Polymyositis
Table of Contents
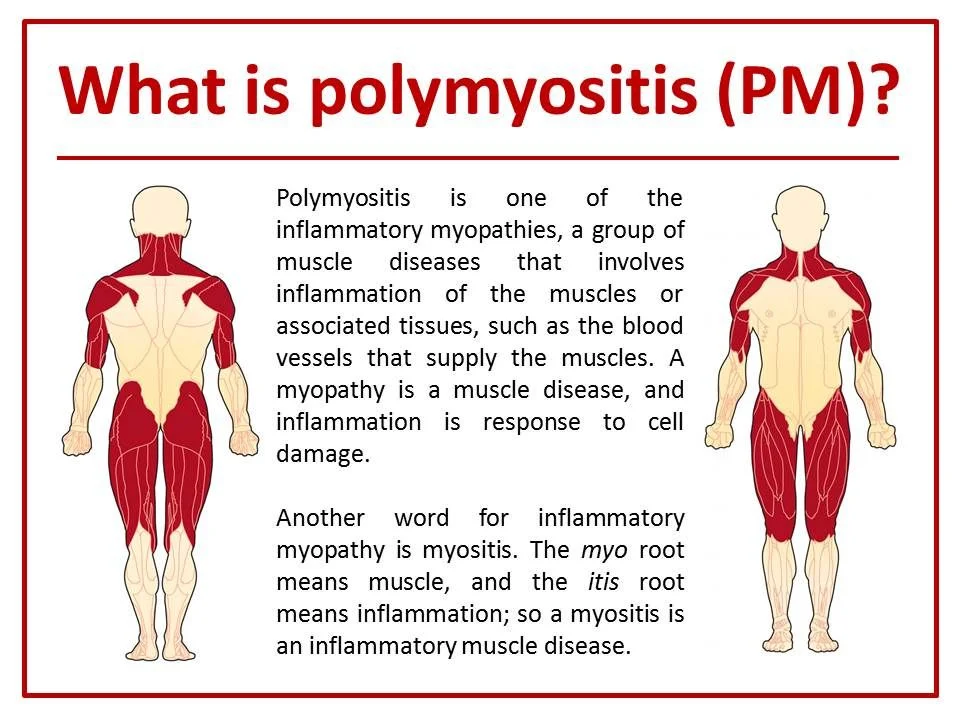
What is polymyositis?
- Polymyositis is an inflammatory muscle disease that causes muscle weakness.
- Myositis means inflammation of the muscle.
- Commonly, polymyositis affects the muscles that are closest to the trunk of the body.
- Eventually, people with polymyositis have trouble when rising from the sitting position, climbing stairs, lifting objects, or reaching overhead.
- In certain cases, muscles that are not close to the trunk of the body become affected as the disease progresses.
- Polymyositis develops gradually over time, & it rarely affects persons younger than the age of 18.
- It is more usual in women (by about 2 (two) to 1 (one) ).
- If the condition is accompanied by an inflammatory process that strikes the skin as well, it is called dermatomyositis.
- Polymyositis can be present in combination with another illness.
- Both polymyositis & dermatomyositis can sometimes be associated with cancers, including lymphoma, breast, lung, ovarian, & colon cancer.
- Polymyositis (pol-e-my-o-SY-tis) is an unusual inflammatory disease that causes muscle weakness affecting both sides of your body.
- Having this condition can make it difficult to climb stairs, rise from a seated position, lift objects or reach overhead.
- Polymyositis most usually affects adults in their 30s, 40s, or 50s.
- Women are affected more sometimes than men.
- Signs & symptoms commonly develop gradually, over weeks or months.
- While there is no prevention for polymyositis, treatment — ranging from medications to physical therapy — can improve your muscle strength & function.
- Polymyositis is a disease that causes the muscles to become irritated & inflamed.
- The muscles eventually start to break down & become weak.
- The condition can affect the muscles all over the body.
- This can make even simple movements difficult.
- Polymyositis is one disease in a group of diseases called inflammatory myopathies.
- Polymyositis is a type of muscle disease called inflammatory myopathy.
- It inflames your muscles & their related tissues, like the blood vessels that supply them.
- It can cause muscle weakness and pain, sometimes on both sides of your body.
- There is no cure for this ongoing (chronic) condition, yet there are treatments that can help with symptoms.
What are the symptoms of polymyositis?
