electrodes, and they are directly inserted into muscle tissue to assess muscle activity when at rest and when contracted.
- The nerve conduction study is performed 1st.
- During this portion of the procedure, your doctor will apply several electrodes to the surface of your skin, commonly in the area where you are experiencing symptoms.
- These electrodes will assess how well your motor neurons communicate with your muscles.
- Once the test is complete, the electrodes are pulled off from the skin.
- Later the nerve conduction study, your doctor will perform needle electromyography(EMG).
- Your doctor will 1st clean the affected area with an antiseptic.
- Then, they will use a needle to put electrodes into your muscle tissue.
- You may feel light discomfort or pain while the needle is being inserted.
- The needle electrodes will assess the electrical activity of your muscles when contracted and when at rest.
- These electrodes will be removed later after the test is over.
- During both parts of the electromyography(EMG) procedure, the electrodes will deliver tiny electrical signals to your nerves.
- A computer will translate these gestures into graphs or numerical values that can be interpreted by your doctor.
- The whole procedure should take between 30 and 60 minutes.
Needle electromyography (NEMG)
- Physiologic assessment of diseases of the motor unit from the anterior horn cells (AHCs) to the muscles relies on a combination of needle electromyography (EMG) and nerve conduction studies (NCS).
- Both need a unique combination of knowledge of peripheral nervous system anatomy, physiology, pathophysiology, diseases, techniques, and electricity is necessary.
- Successful, high-quality, reproducible electromyography (EMG) depends on the skills of a clinician in patient interaction during the physical insertion and movement of the needle while recording the electrical signals.
- These must be combined with the skill of analyzing electric signals recorded from muscle by auditory pattern recognition and semi-quantitation.
- This monograph reviews the techniques of needle electromyography (EMG) and waveform analysis and describes the types of electromyography (EMG) waveforms recorded during needle electromyography (EMG).
What are the risks of electromyography?
- Electromyography (EMG) is a very low-risk exam.
- However, you may feel sore in the location that was tested.
- The soreness may last for a particular day and can be relieved with an over-the-counter pain reliever, such as ibuprofen.
- In a few cases, you may experience tingling, bruising, and swelling at the needle insertion sites.
- Make sure to ask your doctor if the swelling or pain becomes worse.
What do my electromyography (EMG) results mean?
- Your doctor may review the results with you right later in the procedure.
- However, if another healthcare provider ordered the electromyography (EMG), then you may not know the results until you attend a follow-up appointment with your doctor.
If your electromyography (EMG) shows any electrical activity in a resting muscle, then you may have:
- a muscle disorder
- a disorder affecting the nerves that connect to the muscle
- inflammation caused by an injury.
- If your electromyography (EMG) shows abnormal electrical activity when a muscle contracts, then you may have a herniated disc or a nerve disorder, such as ALS or carpal tunnel syndrome.
- Depending on your results, your doctor will talk to you about any additional tests or treatments that might be required.
Risks
- electromyography (EMG) is a low-risk procedure, and complications are rare. There is a small risk of bleeding, infection, & nerve injury when a needle electrode is inserted.
- When muscles along the chest wall are examined with a needle electrode, there is a very small risk that it could cause air to leak into the part between the lungs and the chest wall, causing a lung to collapse (pneumothorax).
FAQs
What do I need to know about electromyography?
Electromyography (EMG) is a test that measures the electrical activity of your muscles. Your nerves send signals to your muscles to assist them to move. An EMG will tell your healthcare provider how well your muscles and nerves work together.
What is an EMG test for muscles?
Overview Electromyography (EMG) is a diagnostic procedure to assess the health of muscles and the nerve cells that control them (motor neurons). EMG results can reveal nerve dysfunction, muscle dysfunction, or problems with nerve-to-muscle signal transmission. Motor neurons transmit electrical signals that cause muscles to contract.
How do you prepare for an electromyography test?
Do not have caffeine or smoke for 2 to 3 hours before the test. Do not apply lotions or creams to your skin on the day of the test. Wear loose-fitting clothing to the test. You may be given medicine to help you relax before the test.
What are the risks of electromyography?
What are the risks of electromyography? Your nerves may be injured during the test. You may get an infection. You may develop soreness, bruises, or bleeding where the needles were put into your skin. You have the right to help plan your care.
What will happen during electromyography?
Your healthcare provider will attach sticky pads to your arm or leg. The provider will also insert 1 or more needles through your skin and into your muscle.






3 Comments