Chronic Obstructive Pulmonary Disease (COPD)
Table of Contents
Key facts
- Chronic obstructive pulmonary disease (COPD) is the 3rd leading cause of death worldwide, causing 3.23 million deaths in 2019.
- Nearly 90% of Chronic obstructive pulmonary disease and COPD deaths in those under 70 years of age happen in low- and middle-income countries (LMIC).
- Early diagnosis & treatment, involving smoking cessation support, is needed to slow the progression of symptoms and reduce flare-ups.
- Environmental exposure to tobacco smoke, indoor air pollution, and occupational specks of dust, fumes, and chemicals are important risk factors for Chronic obstructive pulmonary disease and COPD.
- Chronic obstructive pulmonary disease COPD results from long-term exposure to harmful gases and particles combined with individual factors, including events that influence lung growth in childhood and genetics.
- Chronic obstructive pulmonary disease and COPD cause persistent and progressive respiratory symptoms, involving difficulty in breathing, cough, and phlegm production.
What is Chronic Obstructive Pulmonary Disease (COPD)?
- COPD is a chronic inflammatory lung disease that causes obstructed airflow from the lungs.
- Symptoms involve breathing difficulty, cough, mucus (sputum) production, and wheezing.
- It is typically caused by long-term exposure to irritating gases or particulate matter, most sometimes from cigarette smoke.
- People with Chronic obstructive pulmonary disease (COPD) are at increased risk of developing heart disease, lung cancer, and a variety of other conditions.
- Chronic obstructive pulmonary disease, or COPD, refers to a group of diseases that cause airflow blockage & breathing-related problems.
- It includes emphysema and chronic bronchitis. Chronic obstructive pulmonary disease and COPD make breathing difficult for the 16 million Americans who have this disease.
- Millions more people suffer from Chronic obstructive pulmonary disease COPD, but have not been diagnosed and are not being treated.
- Although there is no cure for Chronic obstructive pulmonary disease and COPD, it can be treated.
- Emphysema and chronic bronchitis are the two most common conditions that contribute to Chronic obstructive pulmonary disease (COPD).
- These two conditions usually occur together and can vary in severity among individuals with Chronic obstructive pulmonary disease (COPD).
- Chronic bronchitis is inflammation of the lining of the bronchial tubes, which carry air to & from the air sacs (alveoli) of the lungs.
- It is characterized by everyday cough & mucus (sputum) production.
- Emphysema is a condition in which the alveoli at the end of the tiniest air passages (bronchioles) of the lungs are destroyed as a result of damaging exposure to cigarette smoke and other irritating gas and particulate matter.
- Although Chronic obstructive pulmonary disease (COPD) is a progressive disease that gets worse over time, Chronic obstructive pulmonary disease (COPD) is treatable.
- With proper management, most people with Chronic obstructive pulmonary disease (COPD) can achieve good symptom control and quality of life, as well as reduced risk of other associated conditions.
- Chronic obstructive pulmonary disease (COPD) is a usual, preventable and treatable chronic lung disease that affects men and women worldwide.
- Abnormalities in the little airways of the lungs lead to limitation of airflow in and out of the lungs.
- Several processes cause the airways to become small. There may be the destruction of parts of the lung, mucus blocking the airways, & inflammation & swelling of the airway lining.
- Chronic obstructive pulmonary disease (COPD) is sometimes called emphysema or chronic bronchitis.
- Chronic obstructive pulmonary disease COPD, or chronic obstructive pulmonary disease, is a progressive disease, which means it gets worse over time.
- With Chronic obstructive pulmonary disease COPD, less air flows in and out of the airways, making it hard to breathe.
- In the United States, Chronic obstructive pulmonary disease COPD affects more than 15 million adults, and many more do not know they have it. More than 1/2 of those diagnosed are women.
- Chronic obstructive pulmonary disease and COPD is a major causes of disability, and it is the fourth leading cause of death in the United States according to the Centers for Disease Control & Prevention (CDC).
- The good news is that Chronic obstructive pulmonary disease COPD can often be prevented, mainly by not smoking.
- Cigarette smoking is the leading cause of Chronic obstructive pulmonary disease COPD.
- Most people who have Chronic obstructive pulmonary disease COPD smoke or used to smoke.
- However, up to 30% of people with Chronic obstructive pulmonary disease COPD never smoked.
- A rare genetic condition called alpha-1 antitrypsin (AAT) deficiency can cause the disease.
In the United States, the term Chronic obstructive pulmonary disease COPD includes two main conditions.
- Emphysema develops when there is damage to the walls between many of the air sacs in the lungs. Commonly, these sacs are elastic or stretchy. When you breathe in, each air sac fills up with air, like a little balloon. When you breathe out, the air sacs deflate, & the air goes out. In emphysema, it is harder for your lungs to action air out of your body.
- Chronic (long-term) bronchitis is caused by repeated or continuous irritation & inflammation in the lining of the airways. Lots of broad mucus forms in the airways, making it hard to breathe. Most people who have Chronic obstructive pulmonary disease and COPD have both emphysema and chronic bronchitis, but how serious each condition varies from person to person.
- Chronic obstructive pulmonary disease COPD can cause coughing that produces large amounts of a slimy substance called mucus.
- It can also cause problems breathing, shortness of breath, chest tightness, & other symptoms.
- Symptoms of Chronic obstructive pulmonary disease COPD often develop slowly but worsen over time, and they can limit your ability to do routine activities.
- Serious Chronic obstructive pulmonary disease COPD may prevent you from doing even basic activities like walking, cooking, or taking care of yourself.
- Although there are no cure, treatments and lifestyle changes such as quitting smoking can help you feel better, stay more active, and slow the progress of the disease.
- You may also require oxygen therapy, pulmonary rehabilitation, or medicines to treat complications.
- Emphysema usually refers to the destruction of the small air sacs at the end of the airways in the lungs.
- Chronic bronchitis refers to chronic cough with the production of phlegm resulting from inflammation in the airways.
- Chronic obstructive pulmonary disease (COPD) and asthma share common symptoms (cough, wheezing, and difficulty breathing), and people may have both conditions.
- Chronic obstructive pulmonary disease usually referred to as COPD, is a group of progressive lung diseases.
- The most usual of these diseases are emphysema and chronic bronchitis.