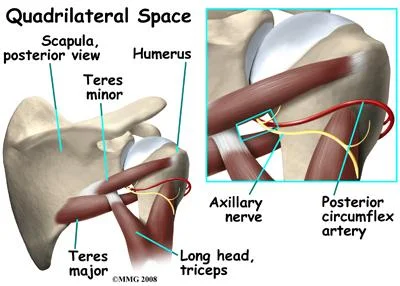
- The muscle weakness associated with polymyositis involves the muscles closest to the trunk, like those in your hips, thighs, shoulders, upper arms & neck.
- The weakness affects both the left & right sides of your body, & tends to gradually worsen.
- The condition affects muscles all over the body, & can affect the ability to run, walk, or lift objects.
- It can too affect the muscles that allow you to eat & breathe.
- The muscles that are closest to the center of the body tend to be affected the most sometimes.
- The symptoms of polymyositis are caused by inflammation in the muscles.
- Muscle weakness affects both sides of the body equally.
- The condition tends to target the muscle groups that are closest to the trunk of the body — the hips, shoulders, thighs, upper arms, upper back, & neck.
- If you have it, you may see you have trouble lifting your arms over your head, walking up flights of stairs, rising from a chair, or carrying things. In certain cases, it may be hard to swallow food, yet this is unusual.
- You may or may not have pain in the parts where the muscles are weak.
- Over time, the muscles may atrophy, meaning they waste away or becomes less bulky.
- The condition sometimes worsens slowly, & you might not notice symptoms for months.
The following are certain symptoms of polymyositis. These symptoms may come & go:
- Muscle weakness: This is the most usual symptom. The muscles involved commonly are those closest to the trunk of the body, and the onset of weakness is commonly gradual, occurring over 3 (three) to 6 (six) months, or rarely the symptoms come on rapidly.
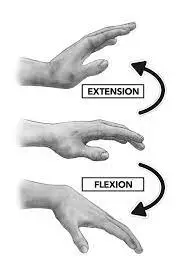
- Difficulty to getting up from chairs, climbing stairs, or lifting objects: Certain people also have trouble getting up after lying down.
- Difficulty in swallowing.
- Muscle ache: In certain cases, muscles ache & are tender to the touch.
- Fatigue.
- Raynaud’s phenomenon: this is a condition in which the fingers or toes become very cold & discolored due to problems with blood flow.
- Shortness of breath due to heart & lung involvement.
- Patchy red or violet rash around the eyes: Certain people also get patchy, red skin over the knuckles, elbows, and knees or a red rash on the neck & upper chest.
- Fever,
- Weight loss,
- Muscle pain and stiffness,
- Muscle weakness: Particularly in the belly (abdomen), shoulders, upper arms, & hips.
- Joint pain & stiffness,
- Trouble catching your breath,
- Irregular heart rhythms, if the heart muscles become inflamed.
- Polymyositis can make it very hard to do everyday things.
- You may notice trouble walking up a flight of stairs, lifting up your arms, or getting out of your chair.
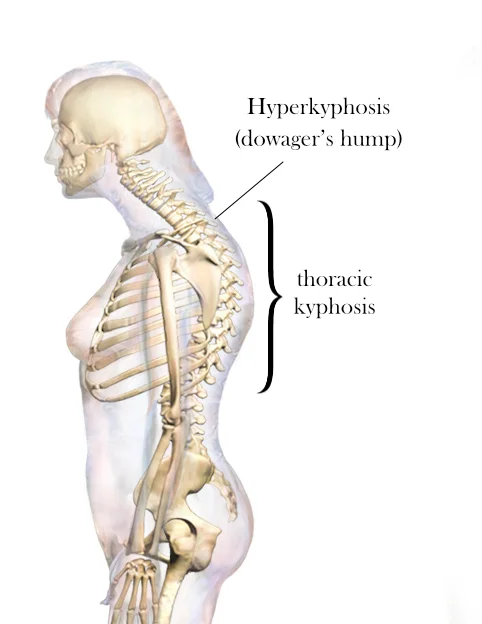
- As inflammation gets worse around the body, pain & weakness may affect the ankles, wrists, & lower arm area.
- Weight loss & poor nutrition may become a problem if muscle weakness leads to trouble eating & swallowing.
What are the causes of polymyositis?
- The cause of polymyositis is not known, yet there are indications that heredity plays a role in the disease.
- Current research suggests that the condition may happen when immune system cells infiltrate & attack muscle tissue (an autoimmune process).
- Research into the workings of the immune system & what causes it to malfunction may result in more knowledge about the causes of polymyositis.
- The exact cause of polymyositis is unknown, yet the disease shares many characteristics with autoimmune disorders, in which your immune system mistakenly attacks your own body tissues.
- The exact cause of polymyositis is not known. It most often occurs in people ages 31 to 60.
- It rarely happens in people younger than 18 (eighteen).
- Experts think that polymyositis may be related to or triggered by a virus or an autoimmune reaction.
- An autoimmune reaction is when the body attacks its own tissues.
- In certain cases, a medicine may lead to an allergic response that causes muscle irritation & damage.
- But in most cases, healthcare providers are not able to find the exact cause of the condition.
- No one knows the exact cause of polymyositis.
- Yet doctors do know that it is an autoimmune condition, which means the body can attack its own tissues.
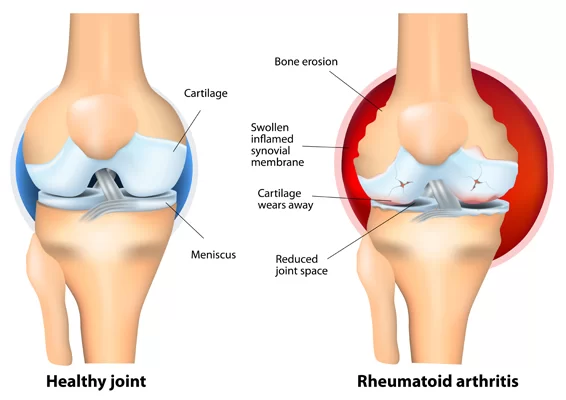
- It is more common in people with other autoimmune diseases like lupus & rheumatoid arthritis.
- It is also more usual among people with HIV.
- Most of the people who have polymyositis get diagnosed between the ages of 30 & 60.
- It is very rare in children, & it affects women more often than men.
What are the risk factors for polymyositis?
Your risk of polymyositis is higher if you have lupus, rheumatoid arthritis, scleroderma, and Sjogren’s syndrome.
Risk factors for polymyositis involve:
- Autoimmune conditions such as:
- Lupus
- Rheumatoid arthritis
- Scleroderma
- Sjogren’s syndrome
- Viral infections like HIV & AIDS
- Diseases that affect your ability to breathe.
How is polymyositis diagnosed?
- There are no easy tests to diagnose polymyositis.
- It sometimes takes time before doctors know for sure you have it.
- The process begins with a health history and a physical exam.
- The exam will involve seeing how strong your muscles are.
- The diagnosis of the disease usually starts with a physician’s exam and blood testing.
- People who have polymyositis sometimes have unusually high levels of muscle enzymes.
- The enzymes are released into the blood by the muscle that is being damaged by inflammation.
- Routine blood & urine tests can check for internal organ abnormalities.
- Chest X-rays, mammograms, PAP smears, and another screening test might be considered to look for signs of the cancers that may arise with polymyositis.
- Additional testing can rule out another condition resembling polymyositis.
- Your doctor will consider your medical history, & your family’s, to rule out another condition.
You may also get tests like as:
- Blood tests: These can assist the doctor spot signs of muscle damage. The process begins with a health history & a physical exam. The exam will involve seeing how strong your muscles are.
- EMG (electromyography): Checks to look if the patterns of electrical impulses in your muscles are normal or not. This may be done to discover abnormal electrical activity in affected muscles. Electromyography (EMG) and nerve conduction velocity (NCV) studies are electrical tests of muscle & nerves that can show abnormal findings typical of polymyositis. These tests also can rule out another nerve-muscle disease. Imaging of the muscles can show parts of muscle inflammation and can be used to find muscle biopsy sites.
- MRI (magnetic resonance imaging): This uses a magnet to scan & create images of large parts of muscles. This test uses large magnets & a computer to see for inflammation in the body.
- Muscle biopsy: Your doctor will take a little sample of your muscle for testing to see if the muscle tissue is inflamed. You may need to get magnetic resonance imaging (MRI) to help your doctor find a good spot to biopsy. Small pieces of tissue are taken to be checked with a microscope. Muscle biopsy is a surgical procedure in which muscle tissue is detached & examined. A muscle biopsy is used to confirm the presence of muscle inflammation common only to polymyositis.
What are the complications of polymyositis?
- If polymyositis is not treated, it can conduct to severe complications.
- As the muscles become weaker, you may fall sometimes and be limited in your daily activities.
- If the muscles in the digestive tract & chest wall are affected, you may have problems breathing (respiratory failure), malnutrition, & weight loss. Polymyositis that is treated but can not be managed well can cause severe disability.