- Many people with Chronic obstructive pulmonary disease (COPD) have both of these conditions.
- Emphysema steadily destroys air sacs in your lungs, which interferes with outward airflow.
- Bronchitis causes inflammation and little of the bronchial tubes, which allows mucus to build up.
- It is estimated that about 30 million people in the United States have Chronic obstructive pulmonary disease (COPD).
- As many as 1/2 are unaware that they have it.
- Untreated, Chronic obstructive pulmonary disease (COPD) can lead to a faster progression of the disease, heart problems, and worsening respiratory infections.
- Chronic obstructive pulmonary disease (COPD), which involves emphysema and chronic bronchitis, makes breathing hard for the 16 million Americans diagnosed with it.
- Millions more suffer from Chronic obstructive pulmonary disease COPD yet have not been diagnosed and are not being treated. Chronic obstructive pulmonary disease COPD can limit your ability to work or even do simple daily tasks.
- Chronic obstructive pulmonary disease and COPD can also make you more likely to get severely ill from COVID-19.
- The leading cause of Chronic obstructive pulmonary disease COPD is tobacco smoke, so if you smoke or are used to smoking, you are at a higher risk of having Chronic obstructive pulmonary disease COPD.
- Exposure to air pollution in the home or at work, family history, and respiratory infections like pneumonia increase your risk.
What are the symptoms of Chronic obstructive pulmonary disease (COPD)?
- Chronic obstructive pulmonary disease (COPD) makes it harder to breathe.
- Symptoms may be mild at 1st, beginning with intermittent coughing and shortness of breath.
- As it progresses, symptoms can become more constant and it can become increasingly hard to breathe.
- You may experience wheezing & tightness in the chest or have severe sputum production.
- Some people with Chronic obstructive pulmonary disease (COPD) have acute exacerbations, which are flare-ups of severe symptoms.
- As Chronic obstructive pulmonary disease (COPD) progresses, people find it more difficult to carry out their normal daily activities, often due to breathlessness.
- There may be a considerable financial burden due to limitations of the workplace and home productivity, and costs of medical treatment.
- During flare-ups, people with Chronic obstructive pulmonary disease (COPD) find their symptoms become much worse & they may need to receive extra treatment at home or be admitted to a hospital for emergency care. Severe flare-ups can be life-threatening.
- People with Chronic obstructive pulmonary disease (COPD) often have other medical conditions such as heart disease, osteoporosis, musculoskeletal disorders, lung cancer, depression, & anxiety.
- Chronic obstructive pulmonary disease (COPD) symptoms often do not appear until significant lung damage has occurred, & they usually worsen over time, particularly if smoking exposure continues.
Signs and symptoms of Chronic obstructive pulmonary disease (COPD) may include:
- Shortness of breath, especially during physical activities
- Wheezing
- Chest tightness
- A chronic cough that may construct mucus (sputum) that may be clear, white, yellow, or greenish
- Frequent respiratory infections
- Lack of energy
- Unintended weight loss (in later stages)
- Swelling in ankles, feet, or legs.
- People with Chronic obstructive pulmonary disease (COPD) are also likely to experience episodes called exacerbations, during which their symptoms become worse than the usual day-to-day variation and persist for at least several days.
Early symptoms
- At first, symptoms of Chronic obstructive pulmonary disease (COPD) can be quite mild. You might mistake them for a cold.
Early symptoms involve:
- occasional shortness of breath, especially later exercise
- mild yet recurrent cough
- needing to clear your throat sometimes, especially 1st thing in the morning
- You might begin making subtle changes, like avoiding stairs & skipping physical activities.
Worsening symptoms
Symptoms can get progressively worse & harder to ignore. As the lungs become more harmed, you may experience:
- shortness of breath, and later even mild forms of exercise like walking up a flight of stairs
- wheezing, which is a type of higher-pitched noisy breathing, especially during exhalations
- chest tightness
- chronic cough, with or without mucus
- require to clear mucus from your lungs every day
- frequent colds, flu, or another respiratory infection
- lack of energy
In the later stages of Chronic obstructive pulmonary disease (COPD), symptoms may also include:
- fatigue
- swelling of the feet, ankles, or legs
- weight loss
- Symptoms are likely to be much worse if you presently smoke or are regularly exposed to secondhand smoke.
What causes COPD?
- Most people with Chronic obstructive pulmonary disease (COPD) are at least 40 years old and have at least some history of smoking.
- The longer and more tobacco products you smoke, the greater your risk of Chronic obstructive pulmonary disease (COPD).
- In addition to cigarette smoke, cigar smoke, pipe smoke, and secondhand smoke can cause Chronic obstructive pulmonary disease (COPD).
- Your risk of Chronic obstructive pulmonary disease (COPD) is even greater if you have asthma and smoke.
- The main cause of Chronic obstructive pulmonary disease (COPD) in developed countries is tobacco smoking.
- In the developing world, Chronic obstructive pulmonary disease (COPD) often occurs in people exposed to fumes from burning fuel for cooking and heating in poorly ventilated homes.
- Only some chronic smokers develop clinically apparent Chronic obstructive pulmonary disease (COPD), although many smokers with long smoking histories may develop reduced lung function.
- Some smokers develop less common lung conditions.
- They may be misdiagnosed as having Chronic obstructive pulmonary disease (COPD) until a more thorough evaluation is performed.
Other causes
- You can also develop Chronic obstructive pulmonary disease COPD if you are exposed to chemicals and fumes in the workplace.
- Long-term exposure to air pollution and inhaling dust can also cause Chronic obstructive pulmonary disease COPD.
- In developing countries, along with tobacco smoke, homes are sometimes poorly ventilated, forcing families to breathe fumes from burning fuel used for cooking and heating.
- There may be a genetic predisposition to developing Chronic obstructive pulmonary disease COPD.
- Up to an estimated 5 percent, of a trusted source of people with Chronic obstructive pulmonary disease, COPD has a deficiency in a protein called alpha-1-antitrypsin.
- This deficiency causes the lungs to deteriorate and also can harm the liver. There may be another associated genetic factor at play as well.
Stages of COPD- according to symptoms:
Mild COPD – Symptoms of chronic cough and sputum production may be present, yet not always. At this stage, the individual is commonly unaware that his or her lung function is abnormal.
Moderate COPD- shortness of breath commonly developing on exertion and cough and sputum may be present. This is the stage at which patients commonly seek medical attention because of chronic respiratory symptoms or an exacerbation of their disease.
Severe COPD– greater shortness of breath, reduced exercise capacity, fatigue, and repeated exacerbations that almost always have an impact on the patient’s quality of life.
Very Severe COPD –the presence of chronic respiratory failure
What are the risk factors?
Chronic obstructive pulmonary disease (COPD) develops gradually over time, often resulting from a combination of risk factors:
- tobacco exposure from active smoking or passive exposure to second-hand smoke,
- occupational exposure to specks of dust, fumes, or chemicals,
- indoor air pollution: biomass fuel (wood, animal dung, crop residue) or coal is frequently used for cooking & heating in low- & middle-income countries with high levels of smoke exposure,
- early life events like as poor growth in utero, prematurity, & frequent or severe respiratory infections in childhood that prevent maximum lung growth,
- asthma in childhood, &
- a rare genetic condition called alpha-1 antitrypsin deficiency, which can cause Chronic obstructive pulmonary disease and COPD at a young age.
- Exposure to tobacco smoke: The most significant risk factor for Chronic obstructive pulmonary disease COPD is long-term cigarette smoking. The more years you smoke & the more packs you smoke, the greater your risk. Pipe smokers, cigar smokers, & marijuana smokers also may be at risk, as well as people exposed to great amounts of secondhand smoke.
- People with asthma: Asthma, a chronic inflammatory airway disease, may be a risk factor for developing Chronic obstructive pulmonary disease COPD. The combination of asthma and smoking increases the risk of Chronic obstructive pulmonary disease COPD even more.
- Occupational exposure to specks of dust and chemicals: Long-term exposure to chemical fumes, vapors, and specks of dust in the workplace can irritate and inflame your lungs.
- Exposure to fumes from burning fuel: In the developing world, people exposed to fumes from burning fuel for cooking & heating in poorly ventilated homes are at higher risk of developing Chronic obstructive pulmonary disease and COPD.
- Genetics: The uncommon genetic disorder alpha-1-antitrypsin deficiency is the cause of some cases of Chronic obstructive pulmonary disease COPD. Other genetic factors likely make some smokers more susceptible to the disease.
What is the Diagnosing of Chronic obstructive pulmonary disease COPD?
- There is no single test for Chronic obstructive pulmonary disease COPD. Diagnosis is based on symptoms, a physical exam, & diagnostic test results. When you meet the doctor, be sure to mention all of your symptoms.
Tell your doctor if:
- you are a smoker or have smoked in the past
- you are exposed to lung irritants on the job
- you are exposed to a lot of secondhand smoke
- you have a family history of Chronic obstructive pulmonary disease COPD
- you have asthma or other respiratory conditions
- you take over-the-counter or prescription medications.
Exam and tests
- During the physical exam: your doctor will use a stethoscope to hear your lungs as you breathe. Based on all this information, your doctor may order certain of these tests to get a more complete picture:
- Spirometry is a noninvasive test to assess lung function: During the test, you will take a deep breath and then blow into a tube connected to the spirometer.
- Imaging tests: like a chest X-ray or CT scan. These images can provide a detailed see of your lungs, blood vessels, & heart.
- An arterial blood gas test: This includes taking a blood sample from an artery to measure your blood oxygen, carbon dioxide, & other important levels.
- These tests can help determine if you have Chronic obstructive pulmonary disease COPD or a different condition, such as asthma, restrictive lung disease, or heart failure.
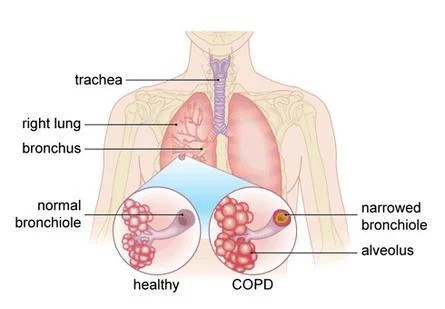
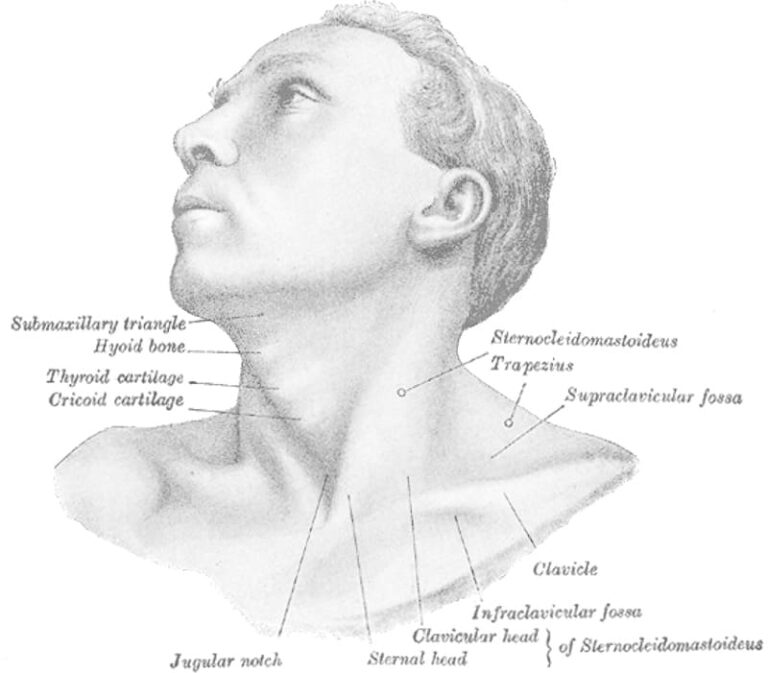
How your lungs are affected?
- Air travels down your windpipe (trachea) & into your lungs through two large tubes (bronchi). Inside your lungs, these tubes divide many times — like the branches of a tree — into many more tin tubes (bronchioles) that end in clusters of tiny air sacs (alveoli).
- The air sacs have very thin walls full of small blood vessels (capillaries).
- The oxygen in the air you inhale passes into these blood vessels & goes into your bloodstream.
- At the same time, carbon dioxide (CO2) — a gas that is an unused product of metabolism — is exhaled.