- This includes an inability to swallow or breathe without assistance.
Complications that might come along with polymyositis involve:
- Trouble swallowing: This could occur if the muscles in your esophagus are affected. It can conduct to weight loss & malnutrition. If the muscles in your esophagus are affected, you may have problems swallowing (dysphagia), which in turn may cause weight loss & malnutrition.
- Aspiration pneumonia: When you can not swallow well, you are more likely to breathe food or liquid (including saliva) into your lungs. This can cause pneumonia. Difficulty swallowing may also cause you to breathe food or liquids, involving saliva, into your lungs (aspiration), which can lead to pneumonia.
- Breathing problems: If your chest muscles are pretentious, you could have shortness of breath, or, at worst, respiratory failure.
- If your chest muscles are affected by the disease, you may experience breathing problems, like shortness of breath or, in severe cases, respiratory failure.
How is polymyositis treated?
- Polymyositis is treated with high doses of corticosteroids as the first course of treatment.
- Corticosteroids are given because they can effectively decrease inflammation in the muscles.
- Corticosteroids do not always adequately better polymyositis.
- In these patients, immunosuppressive medications are considered.
- Polymyositis is a chronic condition.
- That means that one time you have it, it sticks around.
- Yet there are ways to help manage it.
- Treatment will relate to your symptoms, your age, & your general health.
- It will also relate to how severe the condition is.
- There is no cure for polymyositis, yet the symptoms can be managed.
- You may require more than 1 kind of treatment.
- And your treatment may require to be changed over time.
- In severe cases, some treatments do not work as well.
Treatments involve:
- Anti-inflammatory medicines: These are steroid medicines or corticosteroids. They do not trouble inflammation in the body. Symptoms generally get better within 4 to 6 weeks.
- Your healthcare provider may lower the dose of steroids later that to ease side effects. Certain people may need to take steroids ongoing to manage the disease and reduce symptoms.
- Methotrexate,
- Azathioprine,
- Cyclophosphamide,
- Chlorambucil,
- Cyclosporine,
- Tacrolimus,
- Mycophenolate,
- Rituximab.
- Immunosuppressive medicines: These are medicines that block or steady down your body’s immune system.
- Physical therapy: This involves special exercises that help to stretch and strengthen the muscles. These can assist keep muscles from shrinking. This will make you stronger and assist you to move better. Physical therapy also is main in the treatment of polymyositis.
- Heat therapy and rest: These can assist ease muscle symptoms.
- Braces or other special devices: These can assist to support muscles and help with movement.
- Speak with your healthcare providers about the risks, benefits, & possible side effects of all medicines.
- In critical cases of polymyositis, the intravenous infusion of immunoglobulins (IVIG) has been an effective treatment.
- Steroids: These assist with muscle inflammation, ease pain, and even increase muscle strength. Yet steroids can have many side effects, so when your doctor prescribes them, they will keep an eye on you. Most people begin with prednisone, but if you have a severe case, the doctor may add methylprednisone, too.
- Drugs that suppress the immune system: You may take these with steroids, or on their own, if steroids do not help. The doctor will probably begin you off with azathioprine or methotrexate.
Ask your doctor about any questions you have, and for another way to make your life easier. With primary medical treatment of the disease and disease flares, patients with polymyositis can do well. The disease often becomes inactive, enabling the patient to focus on muscle rehabilitation.
Associated conditions
- Although these are not complications, polymyositis is sometimes associated with other conditions that may cause further complications of their own, or in combination with polymyositis symptoms.
Associated conditions involve:
- Raynaud’s phenomenon: This is a condition in which your fingers, toes, cheeks, nose & ears initially turn light when exposed to cold temperatures.
- Other connective tissue diseases: Other conditions, such as lupus, rheumatoid arthritis, scleroderma, & Sjogren’s syndrome, can happen in combination with polymyositis.
- Cardiovascular disease: Polymyositis may cause the muscular walls of your heart to suit inflamed (myocarditis). In a little number of people who have polymyositis, congestive heart failure & heart arrhythmias may develop.
- Lung disease: A condition called interstitial lung disease may happen with polymyositis. Interstitial lung disease (ILD) refers to a group of disorders that cause scarring (fibrosis) of lung tissue, making lungs stiff & inelastic. Signs & symptoms involve a dry cough & shortness of breath.
- Cancer: Peoples who have polymyositis have an elevated risk of cancer.