- Your lungs depend on the natural elasticity of the bronchial tubes & air sacs to force air out of your body.
- Chronic obstructive pulmonary disease COPD causes them to lose their elasticity and over-expand, which leaves some air trapped in your lungs when you exhale.
Causes of airway obstruction
Causes of airway obstruction involve:
Emphysema: This lung disease causes the demolition of the fragile walls & elastic fibers of the alveoli. Tiny airways collapse when you exhale, impairing airflow out of your lungs.
Chronic bronchitis: In this condition, your bronchial tubes become inflamed & narrowed & your lungs produce more mucus, which can further block the little tubes. You develop a chronic cough trying to clear & crystal your airways.
Cigarette smoke & other irritants
- In the vast majority of people with Chronic obstructive pulmonary disease COPD, the lung damage that leads to Chronic obstructive pulmonary disease COPD is caused by long-term cigarette smoking.
- But there are likely other factors at play in the development of Chronic obstructive pulmonary disease COPD, such as a genetic susceptibility to the disease, because not all smokers develop Chronic obstructive pulmonary disease COPD.
- Other irritants can cause Chronic obstructive pulmonary disease COPD, including cigar smoke, secondhand smoke, pipe smoke, air pollution, and workplace exposure to dust, smoke, or fumes.
Alpha-1-antitrypsin deficiency
- In about 1% of people with Chronic obstructive pulmonary disease COPD, the disease results from a genetic disorder that causes low levels of a protein called alpha-1-antitrypsin (AAT). it is made in the liver & secreted into the bloodstream to assist protect the lungs. Alpha-1-antitrypsin (AAT) deficiency can cause liver disease, lung disease, or both.
- For adults with Chronic obstructive pulmonary disease COPD related to AAt deficiency, treatment options include those used for people with more-common types of Chronic obstructive pulmonary disease COPD. In addition, certain people can be treated by replacing the missing AAt protein, which may prevent further damage to the lungs.
What are the Complications of Chronic obstructive pulmonary disease COPD?
Chronic obstructive pulmonary disease COPD can cause many complications, including:
- Respiratory infections: People with Chronic obstructive pulmonary disease COPD are more likely to catch colds, the flu, and pneumonia. Any respiratory infection can make it much harder to breathe & could cause further damage to lung tissue.
- Heart problems: For reasons that are not fully understood, Chronic obstructive pulmonary disease and COPD can increase your risk of heart disease, including heart attack.
- Lung cancer: People with Chronic obstructive pulmonary disease and COPD have a higher risk of developing lung cancer.
- High blood pressure in lung arteries: Chronic obstructive pulmonary disease COPD may cause high blood pressure in the arteries that bring blood to your lungs (pulmonary hypertension).
- Depression: Difficulty breathing can retain you from doing activities that you enjoy. And dealing with a serious illness can give to the development of depression.
What is the Prevention of Chronic obstructive pulmonary disease COPD?
- Unlike some diseases, Chronic obstructive pulmonary disease COPD typically has a clear cause and a clear path of prevention, & there are ways to slow the progression of the disease.
- The majority of cases are directly related to cigarette smoking, and the best way to prevent Chronic obstructive pulmonary disease COPD is to never smoke — or to stop smoking now.
- If you are a longtime smoker, these simple statements may not seem so simple, especially if you have tried quitting — once, twice, or many times before. Yet keep trying to quit.
- It is critical to find a tobacco cessation program that can assist you to quit for good. It is your best chance for reducing damage to your lungs.
- Occupational exposure to chemical fumes and specks of dust is another risk factor for Chronic obstructive pulmonary disease COPD.
- If you work with these types of lung irritants, talk to your supervisor about the best ways to protect yourself, like using respiratory protective equipment.
Here are some steps you can take to help prevent complications associated with Chronic obstructive pulmonary disease COPD:
- Quit smoking to assist reduce your risk of heart disease and lung cancer.
- Get an annual flu vaccination and regular vaccination against pneumococcal pneumonia to reduce your risk of or prevent certain infections.
- Talk to your doctor if you feel sad or helpless or think that you may be experiencing depression.
Reducing the burden of Chronic obstructive pulmonary disease COPD
- There is no cure for Chronic obstructive pulmonary disease COPD, but early diagnosis & treatment are important to slow the progression of symptoms and reduce the risk of flare-ups.
- Chronic obstructive pulmonary disease COPD should be suspected if a person has typical symptoms, and the diagnosis is confirmed by a breathing test called spirometry, which measures how the lungs are working.
- In low- and middle-income countries, spirometry is sometimes not available and so the diagnosis may be missed.
There are several actions that people with Chronic obstructive pulmonary disease COPD can take to improve their overall health and help control their Chronic obstructive pulmonary disease COPD:
- stop smoking: people with Chronic obstructive pulmonary disease and COPD should be offered support to quit smoking.
- take regular exercise, and
- get vaccinated against pneumonia, influenza, and coronavirus.
- Inhaled medication can be used to improve the symptoms & reduce flare-ups.
- There are different types of inhaled medication that work in different ways and can be given in combination with inhalers, if available.
- Certain inhalers open the airways & may be given regularly to prevent or reduce symptoms, & to relieve symptoms during acute flare-ups. Inhaled corticosteroids are often given in combination with these to reduce inflammation in the lungs.
- Inhalers must be taken using the correct technique, and in certain cases with a spacer device to help deliver the medication into the airways more effectively.
- Access to inhalers is limited in many low- & middle-income countries; in 2021 salbutamol inhalers were generally available in public primary healthcare facilities in half of low- and low-middle-income countries.
- Flare-ups are often caused by a respiratory infection, and people may be given an antibiotic or steroid tablets in addition to inhaled or nebulized treatment as needed.
- People living with Chronic obstructive pulmonary disease (COPD) must be given information about their condition, treatment, and self-care to help them to stay as active and healthy as possible.
What is the Treatment for Chronic obstructive pulmonary disease COPD?
- Treatment can ease symptoms, prevent complications, & commonly slow disease progression. Your healthcare team may involve a lung specialist (pulmonologist) & physical and respiratory therapists.
Oxygen therapy
- If your blood oxygen level is too low, you can receive supplemental oxygen through a mask or nasal cannula to assist you to breathe better. A portable unit can conduct it easier to get around.
Surgery
- Surgery is reserved for severe Chronic obstructive pulmonary disease COPD or when other treatments have failed, which is more likely when you have a form of severe emphysema.
- There are two types of surgery.
- The first type of surgery is called bullectomy. During this whole procedure, surgeons remove large, abnormal air spaces (bullae) from the lungs.
- The other one is lung volume reduction surgery, which removes damaged upper lung tissue. Lung volume reduction surgery can be effective at improving breathing, yet few patients undergo this major, somewhat risky procedure.
- Lung transplantation is an option in certain cases. Lung transplantation can effectively cure Chronic obstructive pulmonary disease COPD but has many risks.
- There is a less invasive method of improving the efficiency of airflow in people with severe emphysema called endobronchial valves (EBV), which are one-way valves that divert inspired air to healthy lungs & away from non-functioning, damaged lungs.
- In 2018, an EBV device called the Zephyr Endobronchial Valve Trusted Source was approved by the FDA & has been shown to improve lung function, exercise capacity, and quality of life for patients living with emphysema.
Lifestyle changes
- Certain lifestyle changes may also assist alleviate your symptoms or provide relief.
- If you smoke, quit. Your doctor can recommend appropriate products or support services.
- Whenever possible, avoid secondhand smoke & chemical fumes.
- Get the nutrition your body needs. Work with your doctor or dietician to make a healthy eating plan.
- Tell your doctor about how much exercise is safe for you.
Medications for COPD
- Medications can decrease symptoms & cut down on flare-ups.
It may take certain trial and error to find the medication and dosage that works best for you, but these are some of your options:
- Inhaled bronchodilators: Medicines called bronchodilators help loosen tight muscles in your airways. They are generally taken through an inhaler or nebulizer. Short-acting bronchodilators last from four to six hours. You only use them when you require them. For ongoing symptoms, there are long-acting versions you can utilize every day. They last about twelve hours. For people with Chronic obstructive pulmonary disease and COPD who experience shortness of breath or trouble breathing during exercise, the American Thoracic Society strongly recommends a long-acting beta-agonist (LABA) combined with a long-acting muscarinic antagonist (LAMA). These bronchodilators work by relaxing tightened muscles in the airways, which broads your airways for better air passage. They also assist your body clear mucus from the lungs. These two types of bronchodilators can be taken in combination with an inhaler or with a nebulizer.
Here is a list of recommended LABA/LAMA bronchodilator therapies:
- aclidinium/formoterol
- glycopyrrolate/formoterol
- tiotropium/olodaterol
- umeclidinium/vilanterol
- Corticosteroids.
- Long-acting bronchodilators are typically combined with inhaled glucocorticosteroids. A glucocorticosteroid can decrease inflammation in the airways & lower mucus production.
- The long-acting bronchodilator can relax the airway muscle to assist the airways to stay wider. Corticosteroids are too available in pill form.
Phosphodiesterase-4 inhibitors: This type of medication can be taken in pill form to assist reduce inflammation and relax the airways. It is generally prescribed for severe Chronic obstructive pulmonary disease and COPD with chronic bronchitis.
Theophylline: This medication eases chest tightness & shortness of breath. It may also assist prevent flare-ups. It is available in pill form.
Theophylline is an older medication that relaxes the muscle of the airways, & it may cause side effects. It is generally not a first-line treatment for Chronic obstructive pulmonary disease COPD therapy.
Antibiotics and antivirals: Antibiotics or antivirals may be prescribed when you develop some respiratory infections.
Vaccines: To lower the risk of other respiratory infections, ask your doctor if you should get a yearly flu shot, pneumococcal vaccine, and a tetanus booster that includes protection from pertussis (whooping cough).
Diet recommendations for people with Chronic obstructive pulmonary disease COPD
- There is no specific diet for Chronic obstructive pulmonary disease COPD, but a healthy diet is important for maintaining overall health.
- The stronger you are, the more able you will be to prevent complications & other health problems.
Choose a different of nutritious food from these groups:
- vegetables
- fruits
- grains
- protein
- dairy.
- Also, remember to go easy on the salt. It causes the body to retain water, which can strain breathing.
Liquids
- Drink plenty of fluids. Drinking at least six to eight 8-ounce glasses of non-caffeinated liquids a day can assist keep mucus thinner. This may construct the mucus easier to cough out.
- Limit caffeinated beverages because they can interfere with the medications. If you have heart problems, you may require to drink less, so talk to your doctor.
Weight management
- Maintaining a healthy weight is important. It takes more energy to breathe when you have Chronic obstructive pulmonary disease COPD, so you might need to take in more calories. But if you are overweight, your lungs & heart may have to work harder.
- If you are underweight or frail, even basic body maintenance can become difficult. Overall, having Chronic obstructive pulmonary disease and COPD weakens your immune system and decreases your ability to fight off infection.
Eating habits
A full stomach makes it harder for your lungs to expand, leaving you with shortness of breath. If you find that this happens to you, try these remedies:
- Clear your airways about an hour previous a meal.
- Take little bites of food that you chew slowly before swallowing.
- Swap 3 meals a day for five or six smaller meals.
- Save fluids until the end so you feel a little full during the meal.
Living with Chronic obstructive pulmonary disease COPD
- Chronic obstructive pulmonary disease COPD requires lifelong disease management. That means following the advice of your healthcare team & maintaining healthy lifestyle habits.
- Since your lungs are weakened, you will want to avoid anything that might overtax them or cause a flare-up. Here is a list of things to consider as you adjust your lifestyle.
- Avoid smoking: If you are having trouble quitting, tell your doctor about smoking cessation programs. Try to avoid secondhand smoke, chemical fumes, air pollution, & dust.
- Work out: A little exercise each day can assist you to stay strong. Tell your doctor about how much exercise is good for you.
- Eat a diet of nutritious foods: Avoid highly processed foods that are loaded with calories and salt, yet lack nutrients.
- Treating other conditions: If you have other chronic diseases along with Chronic obstructive pulmonary disease and COPD, it is important to manage those as well, particularly diabetes mellitus & heart disease.
- Clean house: Clear the clutter & streamline your home so that it takes less energy to clean & do other household tasks. If you have advanced Chronic obstructive pulmonary disease COPD, get help with daily chores.
- Be prepared for flare-ups: Carry your emergency contact information with you & post it on your refrigerator. Involve information about what medications you take, as well as the doses. Program emergency numbers into your phone.
- Find support: It can be a relief to tell others who understand. Consider joining a support group. The Chronic obstructive pulmonary disease COPD Foundation provides a comprehensive list of organizations and resources for people living with Chronic obstructive pulmonary disease COPD.
An effective Chronic obstructive pulmonary disease COPD management plan includes four components:
- assess and monitor disease,
- reduce risk factors,
- manage stable Chronic obstructive pulmonary disease COPD,
- manage exacerbations.
Assess & monitor disease:
- A clinical diagnosis of Chronic obstructive pulmonary disease COPD should be considered in any patient who has dyspnoea, chronic cough or sputum production, and /or a history of exposure to risk factors for the disease. The diagnosis should be confirmed by spirometry.
Reduce risk factors:
- Tobacco smoke, occupational exposures, indoor and outdoor air pollution, and irritants are various risk factors for Chronic obstructive pulmonary disease COPD. Reductions of total personal exposure to these risk factors are important goals to prevent the onset and progression of Chronic obstructive pulmonary disease COPD.
(a)Tobacco smoke –
- Healthcare workers should encourage all patients who smoke to quit, even those patients who come to the healthcare provider for unrelated reasons and do not have symptoms of Chronic obstructive pulmonary disease COPD. Counseling delivered by physicians and other health professionals significantly increases quit rates over self-initiated strategies. Pharmacotherapy is recommended in persons when counseling is not sufficient to assist patients to quit smoking.
- The Ministry of Health and Family Welfare, Government of India has launched National Tobacco Control Programme with the objective to bring about greater awareness about the difficult effects of tobacco use.
- With the involvement of mobile technology mCessation Programme- QUIT TOBACCO FOR LIFE “is initiated to reach out and support tobacco users of all categories who want to quit tobacco use.
(b)Occupational exposure –
- The important emphasis should be on primary prevention, which is best achieved by the elimination or reduction of exposure to various substances in the workplace. Secondary prevention, achieved through surveillance and early case detection, is of great importance.
(c) Indoor and outdoor air pollution-
- Reduction of exposure to smoke from biomass fuel, particularly among women & children, is a crucial goal to reduce the prevalence of Chronic obstructive pulmonary disease COPD worldwide. Public policy to reduce vehicle and industrial emissions to safe levels is an urgent priority to reduce the development of Chronic obstructive pulmonary disease COPD.
Manage stable Chronic obstructive pulmonary disease COPD:
- The overall approach to managing stable Chronic obstructive pulmonary disease COPD should be individualized to manage symptoms and thereby improvement in the quality of life. The approach consists of health education, medications, pulmonary rehabilitation, oxygen therapy, ventilatory support, and surgical treatment.
(I) Health education- For patients with Chronic obstructive pulmonary disease COPD, health education can play a role in improving skills, ability to cope with illness, and health status. It is effective in accomplishing some goals, including smoking cessation. Education also improves patient response to exacerbations.
(ii) Pharmacologic treatment- Pharmacologic therapy is used to cure and control symptoms, reduce the frequency and severity of exacerbations, improve health status, and improve exercise tolerance.
(A) Bronchodilators (medications that cause widening of the airway) are given on an as-needed basis or on a regular basis to prevent or reduce symptoms.
(B) Glucocorticosteroids: The role of Glucocorticosteroids in the management of stable Chronic obstructive pulmonary disease COPD is limited to specific indications.
(C) Other pharmacological treatments-
Vaccines- Influenza vaccines containing killed or live, inactivated viruses are recommended for Chronic obstructive pulmonary disease COPD cases. The pneumococcal polysaccharide vaccine is recommended for Chronic obstructive pulmonary disease COPD patients 65 years and older.
Alpha-1 antitrypsin augmentation therapy- It may be used in young patients with increased hereditary alpha-1 antitrypsin deficiency and established emphysema.
Antibiotics- antibiotics should be used for treating infectious exacerbations of Chronic obstructive pulmonary disease COPD and other bacterial infections.
Mucolytic (microkinetic, mucoregulator) agents- Although some patients with viscous sputum may benefit from mucolytics, the overall benefits seem to be very small. Widespread use of these agents is not recommended.
Antitussives- Cough, has a significant protective role, thus the regular use of antitussives is not recommended in stable Chronic obstructive pulmonary disease COPD.
(iii) Non-pharmacologic treatment-
(a) Rehabilitation- Comprehensive pulmonary rehabilitation program involves exercise training, nutrition counseling, and education.
Exercise training- All patients with Chronic obstructive pulmonary disease COPD benefit from exercise training programs, improving with respect to both exercise tolerance and symptoms of dyspnoea and fatigue.
(b)Nutrition counseling- Nutritional state is an important determinant of symptoms, disability, and prognosis in Chronic obstructive pulmonary disease COPD; both overweight and underweight can be a problem.
(iv) Oxygen Therapy- Oxygen therapy, is one of the principal nonpharmacologic treatments for patients with Severe Chronic obstructive pulmonary disease COPD. It can be administered in three ways: long-term continuous therapy, during exercise, and to relieve acute dyspnoea. The long-term administration of oxygen (O2) (> 15 h per day) to patients with chronic respiratory failure has been shown to increase survival.
(v) Ventilatory support- Noninvasive ventilation (using either negative or positive pressure devices) is now widely used to treat acute exacerbations of Chronic obstructive pulmonary disease COPD.
(vi) Surgical treatment-
- Bullectomy
- Lung volume reduction surgery (LVRS)
- Lung transplantation.
(vii) Manage exacerbations:
- Exacerbations of respiratory symptoms requiring medical intervention are important clinical phases in Chronic obstructive pulmonary disease COPD. The most common causes of an exacerbation are infection of the tracheobronchial tree and air pollution, yet the cause of approximately one-third of severe exacerbations cannot be identified.
- Inhaled bronchodilators (particularly inhaled B2-agonists or anticholinergics), theophylline, and systemic, preferably oral, glucocorticosteroids are effective for treatments for acute exacerbations of Chronic obstructive pulmonary disease COPD.
- Patients experiencing Chronic obstructive pulmonary disease COPD exacerbations with clinical signs of airway infection (e.g., increased volume and change of color of sputum, or fever) may benefit from antibiotic treatment.
- Noninvasive positive pressure ventilation (NIPPV) in acute exacerbations improves blood gases and pH (a measure of acidity and alkalinity), reduces in-hospital mortality, decreases the requirement for invasive mechanical ventilation and intubation, and decreases the length of hospital stay.
What are the stages of Chronic obstructive pulmonary disease COPD?
One measure of Chronic obstructive pulmonary disease COPD is achieved by spirometry grading.
- There are various grading systems, and one grading system is part of the GOLD classification.
- The GOLD classification is used for determining Chronic obstructive pulmonary disease COPD severity and helping to form a prognosis and treatment plan.
There are 4 GOLD grades based on spirometry testing:
- grade 1: mild
- grade 2: moderate
- grade 3: severe
- grade 4: very severe
- This is based on the spirometry test result of your forced expiratory volume1 FEV1.
- This is the amount of air you can breathe out of the lungs in the 1st second of forced expiration.
- The severity increases as your forced expiratory volume1 FEV1 decreases.
- The GOLD classification also takes into account your personal symptoms & history of acute exacerbations.
- Based on this information, your doctor can assign a letter group to you to help define your Chronic obstructive pulmonary disease COPD grade.
As the disease progresses, you are more susceptible to complications, like as:
- respiratory infections, involving common colds, flu, and pneumonia
- heart problems
- high blood pressure (BP) in lung arteries (pulmonary hypertension)
- lung cancer
- depression & anxiety.
Is there a connection between Chronic obstructive pulmonary disease COPD & lung cancer?
- Chronic obstructive pulmonary disease COPD and lung cancer are major health problems worldwide.
- These 2 diseases are linked in a number of ways.
- Chronic obstructive pulmonary disease COPD and lung cancer have several common risk factors.
- Smoking is the number 1 risk factor for both diseases.
- Both are more likely if you breathe secondhand smoke, or are exposed to chemicals or another fume in the workplace.
- There may be a genetic predisposition to growing both diseases.
- Also, the risk of developing either Chronic obstructive pulmonary disease COPD or lung cancer increases with age.
- It was estimated in 2009 that between 40 and 70 percent trusted Source of people with lung cancer also have Chronic obstructive pulmonary disease COPD.
- In this same 2009 study trusted Sources concluded that Chronic obstructive pulmonary disease COPD is a risk factor for lung cancer.
- A 2015 study by trusted Sources suggests they may actually be different aspects of the same disease, and that Chronic obstructive pulmonary disease COPD could be a driving factor in lung cancer.
- In some cases, people do not learn they have Chronic obstructive pulmonary disease or COPD until they are diagnosed with lung cancer.
- However, having Chronic obstructive pulmonary disease and COPD does not necessarily mean you will get lung cancer.
- It does mean that you have a higher risk. That is another reason why, if you smoke, quitting is a good idea.
Chronic obstructive pulmonary disease COPD statistics
- Worldwide, it is estimated that about 65 million trusted Source people have moderate to severe Chronic obstructive pulmonary disease COPD.
- About 16 million trusted Source adults in the United States have a diagnosis of Chronic obstructive pulmonary disease COPD.
- Most people with Chronic obstructive pulmonary disease COPD are 40 years of age or older.
- The majority of people with Chronic obstructive pulmonary disease COPD are smokers or former smokers.
- Smoking is the most main risk factor that can be changed.
- In up to 5 percent trusted Source of people with Chronic obstructive pulmonary disease COPD, the cause is a genetic disorder involving a deficiency of a protein called alpha-1-antitrypsin.
- Chronic obstructive pulmonary disease COPD is a leading cause of hospitalizations in industrialized countries. In the United States, Chronic obstructive pulmonary disease COPD is responsible for a large number of emergency department visits and hospital admissions.
- In the year 2000, it was noted that there were over 700,000 hospital admissions to trusted Sources and approximately 1.5 million trusted Sources emergency department visits.
- Chronic obstructive pulmonary disease COPD is the third leading cause of death in the United States.
- More women than men die from Chronic obstructive pulmonary disease COPD each year.
- It is projected that the number of patients diagnosed with Chronic obstructive pulmonary disease COPD will increase by more than 150 percent from 2010 to 2030. Much of that can be assigned to an aging population.
What is the outlook for people with Chronic obstructive pulmonary disease COPD?
- Chronic obstructive pulmonary disease COPD generally reduces life expectancy, though the outlook varies considerably from person to person.
- People with Chronic obstructive pulmonary disease and COPD who never smoked may have a modest reduction in life expectancy rested Source, while former & current smokers are likely to have a larger reduction.
- Chronic obstructive pulmonary disease and COPD tend to progress slowly.
- You may not even realize you have it during the early stages.
- Once you have a diagnosis, you will need to start seeing your doctor on a regular basis.
- You will also have to take steps to manage your condition & make the appropriate changes to your daily life.
- Early symptoms can usually be managed, and certain lifestyle choices can assist you to maintain a good quality of life for some time.
- As the disease progresses, symptoms can increasingly be limiting.
- People with severe stages of Chronic obstructive pulmonary disease COPD may not be able to care for themselves without assistance.
- They are at increased risk of developing respiratory infections, heart problems, and lung cancer.
- They may be at risk of depression and anxiety.
- Besides smoking, your outlook depends on how healthy you respond to treatment and whether you can avoid serious complications.
- Your doctor is in a better position to evaluate your overall health & give you an idea about what to expect.
What is a chronic obstructive pulmonary disease COPD exacerbation?
- A person with chronic obstructive pulmonary disease (COPD) experiences long-term, & progressive harm to their lungs.
- This harms airflow to the lungs. Doctors often call this condition emphysema or chronic bronchitis.
- A person with chronic obstructive pulmonary disease COPD can experience a period when their symptoms are much worse than usual.
- This is known as an acute exacerbation.
- They may require to seek medical help at a hospital.
- The average person with chronic obstructive pulmonary disease COPD has between 0.85 and 1.3 exacerbations a year.
- chronic obstructive pulmonary disease COPD exacerbations can be harmful because they can cause further damage to the lungs.
- If you have been diagnosed with chronic obstructive pulmonary disease COPD, preventing an exacerbation from occurring can help you live a healthier life and reduce the risk of death.
What are the symptoms of chronic obstructive pulmonary disease and COPD exacerbation?
- If you have chronic obstructive pulmonary disease and COPD, physical activity will typically leave you short of breath. You may not be able to do all the activities that a person without chronic obstructive pulmonary disease COPD can do. During an exacerbation, your symptoms can get much poor than usual.
Examples of chronic obstructive pulmonary disease COPD exacerbation symptoms include:
- breathing in a fast & superficial pattern, as if you have just exercised very intensely
- coughing,
- experiencing shortness of breath at rest or with minimal activity, like walking from one room to another
- feeling excessively sleepy or confused
- having lower oxygen levels than normal
- noticing increasing amounts of mucus, which is sometimes yellow, green, tan, or even blood-tinged
- wheezing more than usual.
Which chronic obstructive pulmonary disease COPD exacerbation symptoms require emergency care?
- Later your body uses oxygen, carbon dioxide is left on the inside. Your lungs are responsible for exchanging oxygen with carbon dioxide (CO2).
- A person with chronic obstructive pulmonary disease and COPD has more difficulty making this exchange because their lungs do not work as well. This could guide to a buildup of carbon dioxide and reduced oxygen levels. If carbon dioxide (CO2) builds up in your body or oxygen levels become too low, it can become deadly.
Symptoms of too much carbon dioxide in your body involve:
- confusion
- severe headache
- difficulty walking even short distances
- having a hard time catching your breath
- If these symptoms occur, then it is important to seek immediate medical attention.
What causes chronic obstructive pulmonary disease COPD exacerbation?
- A chronic obstructive pulmonary disease COPD exacerbation is usually triggered by inflammation in the lungs.
- Infections or irritants can cause this inflammation.
Examples involve:
- pneumonia
- flu
- seasonal allergens
- air pollution
- smoke.
- If you have chronic obstructive pulmonary disease and COPD, it is important to take every step possible to avoid lung infection, such as getting flu shots annually. You will also require the pneumococcal vaccine.
- However, about 33 percent of chronic obstructive pulmonary disease COPD exacerbations do not have a known cause.
Can a chronic obstructive pulmonary disease COPD exacerbation cause other conditions to develop?
- Because chronic obstructive pulmonary disease COPD causes limited lung function, it can keep you from exercising or moving around as much.
- Limited lung function also constructs you more likely to get an infection. When you have chronic obstructive pulmonary disease COPD, getting a cold or the flu can be more dangerous & cause more severe symptoms.
Some of the known complications associated with chronic obstructive pulmonary disease COPD include:
- depression, as having chronic obstructive pulmonary disease COPD can affect your ability to do things you enjoy
- heart problems, like as heart disease and an increased risk of heart attack
- pulmonary arterial hypertension, or high blood pressure (BP) in the arteries of the lungs
- lung cancer, as those with chronic obstructive pulmonary disease COPD often were or are smokers.
How are chronic obstructive pulmonary disease COPD exacerbations treated?
- Treatments for chronic obstructive pulmonary disease and COPD exacerbations can depend on the severity of your symptoms.
- Most people with chronic obstructive pulmonary disease COPD will start to notice a pattern in their symptoms. If you notice the symptoms of an exacerbation coming on early enough, you can get treatment previous your symptoms worsen.
Home treatments
- If your symptoms are not severe, your doctor may prescribe treatments for you to use at home.
Examples of these involve:
- Antibiotics: If bacteria caused your respiratory infection, taking antibiotics can assist to slow the infection or stop it from getting worse.
- Inhalers: When the little, treelike parts of your lungs known as alveoli get narrow or fill with mucus, it is harder to breathe. There are two types of inhalers: bronchodilators & steroid inhalers. Bronchodilators inhalers: These inhalers help to open the airways and make it easier to breathe. Examples involve ipratropium/albuterol (Combivent Respimat) & levalbuterol (Xopenex). Steroid inhalers: These inhalers decrease lung inflammation and are sometimes combined, such as fluticasone/salmeterol (Advair).
- Steroids: These medications are designed to reduce lung inflammation, which leads to the narrowing of and swelling in the airways. Methylprednisolone (Medrol) is one example.
Emergency treatments
- At a hospital, your doctor may supply additional treatments to support your breathing. One example is the use of continuous positive airway pressure (CPAP) devices to help keep your lungs open.
- Your doctor may also put you on a ventilator to assist you to breathe. In this case, you will stay in an intensive care unit until your infection clears up or your lungs become less inflamed.
Can chronic obstructive pulmonary disease COPD exacerbation be prevented?
- You can help prevent chronic obstructive pulmonary disease and COPD exacerbations by adopting certain self-care practices.
These involve:
- avoiding exposure to lung irritants, like kerosene heaters, in your home,
- avoiding huge crowds during cold and flu season to prevent getting sick
- drinking plenty of fluids to cure mucus from becoming too thick
- getting the yearly flu shot to cure the respiratory infection
- keeping regular appointments with your healthcare provider, like your pulmonologist
- monitoring your oxygen levels whenever possible, possibly with the health of a tiny device called a pulse oximeter
- practicing healthy habits, like getting enough sleep at night and eating a healthy diet
- getting pneumonia or pertussis shot when your healthcare provider recommends it
- quitting smoking or avoiding secondhand smoke
- washing your hands frequently and using hand sanitizer to cure the spread of germs.
What is the outlook for people with chronic obstructive pulmonary disease and COPD exacerbations?
- Doctors classify chronic obstructive pulmonary disease COPD into four stages, from Group A to Group D.
- Group A has fewer symptoms and a low risk of exacerbations, while Group D has more symptoms & higher risk of exacerbations.
- Because the condition is chronic, you may progress throughout each of the stages.
- However, this commonly occurs over many years.
- These exacerbations can be deadly.
- If your lungs are functioning badly, you might not be able to breathe without a ventilator.
- It is also possible that a ventilator may not provide enough support for your lungs.
- Preventive self-care measures like the ones mentioned earlier can decrease the likelihood of an exacerbation.
- Ask your doctor about additional steps you can take to prevent chronic obstructive pulmonary disease and COPD exacerbations.




20 Comments